基于APRI和PALBI构建的列线图对肝硬化并发食管胃底静脉曲张破裂出血的预测价值
DOI: 10.12449/JCH240314
Establishment of a nomogram model for predicting liver cirrhosis with esophagogastric variceal bleeding based on aspartate aminotransferase-to-platelet ratio index and platelet-albumin-bilirubin score
-
摘要:
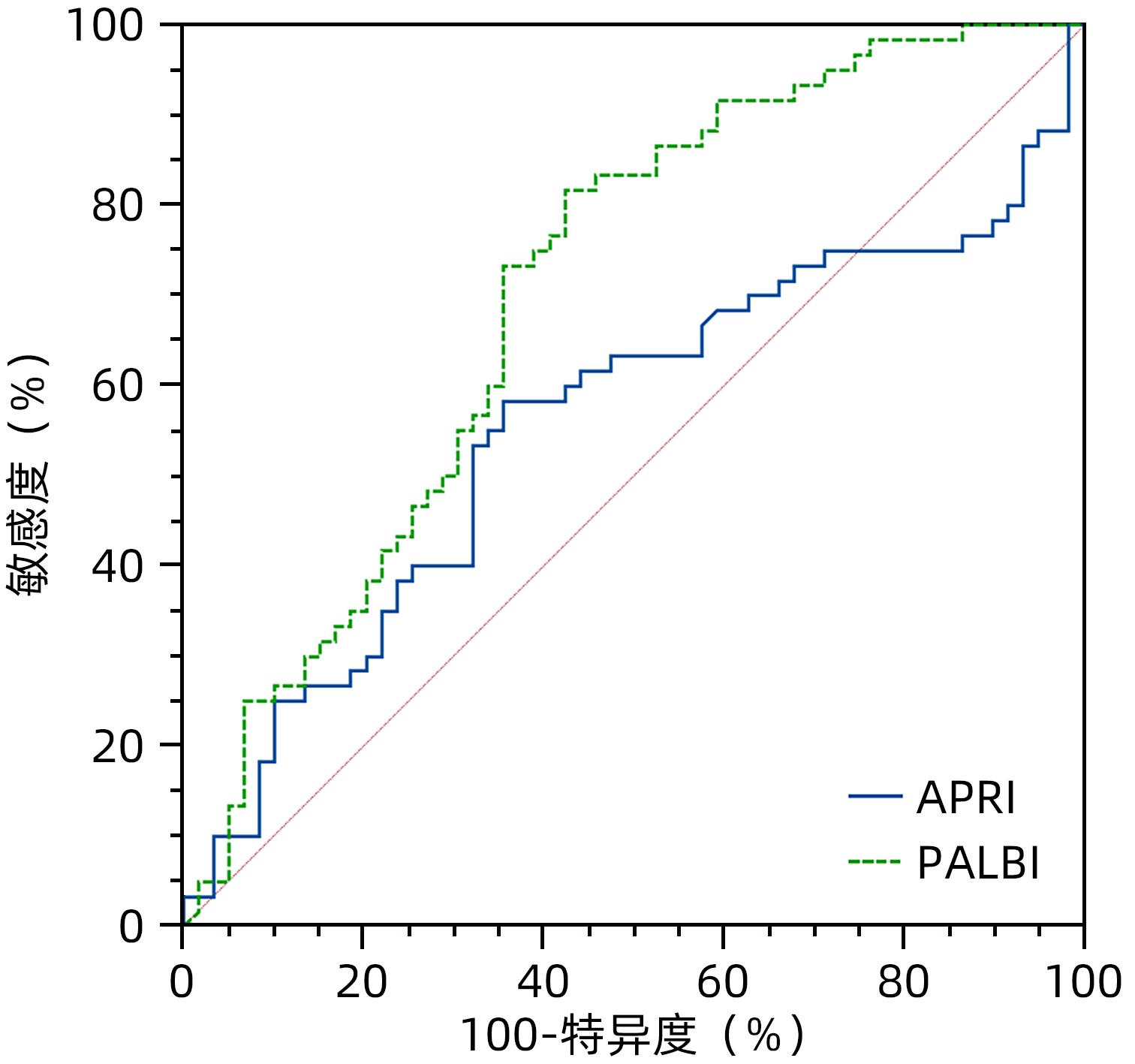
目的 评估天冬氨酸转氨酶与血小板比值指数(APRI)和血小板-白蛋白-胆红素评分(PALBI)对肝硬化并发食管胃底静脉曲张破裂出血风险的预测价值。 方法 选取苏州大学附属第一医院于2021年5月—2022年6月收治的肝硬化患者119例,收集患者的临床资料、血常规、血清生化及血凝等检查结果。根据是否合并食管胃底静脉曲张破裂出血,将患者分为未出血组(n=59)和出血组(n=60),比较组间差异。正态分布的计量资料两组间比较采用独立样本t检验,非正态分布的计量资料两组间比较采用Mann-Whitney U检验。计数资料组间比较采用χ2检验或Fisher精确概率法。使用多因素Logistic回归分析,筛选肝硬化并发食管胃底静脉曲张破裂出血的独立危险因素,并构建列线图预测模型。 结果 出血组男性患者占75.00%,未出血组男性患者占40.68%,两组在性别构成方面,差异具有统计学意义(χ2=14.384,P<0.001)。出血组和未出血组患者病因均以慢性乙型肝炎为主(53.33% vs 38.98%),两者构成比差异无统计学意义(χ2=2.464,P=0.116)。出血组患者抗凝血酶原Ⅲ活性(AT-IIIA)水平高于未出血组(t=3.329,P=0.001),PLT、TBil、Ca、TC、TT水平则低于未出血组(P值均<0.05)。APRI和PALBI在出血组和未出血组之间比较,差异均有统计学意义(χ2值分别为6.175、19.532,P值均<0.05)。进一步二元Logistic回归分析发现,APRI(OR=0.309,95%CI:0.109~0.881,P=0.028)、PALBI(OR=7.667,95%CI:2.005~29.327,P=0.003)、Ca(OR=0.001,95%CI:0.000~0.141,P=0.007)、TC(OR=0.469,95%CI:0.226~0.973,P=0.042)和TT(OR=0.599,95%CI:0.433~0.830,P=0.002)是影响肝硬化并发食管胃底静脉曲张破裂出血的独立影响因素。基于以上因素建立列线图模型,一致性指数(C-index)为0.899,校准曲线拟合良好。 结论 APRI及PALBI对肝硬化并发食管胃底静脉曲张破裂出血具有良好的预测价值,基于本研究构建的列线图模型可以个体化预测肝硬化患者食管胃底静脉曲张破裂出血发生率。 Abstract:Objective To investigate the value of aspartate aminotransferase-to-platelet ratio index (APRI) and platelet-albumin-bilirubin (PALBI) score in predicting the risk of esophagogastric variceal bleeding in patients with liver cirrhosis. Methods A total of 119 patients with liver cirrhosis who were admitted to The First Affiliated Hospital of Soochow University from May 2021 and June 2022 were enrolled, and clinical data, routine blood test results, serum biochemistry, and coagulation test results were collected from all patients. According to the presence or absence of esophagogastric variceal bleeding, the patients were divided into non-bleeding group with 59 patients and bleeding group with 60 patients, and a comparative analysis was performed for the two groups. The independent samples t-test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups; the chi-squared test or the Fisher’s exact test was used for comparison of categorical data between groups. The multivariate Logistic regression analysis was used to identify the independent risk factors for esophagogastric variceal bleeding in patients with liver cirrhosis and establish a nomogram predictive model. Results The male patients accounted for 75.00% in the bleeding group and 40.68% in the non-bleeding group, and there was a significant difference in sex composition between the two groups (χ2=14.384, P<0.001). Chronic hepatitis B was the main etiology in both the bleeding group and the non-bleeding group (53.33% vs 38.98%), and there was no significant difference in composition ratio between the two groups (χ2=2.464, P=0.116). Compared with the non-bleeding group, the bleeding group had a significantly higher activity of AT-IIIA (t=3.329, P=0.001) and significantly lower levels of PLT, TBil, Ca, TC, and TT (all P<0.05). There were significant differences in APRI and PALBI between the two groups (χ2=6.175 and 19.532, both P<0.05). The binary logistic regression analysis showed that APRI (odds ratio [OR]=0.309, 95% confidence interval [CI]: 0.109 — 0.881, P=0.028), PALBI (OR=7.667, 95%CI: 2.005 — 29.327, P=0.003), Ca (OR=0.001, 95%CI: 0.000 — 0.141, P=0.007), TC (OR=0.469, 95%CI: 0.226 — 0.973, P=0.042), and TT (OR=0.599, 95%CI: 0.433 — 0.830, P=0.002) were independent influencing factors for esophagogastric variceal bleeding in liver cirrhosis. A nomogram model was established based on the above factors and had an index of concordance of 0.899 and a well-fitted calibration curve. Conclusion APRI and PALBI have a good value in predicting esophagogastric variceal bleeding in patients with liver cirrhosis, and the nomogram model established based on this study can predict the incidence rate of esophagogastric variceal bleeding in patients with liver cirrhosis. -
Key words:
- Liver Cirrhosis /
- Esophageal and Gastric Varices /
- Gastrointestinal Hemorrhage /
- APRI /
- PALBI /
- Nomograms
-
表 1 肝硬化并发消化道出血患者临床特征
Table 1. Clinical characteristics of patients with liver cirrhosis complicated by gastrointestinal bleeding
项目 出血组(n=60) 未出血组(n=59) 统计值 P值 性别[例(%)] χ2=14.384 <0.001 男 45(75.00) 24(40.68) 女 15(25.00) 35(59.32) 年龄(岁) 58.00±14.48 62.29±14.29 t=-1.626 0.107 肝硬化病因[例(%)] 乙型肝炎 32(53.33) 23(38.98) χ2=2.464 0.116 酒精性 7(11.67) 1(1.69) χ2=3.261 0.071 血吸虫性 7(11.67) 13(22.04) χ2=2.287 0.130 自身免疫性 1(1.66) 4(6.78) χ2=0.871 0.351 其他 13(21.67) 18(30.51) χ2=0.464 0.496 WBC(×109/L) 3.30(2.45~4.59) 3.03(2.36~4.20) Z=-0.460 0.646 PLT(×109/L) 56.00(43.00~69.25) 65.00(50.00~84.00) Z=-2.318 0.020 TBil(μmol/L) 19.15(12.35~25.93) 31.50(21.90~47.60) Z=-5.084 <0.001 AST(U/L) 31.90(23.28~43.95) 36.80(28.00~47.90) Z=-1.629 0.103 Alb(g/L) 31.18±3.63 30.92±6.23 t=-0.273 0.785 APRI[例(%)] χ2=6.175 0.013 ≤0.597 25(41.67) 38(64.41) >0.597 35(58.33) 21(35.59) PALBI[例(%)] χ2=19.532 <0.001 ≤-1.932 49(81.67) 25(42.37) >-1.932 11(18.33) 34(57.63) Ca(mmol/L) 2.02±0.13 2.09±0.15 t=2.677 0.008 TC(mmol/L) 2.92(2.47~3.51) 3.53(3.01~4.12) Z=-3.864 <0.001 TG(mmol/L) 0.95(0.70~1.24) 0.81(0.68~1.05) Z=-1.414 0.157 LDL(mmol/L) 1.63(1.20~2.03) 1.68(1.30~2.02) Z=-0.736 0.462 PT(s) 15.65(14.43~17.08) 15.10(13.50~16.50) Z=-1.789 0.074 APTT(s) 35.50±6.46 36.63±7.34 t=-0.894 0.373 TT(s) 18.15(16.73~19.85) 19.80(18.70~21.20) Z=-4.490 <0.001 AT-ⅢA(%) 62.55±14.99 52.42±18.03 t=3.329 0.001 表 2 影响肝硬化并食管胃底静脉曲张破裂出血的二元Logistic回归分析
Table 2. Binary Logistic regression analysis of factors affecting gastrointestinal bleeding in liver cirrhosis
变量 B值 SE Wald P值 OR 95%CI APRI -1.173 0.534 4.830 0.028 0.309 0.109~0.881 PALBI 2.037 0.684 8.857 0.003 7.667 2.005~29.327 Ca -7.100 2.622 7.335 0.007 0.001 0.000~0.141 TC -0.758 0.373 4.130 0.042 0.469 0.226~0.973 TT -0.512 0.166 9.516 0.002 0.599 0.433~0.830 AT-ⅢA 0.025 0.023 1.106 0.293 1.025 0.979~1.073 注:APRI≤0.597赋值为0,APRI>0.597赋值为1;PALBI>-1.932赋值为0,PALBI≤-1.932赋值为1。 -
[1] Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35( 11): 2408- 2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006.中华医学会肝病学分会. 肝硬化诊治指南[J]. 临床肝胆病杂志, 2019, 35( 11): 2408- 2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. [2] DENG H, QI X, PENG Y, et al. Diagnostic accuracy of APRI, AAR, FIB-4, FI, and King Scores for diagnosis of esophageal varices in liver cirrhosis: A retrospective study[J]. Med Sci Monit, 2015, 21: 3961- 3977. DOI: 10.12659/msm.895005. [3] WU X, ZHANG XJ, XUE Y, et al. Changes and clinical significance of blood antithrombin- and D-dimer levels in liver cirrhosis patients with gastrointestinal bleeding[J/CD]. Chin J Liver Dis: Electronic Edition, 2023, 15( 1): 56- 61. DOI: 10.3969/j.issn.1674-7380.2023.01.009.武幸, 张秀军, 薛源, 等. 肝硬化消化道出血患者血抗凝血酶Ⅲ和D-二聚体水平变化及临床意义[J/CD]. 中国肝脏病杂志(电子版), 2023, 15( 1): 56- 61. DOI: 10.3969/j.issn.1674-7380.2023.01.009. [4] LI DZ, LI J, GUO XL. Value of albumin-bilirubin score in predicting the prognosis of patients with liver cirrhosis and esophagogastric variceal bleeding[J]. J Clin Hepatol, 2021, 37( 5): 1085- 1090. DOI: 10.3969/j.issn.1001-5256.2021.05.022.李德钊, 李健, 郭晓林. 白蛋白-胆红素评分对肝硬化食管胃静脉曲张出血患者预后的预测价值[J]. 临床肝胆病杂志, 2021, 37( 5): 1085- 1090. DOI: 10.3969/j.issn.1001-5256.2021.05.022. [5] TANAKA K, TSUJI K, MATSUI T, et al. Potential of PALBI-T score as a prognostic model for hepatocellular carcinoma in alcoholic liver disease[J]. JGH Open, 2022, 6( 1): 36- 43. DOI: 10.1002/jgh3.12705. [6] GINÈS P, KRAG A, ABRALDES JG, et al. Liver cirrhosis[J]. Lancet, 2021, 398( 10308): 1359- 1376. DOI: 10.1016/S0140-6736(21)01374-X. [7] NIU SN, ZHAO JY, CHANG YF, et al. Application of monitored anesthesia care technique in emergency endoscopic treatment of liver cirrhosis patients with gastric varices bleeding[J/CD]. Chin J Liver Dis(Electronic Version), 2022, 14( 1): 67- 72. DOI: 10.3969/j.issn.1674-7380.2022.01.010.牛少宁, 赵金迎, 常宇飞, 等. 监护麻醉技术在急诊内镜下治疗肝硬化胃底静脉曲张破裂出血患者中的应用[J/CD]. 中国肝脏病杂志(电子版), 2022, 14( 1): 67- 72. DOI: 10.3969/j.issn.1674-7380.2022.01.010. [8] SINGAL AK, MATHURIN P. Diagnosis and treatment of alcohol-associated liver disease: A review[J]. JAMA, 2021, 326( 2): 165- 176. DOI: 10.1001/jama.2021.7683. [9] ZHANG XH, GUAN L, TIAN HY, et al. Risk factors and prevention of viral hepatitis-related hepatocellular carcinoma[J]. Front Oncol, 2021, 11: 686962. DOI: 10.3389/fonc.2021.686962. [10] MAI RY, WANG YY, BAI T, et al. Combination of ALBI and APRI to predict post-hepatectomy liver failure after liver resection for HBV-related HCC patients[J]. Cancer Manag Res, 2019, 11: 8799- 8806. DOI: 10.2147/CMAR.S213432. [11] WAI CT, GREENSON JK, FONTANA RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C[J]. Hepatology, 2003, 38( 2): 518- 526. DOI: 10.1053/jhep.2003.50346. [12] XIAO GQ, YANG JY, YAN LN. Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection: A systemic review and meta-analysis[J]. Hepatology, 2015, 61( 1): 292- 302. DOI: 10.1002/hep.27382. [13] SHRIVASTAVA R, SEN S, BANERJI D, et al. Assessment of non-invasive models for liver fibrosis in chronic hepatitis B virus related liver disease patients in resource limited settings[J]. Indian J Pathol Microbiol, 2013, 56( 3): 196- 199. DOI: 10.4103/0377-4929.120359. [14] IACOB DG, LUMINOS M, BENEA OE, et al. Liver fibrosis progression in a cohort of young HIV and HIV/HBV co-infected patients: A longitudinal study using non-invasive APRI and Fib-4 scores[J]. Front Med, 2022, 9: 888050. DOI: 10.3389/fmed.2022.888050. [15] KANG NL, RUAN QF, ZHANG DS, et al. Advantages of a novel model for predicting hepatic fibrosis in chronic hepatitis B virus carriers compared with APRI and FIB-4 scores[J]. J Clin Transl Hepatol, 2022, 10( 3): 412- 419. DOI: 10.14218/JCTH.2022.00098. [16] MORISHITA N, HIRAMATSU N, OZE T, et al. Liver stiffness measurement by acoustic radiation force impulse is useful in predicting the presence of esophageal varices or high-risk esophageal varices among patients with HCV-related cirrhosis[J]. J Gastroenterol, 2014, 49( 7): 1175- 1182. DOI: 10.1007/s00535-013-0877-z. [17] WANG JH, CHUAH SK, LU SN, et al. Transient elastography and simple blood markers in the diagnosis of esophageal varices for compensated patients with hepatitis B virus-related cirrhosis[J]. J Gastroenterol Hepatol, 2012, 27( 7): 1213- 1218. DOI: 10.1111/j.1440-1746.2012.07132.x. [18] YANG L, KAN QX, GAO J. Relationship between PALBI, MELD, INR and the prognosis of patients with liver cirrhosis combined with upper gastrointestinal hemorrhage and a multivariate study[J]. J Clin Exp Med, 2022, 21( 11): 1137- 1141. DOI: 10.3969/j.issn.1671-4695.2022.11.005.杨磊, 阚全香, 高杰. PALBI、MELD及INR值与肝硬化患者合并上消化道出血患者预后的关系及多因素研究[J]. 临床和实验医学杂志, 2022, 21( 11): 1137- 1141. DOI: 10.3969/j.issn.1671-4695.2022.11.005. -



 PDF下载 ( 918 KB)
PDF下载 ( 918 KB)

 下载:
下载:






