胆囊切除术后原发性胆总管结石复发患者的临床特征分析
DOI: 10.12449/JCH250118
Clinical features of patients with recurrent primary common bile duct stones after cholecystectomy
-
摘要:
目的 分析原发性胆总管结石复发患者的总体情况、膳食因素等临床特征,为积极预防结石复发提供依据。 方法 回顾性收集2013年1月—2023年12月内蒙古自治区人民医院肝胆胰脾外科因胆石病行胆囊切除治疗的23 730例患者临床资料,其中术后复发334例。按性别分类,对复发患者的复发率、复发周期、复发年龄、复发结石类别,以及一般资料、疾病资料、影像学资料和膳食因素资料进行汇总分析。计量资料2组间比较采用成组t检验,计数资料2组间比较采用χ2检验。 结果 胆囊切除术后原发性胆总管结石复发率为1.41%,复发周期频数最高集中在术后10年,男、女性复发周期差异有统计学意义(t=5.238,P<0.001)。首次诊断为单纯胆囊结石和胆囊合并胆总管结石者其术后结石复发率分别为1.23%和2.76%,差异有统计学意义(χ2=42.104,P<0.001)。复发者中年龄>60岁在总计及男、女性中均占比最高,92%为汉族居民;10%的复发者有胆囊结石家族史;合并症中以伴高血压者占比最高。复发者中吸烟和饮酒者占比分别为76.7%和10.3%。63.8%的复发者BMI正常、23.2%为超重,且距第1次胆囊手术时体质量相比,60.1%的复发者体质量下降,22.9%体质量增加。不同性别复发者的年龄构成、民族分布、居住地类型、合并症、吸烟、饮酒、BMI分类、体质量变化差异均有统计学意义(P值均<0.001)。复发结石类型中多发、单发、泥沙样结石的比例为74∶15∶11;结石大小<1 cm、1~2 cm、>2 cm的占比分别为40.5%、48.8%和10.6%;手术方式为开腹和腹腔镜的比例分别为66.1%和33.9%;各类型血脂异常的比例均低于30%。不同性别复发者的初次结石种类、结石类型、结石大小、手术方式及高密度脂蛋白异常占比差异均有统计学意义(P值均<0.001)。影像学资料分析发现胆道结构异常者仅4例,表现为胆囊管长而弯曲,术后73.1%者伴有胆总管扩张。膳食因素随访发现55.8%的复发者平素饮食不规律。平素饮食结构以肉类和主食为主者分别占比43.8%和37.8%,且有性别差异,男性以肉类为主、女性以主食为主;64.1%的复发者平素有高盐高油的饮食习惯;59.8%的患者第1次结石术后饮食有改变,其中80%的患者能将饮食调整为规律(即饮食规律者可提高至92%)。 结论 本地区原发性胆总管结石复发率较低且无性别差异,复发高峰在术后10年,60岁以上人群是结石复发的集中群体。膳食因素及临床特征分析有助于医、患进一步认识原发性胆总管结石复发的特点,为后续采取针对性的预防提供基础依据。 -
关键词:
- 胆囊切除术 /
- 胆总管结石病 /
- 复发 /
- 病理状态, 体征和症状
Abstract:Objective To investigate the general situation, dietary factors, and clinical features of patients with recurrent primary common bile duct stones, and to provide a basis for effective prevention of stone recurrence. Methods A retrospective analysis was performed for 23 730 patients who underwent cholecystectomy due to cholelithiasis in Department of Hepatobiliary, Pancreatic and Spleen Surgery, Inner Mongolia People’s Hospital, from January 2013 to December 2023, and according to the presence or absence of recurrence of primary common bile duct stones after surgery, 334 patients were divided into recurrence group. The recurrence group was further analyzed based on sex in terms of recurrence rate, recurrence cycle, recurrence age, recurrence type, and general, disease, imaging, and dietary factors. The independent-samples t test was used for comparison of continuous data between two groups, the chi-square test was used for comparison of categorical data between two groups. Results There were 334 cases of recurrence of primary bile duct stones after cholecystectomy, with a recurrence rate of 1.41%, and the highest frequency of recurrence cycle was observed in 10 years after surgery, with a significant difference in recurrence cycle between the male and female patients (t=5.238, P<0.001). There was a significant difference in the recurrence rate of stones after surgery between the patients with simple gallstones and those with gallbladder and common bile duct stones at initial diagnosis (1.23% vs 2.76%, χ2=42.104, P<0.001). The patients with recurrence aged >60 years accounted for the highest proportion in the whole population and in both male and female populations, and 92% were Han residents; 10% of the patients with recurrence had a family history of gallstones, and as for comorbidities, the patients with hypertension accounted for the highest proportion. Among the patients with recurrence, the patients with smoking or drinking accounted for 76.7% and 10.3%, respectively. As for body weight, 63.8% of the patients with recurrence had a normal body mass index (BMI), and 23.2% of the patients were overweight; compared with body weight at the time of the first gallbladder surgery, a reduction in body weight was observed in 60.1% of the patients with recurrence, while an increase in body weight was observed in 22.9% of the patients with recurrence. There were significant differences between the male and female patients with recurrence in age composition, ethnicity, the type of place of residence, comorbidities, smoking, drinking, BMI, and the change in body weight (all P<0.001). As for the type of stone recurrence, the ratio of multiple stones, solitary stones, and muddy stones was 74∶15∶11, and the stone size of <1 cm, 1-2 cm, and >2 cm accounted for about 40.5%, 48.8%, and 10.6%, respectively. As for the surgical procedure, the patients undergoing laparotomy accounted for 66.1%, and those undergoing laparoscopy accounted for 33.9%. The patients with various types of dyslipidemia accounted for a percentage of<30%. There were significant differences between the male and female patients with recurrence in the type of stones at initial onset, the type and size of stones, and surgical procedure (all P<0.001). Imaging data showed that 4 patients had an abnormal structure of the bile duct, manifesting as long and curve cystic ducts, and 73.1% of the patients had common bile duct dilatation after surgery. The follow-up of dietary factors showed irregular diets in 55.8% of the patients with recurrence. As for the dietary structure, meat and staple food accounted for 43.8% and 37.8%, respectively, which showed a sex difference, with meat in male patients and staple food in female patients; 64.1% of the patients with recurrence had a high-salt and high-oil diet; 59.8% of the patients had changes in diet after the first surgery for stones, among whom 80% were able to have a regular diet, and the patients with a regular diet accounted for 92%. Conclusion There is a relatively low recurrence rate of primary common bile duct stones in this area, and there is no sex difference. The peak of recurrence is 10 years after surgery, and recurrence of stones is mainly observed in the population aged >60 years. The analysis of dietary and clinical features can help doctors and patients to further understand the characteristics of the recurrence of primary common bile duct stones and provide a basis for subsequent targeted prevention. -
临床上,胰腺恶性肿瘤大部分为原发肿瘤,胰腺转移癌少见[1]。胰腺转移癌与胰腺原发肿瘤鉴别困难,极易造成误诊,延误治疗。目前,胰腺转移癌国内外尚无统一治疗标准,原发肿瘤的生物学特性和针对原发肿瘤的综合治疗是决定其预后的主要因素,个体化差异较大。近期,笔者接诊1例宫颈鳞癌胰腺转移患者,现将病例资料及经验总结报告如下。
1. 病例资料
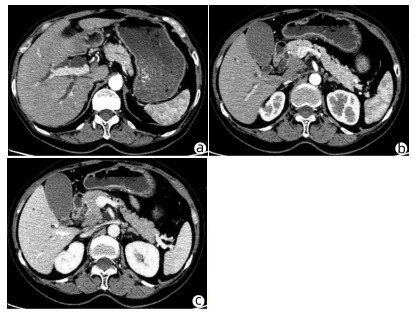
患者女性,63岁,因“皮肤、巩膜黄染20余天”于2021年3月27日入本院。起初黄染程度不重,后进行性加重,无腹痛腹胀,无阴道流血等其他不适。曾于2013年9月6日因阴道异常流血于外院行宫颈活检,病理学诊断为宫颈中分化鳞癌ⅢB期,予局部放疗联合TP方案(多西他赛+奥沙利铂)化疗,于2015年结束治疗后复查腹盆腔脏器、腹腔、盆腔均未见肿瘤转移。出院后患者再未复查,亦无特殊不适。入院查体:皮肤巩膜明显黄染,腹平坦,腹部无压痛,腹部未触及肿块。辅助检查:TBil 282.99 μmol/L,DBil 203.80 μmol/L,CA19-9正常;妇科彩超示:老年性子宫;全腹盆腔增强CT示:肝内外胆管扩张,主胰管可见(图 1a),胆囊明显增大,胆总管下段狭窄,动脉期见胰腺钩突区低密度肿块(图 1b),静脉期肿块轻度强化(图 1c),子宫显示不明显,腹膜后可见多发淋巴结肿大;磁共振胰胆管造影示:胰头区异常信号肿块,肝内外胆管扩张,胆汁淤积;超声内镜示:胰头钩突区占位,直径约3 cm。入院后予以护肝利胆治疗,患者黄疸进行性加重,建议患者行穿刺活检、PET-CT检查,患方拒绝。2021年4月4日行剖腹探查:术中探查发现肿瘤位于胰头钩突区,质地硬,侵犯十二指肠壁和胆总管,腹膜后见多发淋巴结肿大,行胰头十二指肠切除术。术后病理学检查结果:胰腺钩突肿块大小3.0 cm×2.0 cm×1.5 cm,癌组织侵犯十二指肠及胆总管,胰腺切缘未见癌。癌组织呈团块状或条索状癌巢(图 2a),癌细胞及核大小、形态不一,分布不规则,核分裂像多见,癌组织侵犯淋巴管及血管,脉管内见癌栓(图 2b),周围淋巴结可见癌转移(2/2)。免疫组化:P16(弥漫性+),P63(+),P40(+),CK7(+),CK8(+),CK19(+),ER(+)(图 2c、d)。诊断考虑胰腺钩突区中分化鳞状细胞癌,结合临床病史及免疫组化结果,考虑宫颈鳞癌转移。目前,该患者于本院进一步针对原发肿瘤行化疗等综合治疗,日常生活行为已恢复正常。
2. 讨论
据统计,宫颈癌的患病/病死率在女性恶性肿瘤中居第4位,鳞状细胞癌是最常见的病理类型,占比约80%,P16、P40等表达阳性对宫颈鳞癌诊断有重要意义。宫颈鳞癌早期往往无特殊表现,晚期可出现异常阴道流血、腰痛、盆腔痛、性交痛、贫血等表现,诊断时大多发生转移,多转移至直肠、膀胱、盆腔、肺、骨、肝等。临床上,胰腺癌多为原发肿瘤,胰腺转移癌罕见,仅占胰腺恶性肿瘤总数的2%~3%[2]。在一项纳入973例胰腺肿瘤手术标本病理资料的研究[3]中,共38例为胰腺转移瘤,主要包括淋巴瘤11例,胃癌7例,肾癌6例,肺癌2例,肝癌、前列腺癌、卵巢癌、子宫癌各1例,默克尔细胞癌1例,另有3例胃肠道恶性间质瘤和1例腹膜后平滑肌肉瘤;81例转移性胰腺肿瘤尸检报告显示,主要来源肺癌34例,胃肠道20例,肾脏4例,乳腺3例,肝脏2例,卵巢和膀胱各1例,另有6例来自造血系统,黑色素瘤、肉瘤和间皮瘤各2例。来源于宫颈的胰腺转移癌并不多见,笔者在国内外文献检索系统中,共检出各类型宫颈癌胰腺转移病例报告10例[4-7],其中鳞癌3例,神经内分泌癌5例,腺癌2例;转移灶位于胰头3例,位于颈部1例,位于胰腺体部3例,位于尾部、体尾部和胰头及体尾部各1例。转移灶位于胰头的3例患者中,1例为鳞癌,2例为神经内分泌癌,胰腺转移部位与宫颈癌病理类型无明显关联。本例患者在宫颈鳞癌同步放化疗后再未复查,6年后转移至胰腺钩突,临床表现为梗阻性黄疸,行胰头十二指肠切除术,术后病理学检查考虑鳞癌,结合免疫组化考虑为宫颈癌来源。目前,国内尚未见类似报道,国外也鲜有相关报道。
原发性胰腺癌与胰腺转移癌鉴别需依赖血清CA19-9水平、CT、MRI、磁共振胰胆管造影、内镜逆行胰胆管造影、超声内镜等检查手段。本例患者CT和MRI特点较原发性胰腺癌无特异表现,鉴别困难。血清CA19-9水平升高常见于胆道、胰腺恶性肿瘤,对诊断原发性胰腺癌有较高的敏感度和特异度[8]。鉴别困难时,可采用通过超声、CT及内镜引导下穿刺活检获取胰腺组织学、细胞学标本进行确诊,但需要评估穿刺活检的出血风险[9]。一般认为,超声内镜经十二指肠细针穿刺抽吸活检可提高胰腺疾病诊断的准确性,且相对安全[10-11]。本例患者术前影像学检查提示胰头钩突区占位,CA19-9水平不高,且有宫颈鳞癌病史,建议进一步行穿刺活检、PET-CT检查。但患者存在梗阻性黄疸,肝功能持续恶化,有手术指征,且患者家属不同意术前行穿刺活检、PET-CT等进一步检查,因此术前未能获得病理学诊断。
转移性胰腺癌临床表现因胰腺转移部位不同而异。在笔者检出的10例报告中,仅有1例(鳞癌)出现梗阻性黄疸,提示宫颈癌胰腺转移鲜有梗阻性黄疸症状,部分病例可因肿瘤压迫出现胆胰管扩张。转移性胰腺癌出现胰胆管梗阻较少见,可能与原发肿瘤主要经过淋巴及血行途径转移侵犯胰腺,不侵犯胆胰管有关[12]。本例患者胰腺转移性肿瘤致梗阻性黄疸,目前国内尚未见类似报道,国外仅有1例类似报道,但未分析相关转移机制。本例患者影像学检查示肝、胃、肠道等器官均未见肿瘤,但有腹膜后淋巴结肿大,病理学检查阳性;在既往10例报告中,3例胰腺转移性宫颈鳞癌有2例伴腹膜后淋巴结肿大,因此笔者推测宫颈鳞癌胰腺转移可能与腹膜后淋巴结侵犯相关。
关于转移性胰腺癌是否需要手术,意见尚未统一。以急腹症、进行性黄疸、出血为临床表现患者,应行急诊手术治疗,解除症状同时,切除病灶送检,根据病理学检查结果制订综合治疗方案。研究[13-14]表明,转移性胰腺癌行手术切除相较于保守治疗可延长生存期,且根治性手术相较于姑息性手术,预后更好。术后根据原发病灶辅以化疗等综合治疗,可提高治疗效果。对无法接受手术的转移性胰腺癌患者,应根据原发肿瘤的生物学特性制订以放疗为主的个体化综合治疗方案[15]。本例患者影像学检查提示存在胆道梗阻,并见胰头钩突区占位;胆红素水平持续升高,手术指征明确,手术切除胰腺钩突病灶、解除胆道梗阻后,胆红素水平明显下降,目前患者恢复良好,进一步接受化疗等综合治疗,延长生存期。
笔者经验总结:(1)对于诊断不明确的胰腺肿瘤,术前条件允许情况下需行穿刺活检明确性质,以指导下一步治疗方案;(2)胰腺转移癌在具备手术条件情况下,应积极采取以根治性手术为主的治疗方案,姑息性切除方案亦可行。胰腺转移癌为晚期癌症,术后需早期予以放化疗、靶向、免疫治疗等综合治疗;(3)对于不具备手术条件的患者,需根据原发肿瘤予以抗肿瘤综合治疗,包括放疗、化疗以及免疫治疗、靶向治疗等[16-17]。
-
表 1 胆囊切除术后原发性胆总管结石复发概况分析
Table 1. General situation analysis of primary bile duct stone recurrence after cholecystectomy
项目 例数 复发[例(%)] 复发周期(年) 复发年龄(岁) 复发结石类别(例)1) Ⅰ Ⅱ Ⅲ 男 7 608 108(1.42) 7±5 64±10 9 83 16 女 16 111 226(1.40) 12±8 62±13 26 180 20 合计 23 719 334(1.41) 10±8 63±12 35 263 36 统计值 χ2=0.004 t=5.238 t=0.786 χ2=3.186 P值 0.953 <0.001 0.433 0.203 注:1)复发结石类别为胆囊残端结石(Ⅰ)、胆总管结石(Ⅱ)、二者均有(Ⅲ)。
表 2 一般资料分析
Table 2. General information situation analysis table
指标 合计(n=301) 男性(n=97) 女性(n=204) χ2值 P值 年龄分层[例(%)] 336.759 <0.001 <50岁 43(14.3) 11(11.3) 32(15.7) 50~60岁 66(21.9) 23(23.7) 43(21.0) 61~70岁 107(35.5) 32(33.0) 75(36.8) ≥71岁 85(28.2) 31(32.0) 54(26.5) 民族[例(%)] 336.101 <0.001 汉族 277(92.0) 87(89.7) 190(93.1) 蒙古族 24(8.0) 10(10.3) 14(6.9) 居住地类型[例(%)] 339.101 <0.001 市 110(36.5) 35(36.1) 75(36.8) 县 66(21.9) 28(28.9) 38(18.6) 村 125(41.5) 34(35.0) 91(44.6) 胆囊结石家族史[例(%)] 0.922 0.337 有 30(10.0) 12(12.4) 18(8.8) 无 271(90.0) 85(87.6) 186(91.2) 合并症[例(%)] 338.640 <0.001 糖尿病 20(6.6) 6(6.2) 14(6.9) 高血压 57(18.9) 13(13.4) 44(21.6) 糖尿病+高血压 17(5.6) 4(4.1) 13(6.4) 呼吸系统疾病 15(4.9) 12(12.4) 3(1.5) 无 192(63.7) 62(63.9) 130(63.7) 吸烟[例(%)] 50.916 <0.001 有 231(76.7) 50(51.5) 181(88.7) 无 70(23.3) 47(48.5) 23(11.3) 饮酒[例(%)] 有 31(10.3) 24(24.7) 7(3.4) 32.318 <0.001 无 270(89.7) 73(75.3) 197(96.6) BMI分类[例(%)] 354.612 <0.001 消瘦 17(5.6) 1(1.0) 16(7.8) 正常 192(63.8) 52(53.6) 140(68.6) 超重 70(23.2) 32(33.0) 38(18.6) 肥胖 22(7.3) 12(12.4) 10(4.9) 体质量变化[例(%)] 339.826 <0.001 增加 69(22.9) 30(31.0) 39(19.2) 下降 181(60.1) 53(54.6) 128(62.7) 不变 51(16.9) 14(14.4) 37(18.1) 表 3 初次胆石病相关疾病资料分析
Table 3. Data analysis of primary cholelithiasis related diseases
指标 合计(n=301) 男性(n=97) 女性(n=204) χ2值 P值 初次结石种类[例(%)] 343.587 <0.001 单纯胆囊结石 256(85.0) 74(76.3) 182(89.2) 胆囊+胆管结石 45(15.0) 23(23.7) 22(10.8) 结石类型[例(%)] 334.814 <0.001 单发 46(15.3) 16(16.5) 30(14.7) 多发 223(74.1) 71(73.2) 152(74.5) 泥沙样 32(10.6) 10(10.3) 22(10.8) 结石大小[例(%)] 334.199 <0.001 <1 cm 122(40.5) 41(42.3) 81(39.7) 1~2 cm 147(48.8) 46(47.4) 101(49.5) >2 cm 32(10.6) 10(10.3) 22(10.8) 手术方式[例(%)] 343.332 <0.001 开腹 199(66.1) 53(54.6) 146(71.6) 腹腔镜 102(33.9) 44(45.4) 58(28.4) 血脂[例(%)] 高胆固醇 16(5.3) 6(6.2) 10(4.9) 2.080 0.353 高甘油三酯 58(19.3) 22(22.7) 36(17.6) 8.856 0.012 HDL异常 83(27.5) 38(39.2) 45(22.1) 22.422 <0.001 LDL异常 30(9.9) 11(11.3) 19(9.3) 3.944 0.139 表 4 影像学资料分析
Table 4. Analysis of imaging data
指标 合计(n=301) 男性(n=97) 女性(n=204) χ2值 P值 胆道结构异常[例(%)] 334.651 <0.001 有 4(1.3) 2(2.1) 2(1.0) 无 297(98.7) 95(97.9) 202(99.0) 胆总管有无扩张[例(%)] 334.104 <0.001 有 220(73.1) 72(74.2) 148(72.5) 无 81(26.9) 25(25.8) 56(27.5) 表 5 胆囊切除术后膳食因素分析
Table 5. Analysis of dietary factors after cholecystectomy
膳食因素 合计(n=301) 男性(n=97) 女性(n=204) 平素饮食规律[例(%)] 是 133(44.2) 44(45.4) 89(43.6) 否 168(55.8) 53(54.6) 115(56.4) 不吃早餐 89(53.0) 20(37.7) 69(60.0) 就餐时间不固定 47(27.9) 7(13.2) 40(34.7) 夜加餐 32(19.0) 26(49.0) 6(5.2) 平素饮食结构[例(%)] 主食为主 114(37.8) 27(27.8) 87(42.6) 肉类为主 132(43.8) 52(53.6) 80(39.2) 均衡饮食 48(15.9) 16(16.5) 32(15.7) 素食 7(2.3) 2(2.1) 5(2.5) 平素饮食习惯[例(%)] 高油高盐 193(64.1) 67(69.1) 126(61.8) 适中 108(35.8) 30(30.9) 78(38.2) 术后饮食改变[例(%)] 有改变 180(59.8) 61(62.9) 119(58.3) 改变规律 144(80.0) 50(82.0) 94(79.0) 调整结构 29(16.1) 10(16.4) 19(16.0) 二者均改变 7(3.9) 1(1.6) 6(5.0) 无改变 121(40.2) 36(37.1) 85(41.7) -
[1] LI JQ, ZHANG GX. Research advances in the risk factors for recurrence of common bile duct stone after choledocholithotomy[J]. J Clin Hepatol, 2023, 39( 1): 231- 237. DOI: 10.3969/j.issn.1001-5256.2023.01.036.李积强, 张桂信. 胆总管取石术后结石复发危险因素的研究进展[J]. 临床肝胆病杂志, 2023, 39( 1): 231- 237. DOI: 10.3969/j.issn.1001-5256.2023.01.036. [2] CIANCI P, RESTINI E. Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches[J]. World J Gastroenterol, 2021, 27( 28): 4536- 4554. DOI: 10.3748/wjg.v27.i28.4536. [3] ZHU JH, ZHAO SL, KANG Q, et al. Classification of anatomical morphology of cystic duct and its association with gallstone[J]. World J Gastrointest Surg, 2024, 16( 2): 307- 317. DOI: 10.4240/wjgs.v16.i2.307. [4] YOO ES, YOO BM, KIM JH, et al. Evaluation of risk factors for recurrent primary common bile duct stone in patients with cholecystectomy[J]. Scand J Gastroenterol, 2018, 53( 4): 466- 470. DOI: 10.1080/00365521.2018.1438507. [5] WU Y, XU CJ, XU SF. Advances in risk factors for recurrence of common bile duct stones[J]. Int J Med Sci, 2021, 18( 4): 1067- 1074. DOI: 10.7150/ijms.52974. [6] Chinese Nutrition Society. Dietary guidelines for Chinese residents(2022): Balanced dietary pattern[M]. Beijing: People’s Medical Publishing House, 2022: 303.中国营养学会. 中国居民膳食指南(2022): 平衡膳食模式[M]. 北京: 人民卫生出版社, 2022: 303. [7] LU JH, TONG GX, HU XY, et al. Construction and evaluation of a nomogram to predict gallstone disease based on body composition[J]. Int J Gen Med, 2022, 15: 5947- 5956. DOI: 10.2147/IJGM.S367642. [8] Section of Biliary Surgery, Branch of Surgery, Chinese Medical Association, Chinese Committee of Biliary Surgeons. Expert consensus on diagnosis and treatment of common complications after cholecystectomy(2018 edition)[J]. Clin Educ Gen Pract, 2018, 16( 3): 244- 246. DOI: 10.13558/j.cnki.issn1672-3686.2018.03.002.中华医学会外科学分会胆道外科学组, 中国医师协会外科医师分会胆道外科医师委员会. 胆囊切除术后常见并发症的诊断与治疗专家共识(2018版)[J]. 全科医学临床与教育, 2018, 16( 3): 244- 246. DOI: 10.13558/j.cnki.issn1672-3686.2018.03.002. [9] ANDREWS S. Gallstone size related to incidence of post cholecystectomy retained common bile duct stones[J]. Int J Surg, 2013, 11( 4): 319- 321. DOI: 10.1016/j.ijsu.2013.02.009. [10] ZHANG S. Safety and prognostic evaluation of laparoscopic cholecystectomy for acute cholecystitis complicated with gallstones[J/CD]. J Clin Med Lit, 2018, 5( 93): 40- 41. DOI: 10.16281/j.cnki.jocml.2018.93.029.张松. 腹腔镜胆囊切除术治疗急性胆囊炎并发胆结石的安全性及预后评估[J/CD]. 临床医药文献电子杂志, 2018, 5( 93): 40- 41. DOI: 10.16281/j.cnki.jocml.2018.93.029. [11] PARK SY, HONG TH, LEE SK, et al. Recurrence of common bile duct stones following laparoscopic common bile duct exploration: A multicenter study[J]. J Hepatobiliary Pancreat Sci, 2019, 26( 12): 578- 582. DOI: 10.1002/jhbp.675. [12] WEILAND CJS, SMEETS XJNM, UMANS DS, et al. Aggressive hydration and post-ERCP pancreatitis-Authors’ reply[J]. Lancet Gastroenterol Hepatol, 2021, 6( 9): 686- 687. DOI: 10.1016/S2468-1253(21)00235-1. [13] WU YY, YAN SJ, LI DP, et al. Retrospective study of the clinical characteristics of ERCP and LCBDE in treatment of gallbladder stones and stone recurrence[J]. Chin J Gen Pract, 2020, 18( 2): 188- 190, 207. DOI: 10.16766/j.cnki.issn.1674-4152.001201.吴炎炎, 燕善军, 李大鹏, 等. 回顾性研究ERCP与LCBDE治疗胆管结石临床特点及结石复发情况[J]. 中华全科医学, 2020, 18( 2): 188- 190, 207. DOI: 10.16766/j.cnki.issn.1674-4152.001201. [14] WU Y, ZHANG Y, JIANG XM, et al. Risk factors for single and multiple recurrences for endoscopic retrograde cholangiopancreatography and open choledochotomy in treating choledocholithiasis[J]. Gastroenterol Res Pract, 2023, 2023: 4738985. DOI: 10.1155/2023/4738985. [15] DING GQ, CAI W, QIN MF. Single-stage vs. two-stage management for concomitant gallstones and common bile duct stones: A prospective randomized trial with long-term follow-up[J]. J Gastrointest Surg, 2014, 18( 5): 947- 951. DOI: 10.1007/s11605-014-2467-7. [16] ZHANG WJ, XU GF, HUANG Q, et al. Treatment of gallbladder stone with common bile duct stones in the laparoscopic era[J]. BMC Surg, 2015, 15: 7. DOI: 10.1186/1471-2482-15-7. [17] PARK BK, SEO JH, JEON HH, et al. A nationwide population-based study of common bile duct stone recurrence after endoscopic stone removal in Korea[J]. J Gastroenterol, 2018, 53( 5): 670- 678. DOI: 10.1007/s00535-017-1419-x. [18] LEE SJ, CHOI IS, MOON JI, et al. Optimal treatment for concomitant gallbladder stones with common bile duct stones and predictors for recurrence of common bile duct stones[J]. Surg Endosc, 2022, 36( 7): 4748- 4756. DOI: 10.1007/s00464-021-08815-1. [19] QIN XX, MA RL, GUO H, et al. Effect of health education on gallstone disease among uygur rural residents in Xinjiang production and construction corps: Evaluation on a two years intervention program[J]. Chin J Public Health, 2023, 39( 1): 86- 91. DOI: 10.11847/zgggws1138099.秦茜茜, 马儒林, 郭恒, 等. 新疆生产建设兵团维吾尔族农村居民胆结石健康教育干预效果评价[J]. 中国公共卫生, 2023, 39( 1): 86- 91. DOI: 10.11847/zgggws1138099. [20] ZHU WG, ZHENG XP. Analysis of risk factors for postoperative recurrence of common bile duct stones[J]. J Qiqihar Univ Med, 2016, 37( 16): 2050- 2052.朱卫国, 郑小平. 胆总管结石术后复发的相关危险因素分析[J]. 齐齐哈尔医学院学报, 2016, 37( 16): 2050- 2052. [21] WANG LM, CHEN C, DING H, et al. Risk factors of recurrence after endoscopic retrograde cholangiopancreatography combined with laparoscopic cholecystectomy for gallbladder and choledocholithiasis[J/CD]. Chin Arch Gen Surg(Electronic Edition), 2019, 13( 3): 224- 228. DOI: 10.3877/cma.j.issn.1674-0793.2019.03.012.王雷鸣, 陈晨, 丁辉, 等. 经内镜逆行胰胆管造影联合腹腔镜胆囊切除术后胆囊结石合并胆总管结石复发的危险因素分析[J/CD]. 中华普通外科学文献(电子版), 2019, 13( 3): 224- 228. DOI: 10.3877/cma.j.issn.1674-0793.2019.03.012. [22] RYU S, JO IH, KIM S, et al. Clinical impact of common bile duct angulation on the recurrence of common bile duct stone: A meta-analysis and review[J]. Korean J Gastroenterol, 2020, 76( 4): 199- 205. DOI: 10.4166/kjg.2020.76.4.199. [23] CHOI SJ, YOON JH, KOH DH, et al. Low insertion of cystic duct increases risk for common bile duct stone recurrence[J]. Surg Endosc, 2022, 36( 5): 2786- 2792. DOI: 10.1007/s00464-021-08563-2. [24] LU ZH, NIU J, XU PP, et al. Analysis of related risk factors for recurrence of choledocholithiasis after the operation[J]. Chin J Curr Adv Gen Surg, 2016, 19( 5): 372- 375. DOI: 10.3969/j.issn.1009-9905.2016.05.011.鲁志华, 牛军, 许平平, 等. 胆总管取石并胆囊切除术后胆总管结石复发的相关危险因素分析[J]. 中国现代普通外科进展, 2016, 19( 5): 372- 375. DOI: 10.3969/j.issn.1009-9905.2016.05.011. [25] QUARESIMA S, BALLA A, GUERRIERI M, et al. Results of medium seventeen years' follow-up after laparoscopic choledochotomy for ductal stones[J]. Gastroenterol Res Pract, 2016, 2016: 9506406. DOI: 10.1155/2016/9506406. [26] WU RZ. Analysis of factors associated with recurrence of choledocholithiasis after choledochotomy with cholecystectomy[J]. Chin Foreign Med Res, 2017, 15( 5): 45- 47. DOI: 10.14033/j.cnki.cfmr.2017.5.024.吴润芝. 胆总管取石并胆囊切除术后胆总管结石复发的相关因素分析[J]. 中外医学研究, 2017, 15( 5): 45- 47. DOI: 10.14033/j.cnki.cfmr.2017.5.024. [27] SI YG, ZHANG GC. Postoperative recurrence of gallstone complicated with common bile duct stones treated with LC combined with LCHTD and its influencing factors[J]. J Bengbu Med Coll, 2018, 43( 2): 223- 226. DOI: 10.13898/j.cnki.issn.1000-2200.2018.02.024.司宇光, 张国超. 胆囊结石合并胆总管结石病人LC联合LCHTD术后结石复发情况及其影响因素分析[J]. 蚌埠医学院学报, 2018, 43( 2): 223- 226. DOI: 10.13898/j.cnki.issn.1000-2200.2018.02.024. [28] HE HZ, ZHOU Z, YIN QH, et al. Retrospective study on the clinical effect of the treatment of ERCP+LC and LC+LCBDE on cholecystolithiasis and choledocholithiasis[J]. J Pract Med, 2018, 34( 11): 1889- 1892. DOI: 10.3969/j.issn.1006-5725.2018.11.033.何恒正, 周峥, 尹清华, 等. ERCP+LC和LC+LCBDE治疗胆囊结石合并胆总管结石的效果比较[J]. 实用医学杂志, 2018, 34( 11): 1889- 1892. DOI: 10.3969/j.issn.1006-5725.2018.11.033. [29] DENG F, ZHOU M, LIU PP, et al. Causes associated with recurrent choledocholithiasis following therapeutic endoscopic retrograde cholangiopancreatography: A large sample sized retrospective study[J]. World J Clin Cases, 2019, 7( 9): 1028- 1037. DOI: 10.12998/wjcc.v7.i9.1028. [30] CAI Y, HE YA. Risk factors for recurrence of stones after LC combined LCHTD in patients with gallbladder and common bile duct stones[J]. J Hepatobiliary Surg, 2016, 24( 3): 203- 205.蔡宇, 何彦安. 胆囊结石合并胆总管结石患者行腹腔镜胆囊切除联合胆总管切开取石T管引流术后结石复发危险因素分析[J]. 肝胆外科杂志, 2016, 24( 3): 203- 205. [31] PASPATIS GA, PARASKEVA K, VARDAS E, et al. Long-term recurrence of bile duct stones after endoscopic papillary large balloon dilation with sphincterotomy: 4-year extended follow-up of a randomized trial[J]. Surg Endosc, 2017, 31( 2): 650- 655. DOI: 10.1007/s00464-016-5012-9. [32] SONG ME, CHUNG MJ, LEE DJ, et al. Cholecystectomy for prevention of recurrence after endoscopic clearance of bile duct stones in Korea[J]. Yonsei Med J, 2016, 57( 1): 132- 137. DOI: 10.3349/ymj.2016.57.1.132. [33] CAI M, YU YH. Progress on risk factors for postoperative recurrence of common bile duct stones[J/CD]. Chin Arch Gen Surg(Electronic Edition), 2022, 16( 6): 438- 442. DOI: 10.3877/cma.j.issn.1674-0793.2022.06.013.蔡茗, 俞亚红. 胆总管结石术后复发危险因素的研究进展[J/CD]. 中华普通外科学文献(电子版), 2022, 16( 6): 438- 442. DOI: 10.3877/cma.j.issn.1674-0793.2022.06.013. [34] JEON J, SU LIM, PARK CH, et al. Restoration of common bile duct diameter within 2 weeks after endoscopic stone retraction is a preventive factor for stone recurrence[J]. Hepatobiliary Pancreat Dis Int, 2018, 17( 3): 251- 256. DOI: 10.1016/j.hbpd.2018.03.014. [35] WANG CY, GUO Y. A study on relationship between postoperative stone recurrence and disease cognition and dietary composition in elderly patients with gallstones[J]. Geriatr Health Care, 2023, 29( 6): 1364- 1368. DOI: 10.3969/j.issn.1008-8296.2023.06.052.王春艳, 郭韵. 老年胆囊结石患者术后结石复发与疾病认知及饮食构成的关系研究[J]. 老年医学与保健, 2023, 29( 6): 1364- 1368. DOI: 10.3969/j.issn.1008-8296.2023.06.052. [36] WANG JH. Effect of self-efficacy intervention on the postoperative behavior, diet, and relapse within one year in patients with gallstone[J]. Tibet Med, 2017, 38( 1): 58- 60.王俊红. 自我效能提升干预对胆囊结石患者术后行为、饮食习惯及1年复发率的影响[J]. 西藏医药, 2017, 38( 1): 58- 60. [37] ZHANG XL, MA Q, ZHANG L, et al. Investigation and analysis of the incidence and risk factors of gallstones in Dayi County, Chengdu City[J]. South China J Prev Med, 2023, 49( 6): 686- 689. DOI: 10.12183/j.scjpm.2023.0686.张孝亮, 马秋, 张雳, 等. 成都市大邑地区胆结石发病现状及危险因素调查分析[J]. 华南预防医学, 2023, 49( 6): 686- 689. DOI: 10.12183/j.scjpm.2023.0686. [38] GRIGOR’EVA IN, ROMANOVA TI. Gallstone disease and microbiome[J]. Microorganisms, 2020, 8( 6): 835. DOI: 10.3390/microorganisms8060835. [39] BAI JD, XUE RQ, BAI YL, et al. Association between metabolic syndrome and gallstones[J]. J Clin Hepatol, 2020, 36( 3): 701- 703. DOI: 10.3969/j.issn.1001-5256.2020.03.052.白济东, 薛荣泉, 白永乐, 等. 代谢综合征与胆囊结石的关系[J]. 临床肝胆病杂志, 2020, 36( 3): 701- 703. DOI: 10.3969/j.issn.1001-5256.2020.03.052. 期刊类型引用(1)
1. 李帅,王娟,夏仕雪,顾鹏. 子宫颈混合性腺神经内分泌癌胰腺转移1例. 中国医学影像学杂志. 2022(12): 1283-1284 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 877 KB)
PDF下载 ( 877 KB)


 下载:
下载:


 下载:
下载:
 百度学术
百度学术