血清肌酐与胱抑素C比值(CCR)对HBV相关慢加急性肝衰竭预后的评估价值
DOI: 10.12449/JCH240208
Value of serum creatinine-to-cystatin C ratio in assessing the prognosis of hepatitis B virus-related acute-on-chronic liver failure
-
摘要:
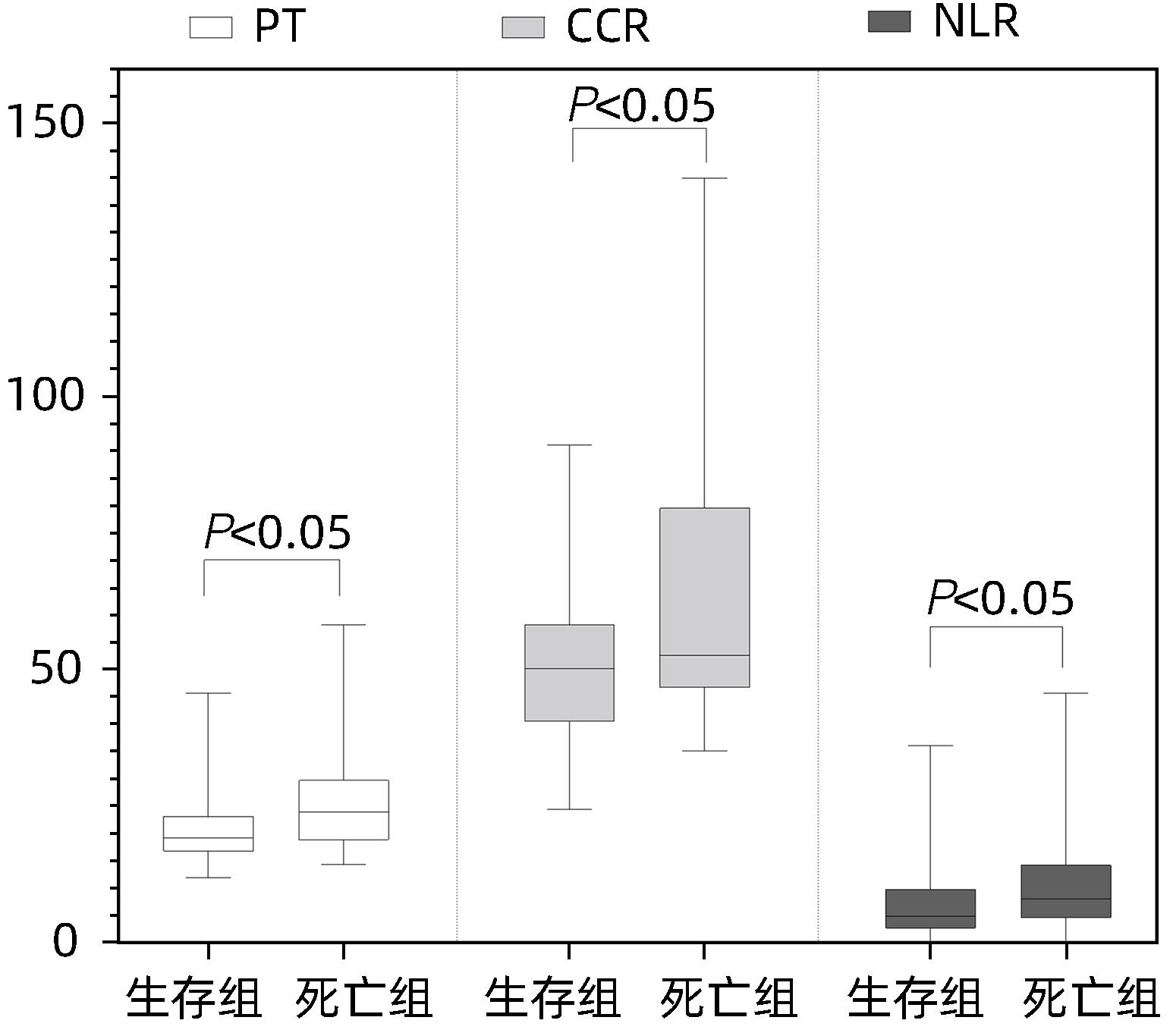
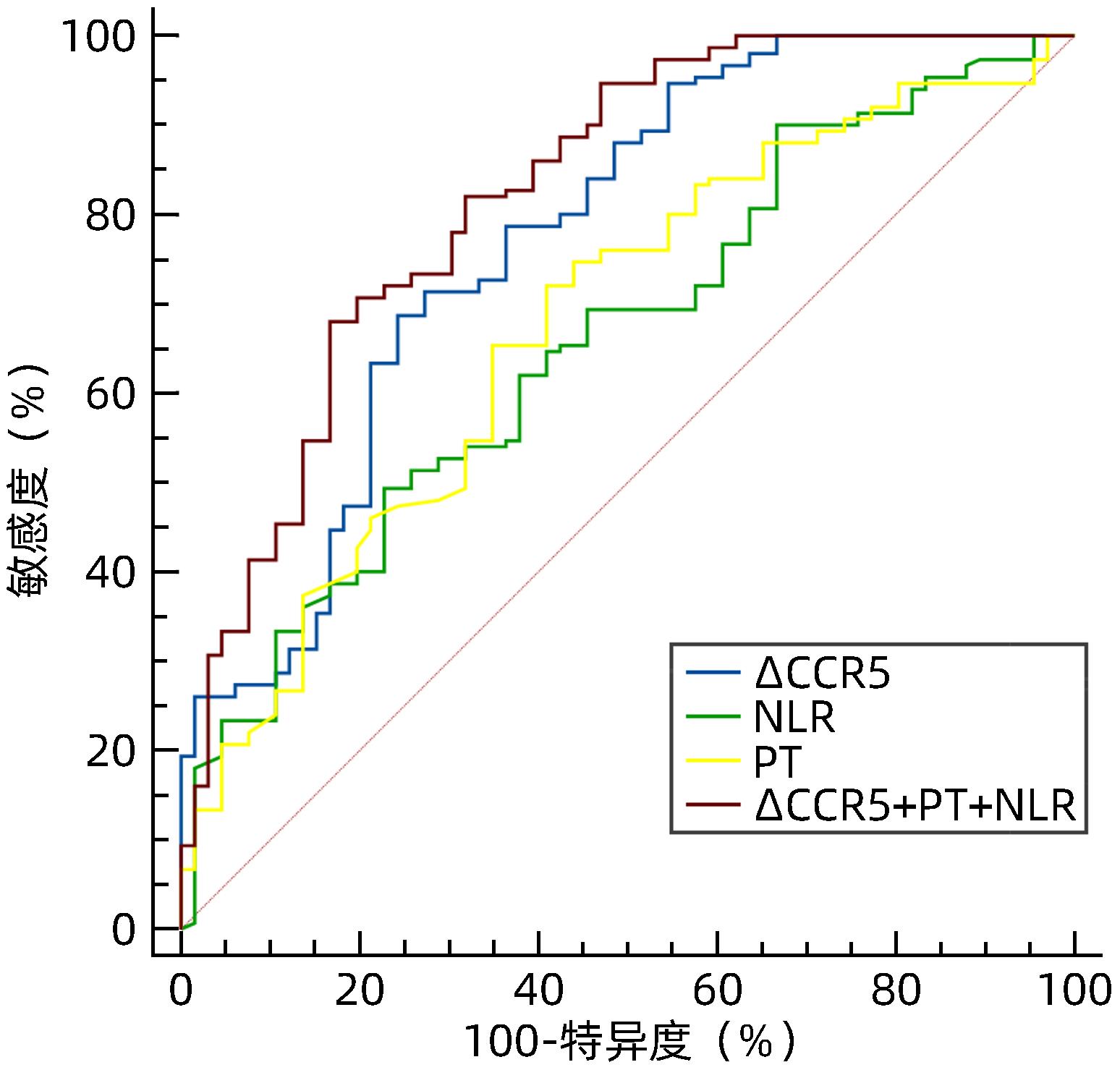
目的 探讨血清肌酐与胱抑素C比值(CCR)评估HBV相关慢加急性肝衰竭(HBV-ACLF)预后的临床价值。 方法 回顾性分析2021年1月—2022年11月苏州大学附属第一医院感染病科住院治疗的130例HBV-ACLF患者(治疗组)临床资料,根据治疗结局分为生存组(n=87)和死亡组(n=43);根据是否合并感染,分为感染组(n=37)和非感染组(n=93)。以同期30例健康体检者作为对照组。收集入院当天血常规指标,包括白细胞、血小板、中性粒细胞和淋巴细胞计数;观察入院当天、住院第5天、第10天、第15天血清肌酐、胱抑素C、血清Alb、PT,计算CCR、中性粒细胞与淋巴细胞比值(NLR)、血小板与淋巴细胞比值(PLR)、营养指数(PNI)、CCR5(入院后第5天CCR)、ΔCCR5(入院后第5天CCR-入院当天CCR)、CCR10(入院后第10天CCR)、ΔCCR10(入院后第10天CCR-入院后第5天CCR)、CCR15(入院后第15天CCR)、ΔCCR15(入院后第15天CCR-入院后第10天CCR),比较生存组和死亡组、感染组与非感染组上述指标的差异。计量资料两组间比较采用Mann-Whitney U检验;多组间比较采用Kruskal-Wallis H检验。单因素和多因素Logistic回归分析探讨影响疾病预后的因素;受试者工作特征曲线(ROC曲线)评估CCR对HBV-ACLF死亡事件的预测价值,ROC曲线下面积(AUC)比较采用DeLong检验。 结果 治疗组基线CCR、NLR、PNI、PT和Alb与健康对照组比较,差异均有统计学意义(P值均<0.001)。生存组与死亡组患者入院当天CCR、NLR、PT比较,差异均有统计学意义(P值均<0.05)。在130例HBV-ACLF患者中,有25例处于前期,48例处于早期,32例处于中期,25例处于晚期。各分期HBV-ACLF患者基线CCR、PLR及PT比较,差异均有统计学意义(P值均<0.05)。感染组与非感染组患者基线ΔCCR5、NLR比较,差异均有统计学意义(P值均<0.05)。患者入院第5天、第10天、第15天生存组与死亡组ΔCCR5、CCR10、CCR15比较,差异均有统计学意义(P值均<0.05)。多因素Logistic回归分析发现ΔCCR5(OR=1.175,95%CI:1.098~1.256,P<0.001)、NLR(OR=0.921,95%CI:0.880~0.964,P<0.001)和PT(OR=0.921,95%CI:0.873~0.973,P=0.003)是HBV-ACLF患者预后的独立影响因素。ΔCCR5的AUC为0.774,敏感度为0.687,特异度为0.757;ΔCCR5+PT+NLR联合的AUC为0.824,高于ΔCCR5、NLR、PT单独预测时的AUC(P值均<0.05)。 结论 ΔCCR5、NLR、PT可反映HBV-ACLF患者的病情及预后,是HBV-ACLF患者死亡事件的独立预测指标,ΔCCR5+PT+NLR联合时预测效能最佳。 -
关键词:
- 乙型肝炎病毒 /
- 慢加急性肝功能衰竭 /
- 肌酸酐 /
- 半胱氨酸蛋白酶抑制物C /
- 预后
Abstract:Objective To investigate the clinical value of serum creatinine-to-cystatin C ratio (CCR) in evaluating the prognosis of hepatitis B virus-related acute-on-chronic liver failure (HBV-ACLF). Methods A retrospective analysis was performed for the clinical data of 130 patients with HBV-ACLF (treatment group) who were hospitalized in Department of Infectious Diseases, The First Affiliated Hospital of Soochow University, from January 2021 to November 2022. According to the treatment outcome, they were divided into survival group with 87 patients and death group with 43 patients; according to the presence or absence of infection, they were divided into infection group with 37 patients and non-infection group with 93 patients. A total of 30 individuals who underwent physical examination during the same period of time were enrolled as control group. Routine blood test results were collected on the day of admission, including white blood cell count, platelet count, neutrophil count, and lymphocyte count; serum creatinine, cystatin C, serum albumin (Alb), and prothrombin time (PT) were observed on the day of admission and on days 5, 10, and 15 of hospitalization, and related indicators were calculated, including CCR, neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), prognostic nutritional index (PNI), CCR5 (CCR on day 5 after admission), ΔCCR5 (CCR on day 5 after admission minus CCR on the day of admission), CCR10 (CCR on day 10 after admission), ΔCCR10 (CCR on day 10 after admission minus CCR on day 5 after admission), CCR15 (CCR on day 15 after admission), and ΔCCR15 (CCR on day 15 after admission minus CCR on day 10 after admission). The above indicators were compared between the survival group and the death group and between the infection group and the non-infection group. The Mann-Whitney U test was used for comparison of continuous data between two groups, and the Kruskal-Wallis H test was used for comparison between multiple groups. The univariate and multivariate logistic regression analyses were used to investigate the influencing factors for disease prognosis; the receiver operating characteristic (ROC) curve was used to assess the value of CCR in predicting HBV-ACLF death events, and the DeLong test was used for comparison of the area under the ROC curve (AUC). Results There were significant differences in CCR, NLR, PNI, PT, and Alb at baseline between the treatment group and the healthy control group (all P<0.001), and there were significant differences in CCR, NLR, and PT between the survival group and the death group on the day of admission (all P<0.05). Among the 130 patients with HBV-ACLF, there were 25 in the precancerous stage, 48 in the early stage, 32 in the intermediate stage, and 25 in the advanced stage, and there were significant differences in baseline CCR, PLR, and PT between the patients in different stages of HBV-ACLF (all P<0.05). There were significant differences in ΔCCR5 and NLR between the infection group and the non-infection group (P<0.05), and there were significant differences in ΔCCR5, CCR10, and CCR15 between the survival group and the death group (all P<0.05). The multivariate logistic regression analysis showed that ΔCCR5 (odds ratio [OR]=1.175, 95% confidence interval [CI]: 1.098 — 1.256, P<0.001), NLR (OR=0.921, 95%CI: 0.880 — 0.964, P<0.001), and PT (OR=0.921, 95%CI: 0.873 — 0.973, P=0.003) were independent influencing factors for the prognosis of HBV-ACLF patients. ΔCCR5 had an AUC of 0.774, a sensitivity of 0.687, and a specificity of 0.757, and the AUC of ΔCCR5+PT+NLR was 0.824, which was significantly higher than the AUC of ΔCCR5, NLR, or PT alone (all P<0.05). Conclusion ΔCCR5, NLR, and PT can reflect the condition and prognosis of patients with HBV-ACLF and are independent predictive indicators for death events in patients with HBV-ACLF. The combination ofΔCCR5, PT, and NLR has the best predictive efficiency. -
Key words:
- Hepatitis B Virus /
- Acute-On-Chronic Liver Failure /
- Creatinine /
- Cystatin C /
- Prognosis
-
临床上,胰腺恶性肿瘤大部分为原发肿瘤,胰腺转移癌少见[1]。胰腺转移癌与胰腺原发肿瘤鉴别困难,极易造成误诊,延误治疗。目前,胰腺转移癌国内外尚无统一治疗标准,原发肿瘤的生物学特性和针对原发肿瘤的综合治疗是决定其预后的主要因素,个体化差异较大。近期,笔者接诊1例宫颈鳞癌胰腺转移患者,现将病例资料及经验总结报告如下。
1. 病例资料
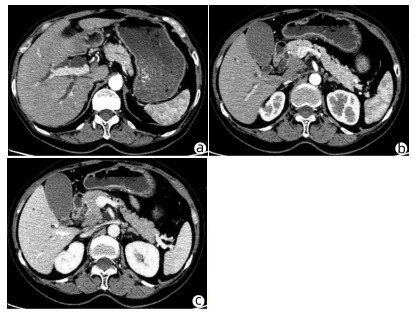
患者女性,63岁,因“皮肤、巩膜黄染20余天”于2021年3月27日入本院。起初黄染程度不重,后进行性加重,无腹痛腹胀,无阴道流血等其他不适。曾于2013年9月6日因阴道异常流血于外院行宫颈活检,病理学诊断为宫颈中分化鳞癌ⅢB期,予局部放疗联合TP方案(多西他赛+奥沙利铂)化疗,于2015年结束治疗后复查腹盆腔脏器、腹腔、盆腔均未见肿瘤转移。出院后患者再未复查,亦无特殊不适。入院查体:皮肤巩膜明显黄染,腹平坦,腹部无压痛,腹部未触及肿块。辅助检查:TBil 282.99 μmol/L,DBil 203.80 μmol/L,CA19-9正常;妇科彩超示:老年性子宫;全腹盆腔增强CT示:肝内外胆管扩张,主胰管可见(图 1a),胆囊明显增大,胆总管下段狭窄,动脉期见胰腺钩突区低密度肿块(图 1b),静脉期肿块轻度强化(图 1c),子宫显示不明显,腹膜后可见多发淋巴结肿大;磁共振胰胆管造影示:胰头区异常信号肿块,肝内外胆管扩张,胆汁淤积;超声内镜示:胰头钩突区占位,直径约3 cm。入院后予以护肝利胆治疗,患者黄疸进行性加重,建议患者行穿刺活检、PET-CT检查,患方拒绝。2021年4月4日行剖腹探查:术中探查发现肿瘤位于胰头钩突区,质地硬,侵犯十二指肠壁和胆总管,腹膜后见多发淋巴结肿大,行胰头十二指肠切除术。术后病理学检查结果:胰腺钩突肿块大小3.0 cm×2.0 cm×1.5 cm,癌组织侵犯十二指肠及胆总管,胰腺切缘未见癌。癌组织呈团块状或条索状癌巢(图 2a),癌细胞及核大小、形态不一,分布不规则,核分裂像多见,癌组织侵犯淋巴管及血管,脉管内见癌栓(图 2b),周围淋巴结可见癌转移(2/2)。免疫组化:P16(弥漫性+),P63(+),P40(+),CK7(+),CK8(+),CK19(+),ER(+)(图 2c、d)。诊断考虑胰腺钩突区中分化鳞状细胞癌,结合临床病史及免疫组化结果,考虑宫颈鳞癌转移。目前,该患者于本院进一步针对原发肿瘤行化疗等综合治疗,日常生活行为已恢复正常。
2. 讨论
据统计,宫颈癌的患病/病死率在女性恶性肿瘤中居第4位,鳞状细胞癌是最常见的病理类型,占比约80%,P16、P40等表达阳性对宫颈鳞癌诊断有重要意义。宫颈鳞癌早期往往无特殊表现,晚期可出现异常阴道流血、腰痛、盆腔痛、性交痛、贫血等表现,诊断时大多发生转移,多转移至直肠、膀胱、盆腔、肺、骨、肝等。临床上,胰腺癌多为原发肿瘤,胰腺转移癌罕见,仅占胰腺恶性肿瘤总数的2%~3%[2]。在一项纳入973例胰腺肿瘤手术标本病理资料的研究[3]中,共38例为胰腺转移瘤,主要包括淋巴瘤11例,胃癌7例,肾癌6例,肺癌2例,肝癌、前列腺癌、卵巢癌、子宫癌各1例,默克尔细胞癌1例,另有3例胃肠道恶性间质瘤和1例腹膜后平滑肌肉瘤;81例转移性胰腺肿瘤尸检报告显示,主要来源肺癌34例,胃肠道20例,肾脏4例,乳腺3例,肝脏2例,卵巢和膀胱各1例,另有6例来自造血系统,黑色素瘤、肉瘤和间皮瘤各2例。来源于宫颈的胰腺转移癌并不多见,笔者在国内外文献检索系统中,共检出各类型宫颈癌胰腺转移病例报告10例[4-7],其中鳞癌3例,神经内分泌癌5例,腺癌2例;转移灶位于胰头3例,位于颈部1例,位于胰腺体部3例,位于尾部、体尾部和胰头及体尾部各1例。转移灶位于胰头的3例患者中,1例为鳞癌,2例为神经内分泌癌,胰腺转移部位与宫颈癌病理类型无明显关联。本例患者在宫颈鳞癌同步放化疗后再未复查,6年后转移至胰腺钩突,临床表现为梗阻性黄疸,行胰头十二指肠切除术,术后病理学检查考虑鳞癌,结合免疫组化考虑为宫颈癌来源。目前,国内尚未见类似报道,国外也鲜有相关报道。
原发性胰腺癌与胰腺转移癌鉴别需依赖血清CA19-9水平、CT、MRI、磁共振胰胆管造影、内镜逆行胰胆管造影、超声内镜等检查手段。本例患者CT和MRI特点较原发性胰腺癌无特异表现,鉴别困难。血清CA19-9水平升高常见于胆道、胰腺恶性肿瘤,对诊断原发性胰腺癌有较高的敏感度和特异度[8]。鉴别困难时,可采用通过超声、CT及内镜引导下穿刺活检获取胰腺组织学、细胞学标本进行确诊,但需要评估穿刺活检的出血风险[9]。一般认为,超声内镜经十二指肠细针穿刺抽吸活检可提高胰腺疾病诊断的准确性,且相对安全[10-11]。本例患者术前影像学检查提示胰头钩突区占位,CA19-9水平不高,且有宫颈鳞癌病史,建议进一步行穿刺活检、PET-CT检查。但患者存在梗阻性黄疸,肝功能持续恶化,有手术指征,且患者家属不同意术前行穿刺活检、PET-CT等进一步检查,因此术前未能获得病理学诊断。
转移性胰腺癌临床表现因胰腺转移部位不同而异。在笔者检出的10例报告中,仅有1例(鳞癌)出现梗阻性黄疸,提示宫颈癌胰腺转移鲜有梗阻性黄疸症状,部分病例可因肿瘤压迫出现胆胰管扩张。转移性胰腺癌出现胰胆管梗阻较少见,可能与原发肿瘤主要经过淋巴及血行途径转移侵犯胰腺,不侵犯胆胰管有关[12]。本例患者胰腺转移性肿瘤致梗阻性黄疸,目前国内尚未见类似报道,国外仅有1例类似报道,但未分析相关转移机制。本例患者影像学检查示肝、胃、肠道等器官均未见肿瘤,但有腹膜后淋巴结肿大,病理学检查阳性;在既往10例报告中,3例胰腺转移性宫颈鳞癌有2例伴腹膜后淋巴结肿大,因此笔者推测宫颈鳞癌胰腺转移可能与腹膜后淋巴结侵犯相关。
关于转移性胰腺癌是否需要手术,意见尚未统一。以急腹症、进行性黄疸、出血为临床表现患者,应行急诊手术治疗,解除症状同时,切除病灶送检,根据病理学检查结果制订综合治疗方案。研究[13-14]表明,转移性胰腺癌行手术切除相较于保守治疗可延长生存期,且根治性手术相较于姑息性手术,预后更好。术后根据原发病灶辅以化疗等综合治疗,可提高治疗效果。对无法接受手术的转移性胰腺癌患者,应根据原发肿瘤的生物学特性制订以放疗为主的个体化综合治疗方案[15]。本例患者影像学检查提示存在胆道梗阻,并见胰头钩突区占位;胆红素水平持续升高,手术指征明确,手术切除胰腺钩突病灶、解除胆道梗阻后,胆红素水平明显下降,目前患者恢复良好,进一步接受化疗等综合治疗,延长生存期。
笔者经验总结:(1)对于诊断不明确的胰腺肿瘤,术前条件允许情况下需行穿刺活检明确性质,以指导下一步治疗方案;(2)胰腺转移癌在具备手术条件情况下,应积极采取以根治性手术为主的治疗方案,姑息性切除方案亦可行。胰腺转移癌为晚期癌症,术后需早期予以放化疗、靶向、免疫治疗等综合治疗;(3)对于不具备手术条件的患者,需根据原发肿瘤予以抗肿瘤综合治疗,包括放疗、化疗以及免疫治疗、靶向治疗等[16-17]。
-
表 1 治疗组与健康对照组基线指标比较
Table 1. Comparison of baseline indexes between the treatment group and the healthy control group
指标 健康对照组(n=30) 治疗组(n=130) Z值 P值 男/女(例) 15/15 78/52 χ2=-1.233 0.190 年龄(岁) 52(47~76) 53(42~66) Z=-0.638 0.524 CCR(μmol/mg) 74.67(64.54~83.18) 51.22(43.35~62.33) Z=-6.378 <0.001 NLR 1.88(1.35~2.24) 5.81(2.89~11.11) Z=-6.745 <0.001 PLR 109.00(88.54~123.89) 96.77(57.38~146.99) Z=-1.437 0.151 PNI 51.80(49.34~54.80) 34.50(30.70~38.10) Z=-8.418 <0.001 PT(s) 10.90(10.38~11.75) 19.70(17.60~25.80) Z=-8.881 <0.001 Alb(g/L) 42.90(41.08~44.30) 29.10(26.53~32.60) Z=-8.746 <0.001 表 2 HBV-ACLF患者不同分期基线指标比较
Table 2. Baseline markers of HBV-ACLF at different stages were compared
指标 前期(n=25) 早期(n=48) 中期(n=32) 晚期(n=25) H值 P值 CCR(μmol/mg) 43.85(38.01~53.55) 53.01(43.18~64) 51.69(44.95~60.57) 56.84(46.43~80.44) 19.816 <0.001 NLR 5.70(2.38~10.69) 6.58(3.43~12.38) 5.55(2.80~10.45) 7.64(2.77~11.25) 2.070 0.558 PLR 77.38(52.27~140.63) 106.96(65.79~188.73) 69.44(50.18~143.86) 78.21(54.02~120.69) 13.698 0.003 PNI 32.65(30.60~37.25) 34.55(30.50~38.85) 33.90(29.35~37.65) 36.25(32.35~39.55) 5.949 0.114 PT(s) 17.60(16.25~19.05) 18.20(16.20~19.50) 24.00(22.50~26.05) 33.10(30.30~41.00) 187.731 <0.001 Alb(g/L) 28.70(26.20~30.50) 28.80(26.40~32.70) 29.10(26.10~32.90) 29.80(28.00~33.20) 3.285 0.350 表 3 非感染组与感染组基线指标比较
Table 3. Comparison of baseline indexes between infected group and non-infected group
指标 感染组(n=37) 非感染组(n=93) Z值 P值 CCR(μmol/mg) 54.17(40.49~66.08) 50.74(43.78~62.33) -1.098 0.272 NLR 12.38(7.64~16.29) 4.65(2.70~7.98) -6.363 <0.001 PLR 107.53(57.86~168.42) 93.18(60.34~145.16) -0.414 0.679 PNI 35.65(31.20~38.65) 34.20(30.50~37.80) -0.630 0.529 PT(s) 18.60(16.60~24.75) 20.30(17.50~25.10) -0.623 0.533 Alb(g/L) 28.70(25.25~32.40) 29.10(26.70~32.30) -0.416 0.678 ΔCCR5(μmol/mg) -13.94(-22.19~-5.48) -9.41(-13.40~-5.04) -2.675 0.007 表 4 死亡组与生存组患者入院第5天、第10天、第15天CCR动态比较
Table 4. Dynamic comparison of CCR in death group and survival group at 5、10 and 15 days after admission
指标 死亡组(n=43) 生存组(n=87) Z值 P值 CCR5(μmol/mg) 39.70(32.32~46.86) 40.80(37.00~49.37) -0.360 0.719 ΔCCR5(μmol/mg) -18.43(-70.19~-13.40) -9.41(-11.25~-3.49) -5.380 <0.001 CCR10(μmol/mg) 40.00(1.82~44.62) 39.32(33.65~49.04) -2.410 0.016 ΔCCR10(μmol/mg) -4.89(-32.44~-0.69) -3.44(-5.56~1.47) -1.674 0.094 CCR15(μmol/mg) 27.84(24.69~34.43) 37.60(31.64~46.86) -3.480 <0.001 ΔCCR15(μmol/mg) -7.55(-12.16~22.87) -2.64(-7.49~2.09) -1.323 0.186 表 5 基线指标单因素及多因素Logistic回归分析
Table 5. The baseline indexes were analyzed by binary single factor and multivariate Logistic regression
指标 单因素分析 多因素分析 OR(95%CI) P值 OR(95%CI) P值 ΔCCR5(μmol/mg) 1.163(1.101~1.228) <0.001 1.175(1.098~1.256) <0.001 PT(s) 0.912(0.876~0.950) <0.001 0.921(0.873~0.973) 0.003 NLR 0.948(0.917~0.980) 0.001 0.921(0.880~0.964) <0.001 CCR(μmol/mg) 0.959(0.943~0.976) <0.001 1.006(0.976~1.036) 0.713 PLR 1.003(0.999~1.007) 0.191 PNI 0.997(0.976~1.018) 0.780 Alb(g/L) 0.993(0.937~1.051) 0.798 表 6 ΔCCR5、PT、NLR、ΔCCR5+PT+NLR预测HBV-ACLF患者死亡事件效能分析
Table 6. Efficacy analysis of ΔCCR5, PT, NLR, ΔCCR5+PT+NLR in predicting death events in patients with HBV-ACLF
变量 AUC 95%CI P值 最佳临界值 敏感度 特异度 约登指数 PT(s) 0.704 0.643~0.761 <0.001 21.500 0.710 0.650 0.360 NLR 0.645 0.581~0.705 <0.001 4.610 0.481 0.762 0.244 ∆CCR5(μmol/mg) 0.774 0.712~0.828 <0.001 -10.150 0.687 0.757 0.444 ∆CCR5+PT+NLR 0.824 0.767~0.873 <0.001 0.700 0.680 0.833 0.513 -
[1] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association. Clinical guidelines on nutrition in end-stage liver disease[J]. J Clin Hepatol, 2019, 35( 6): 1222- 1230. DOI: 10.3969/j.issn.1001-5256.2019.06.010.中华医学会肝病学分会, 中华医学会消化病学分会. 终末期肝病临床营养指南[J]. 临床肝胆病杂志, 2019, 35( 6): 1222- 1230. DOI: 10.3969/j.issn.1001-5256.2019.06.010. [2] MANGANA DEL RIO T, SACLEUX SC, VIONNET J, et al. Body composition and short-term mortality in patients critically ill with acute-on-chronic liver failure[J]. JHEP Rep, 2023, 5( 8): 100758. DOI: 10.1016/j.jhepr.2023.100758. [3] NISHIKAWA H, SHIRAKI M, HIRAMATSU A, et al. Japan Society of Hepatology guidelines for sarcopenia in liver disease(1st edition): Recommendation from the working group for creation of sarcopenia assessment criteria[J]. Hepatol Res, 2016, 46( 10): 951- 963. DOI: 10.1111/hepr.12774. [4] PENG H, ZHANG Q, LUO L, et al. A prognostic model of acute-on-chronic liver failure based on sarcopenia[J]. Hepatol Int, 2022, 16( 4): 964- 972. DOI: 10.1007/s12072-022-10363-2. [5] SANCHEZ-RODRIGUEZ D, MARCO E, CRUZ-JENTOFT AJ. Defining sarcopenia: Some caveats and challenges[J]. Curr Opin Clin Nutr Metab Care, 2020, 23( 2): 127- 132. DOI: 10.1097/MCO.0000000000000621. [6] SAYER AA, CRUZ-JENTOFT A. Sarcopenia definition, diagnosis and treatment: Consensus is growing[J]. Age Ageing, 2022, 51( 10): afac220. DOI: 10.1093/ageing/afac220. [7] KASHANI KB, FRAZEE EN, KUKRÁLOVÁ L, et al. Evaluating muscle mass by using markers of kidney function: Development of the sarcopenia index[J]. Crit Care Med, 2017, 45( 1): e23- e29. DOI: 10.1097/CCM.0000000000002013. [8] WANG S, XIE L, XU J, et al. Predictive value of serum creatinine/cystatin C in neurocritically ill patients[J]. Brain Behav, 2019, 9( 12): e01462. DOI: 10.1002/brb3.1462. [9] JUNG CY, KIM HW, HAN SH, et al. Creatinine-cystatin C ratio and mortality in cancer patients: A retrospective cohort study[J]. J Cachexia Sarcopenia Muscle, 2022, 13( 4): 2064- 2072. DOI: 10.1002/jcsm.13006. [10] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [11] LI JQ, LIANG X, YOU SL, et al. Development and validation of a new prognostic score for hepatitis B virus-related acute-on-chronic liver failure[J]. J Hepatol, 2021, 75( 5): 1104- 1115. DOI: 10.1016/j.jhep.2021.05.026. [12] GAO FY, ZHANG QQ, LIU Y, et al. Nomogram prediction of individual prognosis of patients with acute-on-chronic hepatitis B liver failure[J]. Dig Liver Dis, 2019, 51( 3): 425- 433. DOI: 10.1016/j.dld.2018.08.023. [13] SUN ZY, LIU XL, WU DX, et al. Circulating proteomic panels for diagnosis and risk stratification of acute-on-chronic liver failure in patients with viral hepatitis B[J]. Theranostics, 2019, 9( 4): 1200- 1214. DOI: 10.7150/thno.31991. [14] BEER L, BASTATI N, BA-SSALAMAH A, et al. MRI-defined sarcopenia predicts mortality in patients with chronic liver disease[J]. Liver Int, 2020, 40( 11): 2797- 2807. DOI: 10.1111/liv.14648. [15] JIN L, LI X. MRI-defined sarcopenia predicts mortality in patients with chronic liver disease[J]. Liver Int, 2021, 41( 1): 223. DOI: 10.1111/liv.14691. [16] WANG T, ZHANG YG, LI QQ, et al. Evaluation value of area index of the third lumbar psoas major muscle in nutritional status and prognosis of patients with cirrhosis[J]. Clin J Med Offic, 2022, 50( 7): 729- 732. DOI: 10.16680/j.1671-3826.2022.07.18.王然, 张永国, 李谦谦, 等. 第三腰椎腰大肌面积指数对肝硬化患者营养状态及预后评估价值[J]. 临床军医杂志, 2022, 50( 7): 729- 732. DOI: 10.16680/j.1671-3826.2022.07.18. [17] Society of Infectious Diseases, Chinese Medical Association. Expert consensus on diagnosis and treatment of end-stage liver disease complicated with infections(2021 version)[J]. J Clin Hepatol, 2022, 38( 2): 304- 310. DOI: 10.3969/j.issn.1001-5256.2022.02.010.中华医学会感染病学分会. 终末期肝病合并感染诊治专家共识(2021年版)[J]. 临床肝胆病杂志, 2022, 38( 2): 304- 310. DOI: 10.3969/j.issn.1001-5256.2022.02.010. [18] WANG XB, ZHANG Q, GAO FY. Prediction of acute-on-chronic liver failure and integrated traditional Chinese and Western medicine therapy[J]. J Clin Hepatol, 2020, 36( 1): 19- 25. DOI: 10.3969/j.issn.1001-5256.2020.01.003.王宪波, 张群, 高方媛. 慢加急性肝衰竭的预后评估及中西医结合治疗[J]. 临床肝胆病杂志, 2020, 36( 1): 19- 25. DOI: 10.3969/j.issn.1001-5256.2020.01.003. [19] HAINES RW, ZOLFAGHARI P, WAN Y, et al. Elevated urea-to-creatinine ratio provides a biochemical signature of muscle catabolism and persistent critical illness after major trauma[J]. Intensive care medicine, 2019, 45( 12): 1718- 1731. DOI: 10.1007/s00134-019-05760-5. [20] PAGE A, FLOWER L, PROWLE J, et al. Novel methods to identify and measure catabolism[J]. Curr Opin Crit Care, 2021, 27( 4): 361- 366. DOI: 10.1097/MCC.0000000000000842. [21] VERHAMME FM, FREEMAN CM, BRUSSELLE GG, et al. GDF-15 in pulmonary and critical care medicine[J]. Am J Respir Cell Mol Biol, 2019, 60( 6): 621- 628. DOI: 10.1165/rcmb.2018-0379TR. [22] LEE ES, KIM SH, KIM HJ, et al. Growth differentiation factor 15 predicts chronic liver disease severity[J]. Gut Liver, 2017, 11( 2): 276- 282. DOI: 10.5009/gnl16049. [23] ZHANG IW, CURTO A, LÓPEZ-VICARIO C, et al. Mitochondrial dysfunction governs immunometabolism in leukocytes of patients with acute-on-chronic liver failure[J]. J Hepatol, 2022, 76( 1): 93- 106. DOI: 10.1016/j.jhep.2021.08.009. [24] WEINERT LS, CAMARGO EG, SOARES AA, et al. Glomerular filtration rate estimation: Performance of serum cystatin C-based prediction equations[J]. Clin Chem Lab Med, 2011, 49( 11): 1761- 1771. DOI: 10.1515/CCLM.2011.670. [25] EINHORN D, MENDE CW. Combining creatinine-based EGFR with cystatin C-based EGFR to better assess renal function in patients with diabetes and chronic kidney disease 3a: Implications for drug selection and dosage in type 2 diabetes[J]. Endocr Pract, 2015, 21( 11): 1301- 1302. DOI: 10.4158/EP15821.ED. [26] CHEN XY, SHEN YJ, HOU LS, et al. Sarcopenia index based on serum creatinine and cystatin C predicts the risk of postoperative complications following hip fracture surgery in older adults[J]. BMC Geriatr, 2021, 21( 1): 541. DOI: 10.1186/s12877-021-02522-1. [27] ULMANN G, KAÏ J, DURAND JP, et al. Creatinine-to-cystatin C ratio and bioelectrical impedance analysis for the assessement of low lean body mass in cancer patients: Comparison to L3-computed tomography scan[J]. Nutrition, 2021, 81: 110895. DOI: 10.1016/j.nut.2020.110895. [28] ZHENG C, WANG E, LI JS, et al. Serum creatinine/cystatin C ratio as a screening tool for sarcopenia and prognostic indicator for patients with esophageal cancer[J]. BMC Geriatr, 2022, 22( 1): 207. DOI: 10.1186/s12877-022-02925-8. [29] SUN J, YANG H, CAI WT, et al. Serum creatinine/cystatin C ratio as a surrogate marker for sarcopenia in patients with gastric cancer[J]. BMC Gastroenterol, 2022, 22( 1): 26. DOI: 10.1186/s12876-022-02093-4. 期刊类型引用(1)
1. 李帅,王娟,夏仕雪,顾鹏. 子宫颈混合性腺神经内分泌癌胰腺转移1例. 中国医学影像学杂志. 2022(12): 1283-1284 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 799 KB)
PDF下载 ( 799 KB)


 下载:
下载:

 下载:
下载:
 百度学术
百度学术