1990—2019年中国肝硬化疾病负担变化趋势分析
DOI: 10.12449/JCH240414
Changing trend of the disease burden of liver cirrhosis in China from 1990 to 2019
-
摘要:
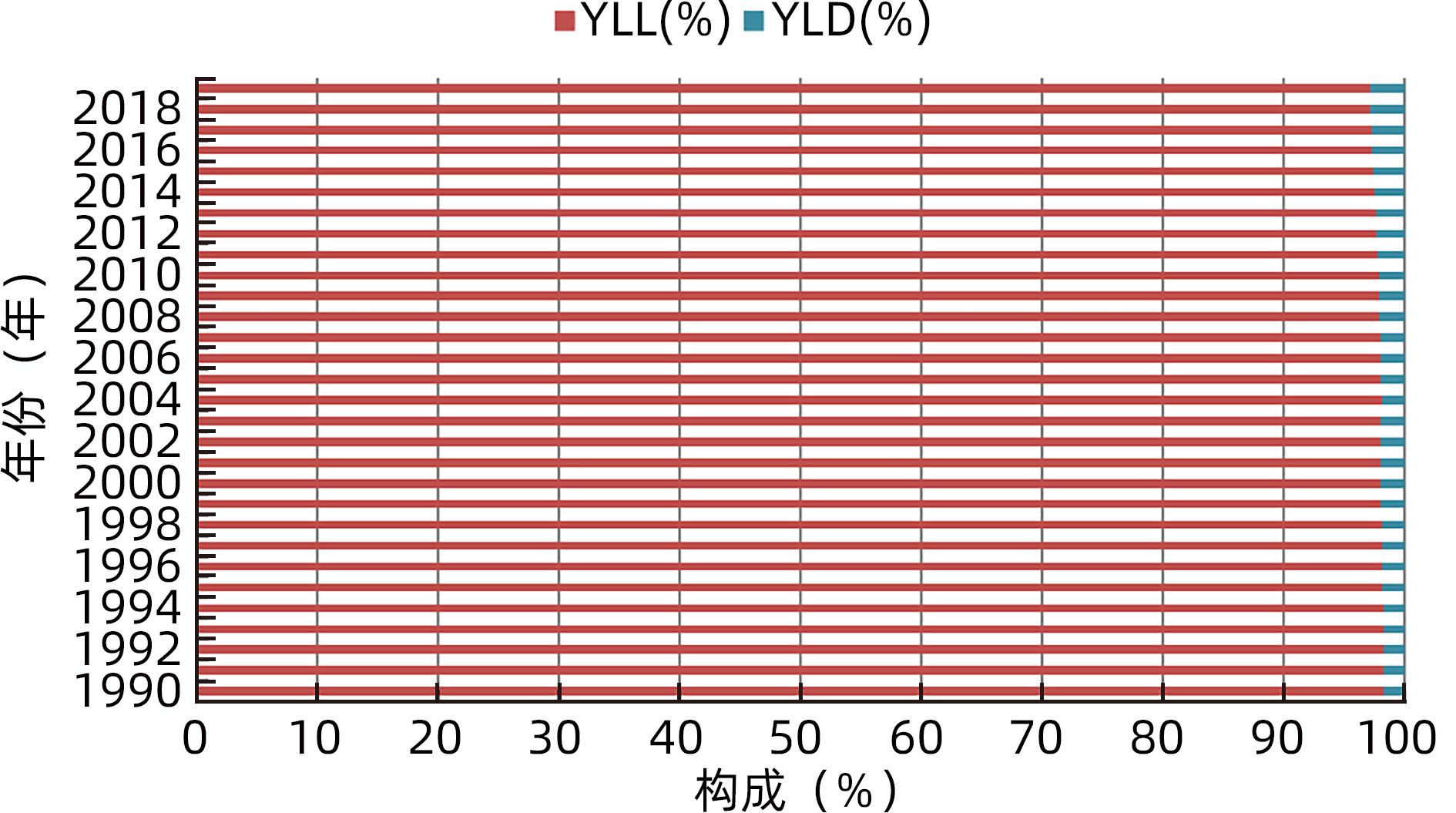
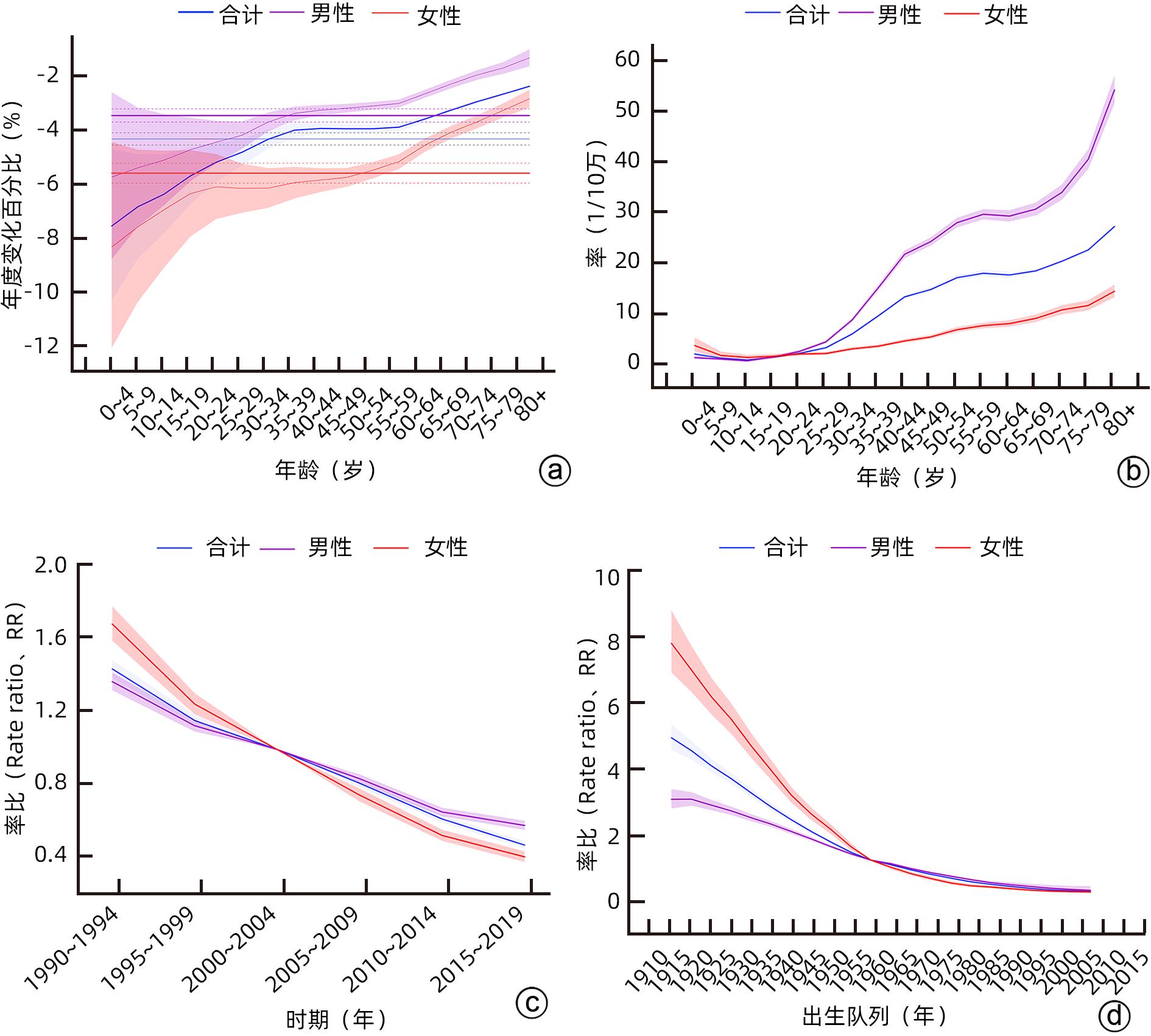
目的 分析1990—2019年中国人群肝硬化流行情况和疾病负担变化趋势,为中国肝硬化防治策略的制定提供数据参考。 方法 从2019年全球疾病负担(GBD 2019)收集整理1990—2019年中国肝硬化发病、死亡、伤残调整寿命年(DALY)、过早死亡损失寿命年(YLL)、伤残损失寿命年(YLD)等疾病负担数据,使用Joinpoint回归模型分析其疾病负担变化趋势,使用年龄-时期-队列(APC)模型评估年龄、时期和队列效应,使用R软件BAPC包预测未来疾病负担变化情况。 结果 与1990年相比,2019年中国总体、男性和女性人群肝硬化发病例数和患病例数均有所上升,而死亡例数有所下降。1990—2019年中国人群肝硬化标化发病率、标化患病率和标化死亡率均呈下降趋势,平均每年分别下降0.62%(95%CI:-0.74%~-0.50%,t=9.99,P<0.001)、0.44%(95%CI:-0.53%~-0.35%,t=13.18,P<0.001)和3.02%(95%CI:-3.12%~-2.93%,t=7.58,P<0.001)。1990—2019年中国人群肝硬化标化DALY率、YLL率和YLD率均呈下降趋势,平均每年分别下降3.27%(95%CI:-3.37%~-3.18%,t=6.22,P<0.001)、3.32%(95%CI:-3.42%~-3.22%,t=9.31,P<0.001)和1.42%(95%CI:-1.49%~-1.34%,t=4.93,P<0.001)。1990—2019年中国人群肝硬化发病率随年龄增长呈先上升后下降趋势,死亡率呈上升趋势;发病风险和死亡风险随时间和出生队列推移均呈现下降趋势。预测模型显示,2020—2030年中国肝硬化造成的标化发病率、患病率、死亡率和DALY率均呈下降趋势。男性和女性最主要的危险因素均是酒精,其次是药物。 结论 1990—2019年中国肝硬化疾病负担呈下降趋势,且存在性别和年龄差异,中年男性人群是肝硬化疾病负担的重点人群,应采取有效措施进行干预。 Abstract:Objective To investigate the prevalence of liver cirrhosis and the changing trend of the disease burden of liver cirrhosis in the Chinese population from 1990 to 2019, and to provide a data reference for formulating the prevention and treatment strategies for liver cirrhosis in China. Methods The Global Burden of Disease Study 2019 was used to collect the data on the incidence rate, mortality rate, disability-adjusted life years (DALY), years of life lost (YLL), and years lived with disability (YLD) of liver cirrhosis. The Joinpoint regression model was used to analyze the changing trend of disease burden; the age-period-cohort (APC) model was used to evaluate age, period, and cohort effects; R software BAPC package was used to predict future changes in disease burden. Results From 1990 to 2019 in China, there were increases in the numbers of liver cirrhosis cases and prevalent cases in the general population, as well as in the male and female populations, while there was a reduction in the number of deaths. From 1990 to 2019, the standardized incidence rate, standardized prevalence rate, and standardized mortality rate of liver cirrhosis in the Chinese population showed a downward trend, with a mean annual reduction of 0.62% (95% confidence interval [CI]: -0.74% to -0.50%, t=9.99, P<0.001), 0.44% (95%CI: -0.53% to -0.35%, t=13.18, P<0.001), and 3.02% (95%CI: -3.12% to -2.93%, t=7.58, P<0.001), respectively. From 1990 to 2019, the standardized DALY, YLL, and YLD rates of liver cirrhosis in the Chinese population also showed a downward trend, with a mean annual reduction of 3.27% (95%CI: -3.37% to -3.18%, t=6.22, P<0.001), 3.32% (95%CI: -3.42% to -3.22%, t=9.31, P<0.001), and 1.42% (95%CI: -1.49% to -1.34%, t=4.93, P<0.001), respectively. From 1990 to 2019, the incidence rate of liver cirrhosis in the Chinese population first increased and then decreased with age, while the mortality rate showed an increasing trend, and the risks of disease onset and death showed a decreasing trend with time and birth cohort. The predictive model showed that the standardized incidence rate, prevalence rate, mortality rate, and DALY rate of liver cirrhosis in China will show a decreasing trend from 2020 to 2030. Alcohol was the most important risk factor for both male and female populations, followed by medication. Conclusion The disease burden of liver cirrhosis in China shows a decreasing trend from 1990 to 2019, with sex and age differences, especially in the middle-aged male population. Effective measures should be taken for intervention. -
Key words:
- Liver cirrhosis /
- Cost of Illness /
- Forecasting /
- China
-
表 1 1990年和2019年中国肝硬化发病、患病和死亡流行情况
Table 1. Epidemic situation of liver cirrhosis incidence, prevalence, and mortality in China in 1990 and 2019
组别 病例数及95%CI(×105) 粗率及95%CI(1/10万) 标化率及95%CI(1/10万) 1990年 2019年 1990年 2019年 AAPC 1990年 2019年 AAPC 发病 男 1.93 (1.36~2.53) 2.46 (1.81~3.11) 31.60 (22.21~41.51) 33.38 (24.96~42.88) 0.261) (0.11~0.40) 31.51 (21.45~41.77) 27.49 (21.00~34.13) -0.461) (-0.57~-0.34) 女 1.17 (0.87~1.49) 1.64 (1.26~2.06) 20.47 (15.17~26.04) 23.53 (17.99~29.53) 0.49 (0.39~0.60) 22.16 (16.18~28.74) 17.30 (13.69~21.46) -0.841) (-0.98~-0.70) 合计 3.10 (2.24~3.99) 4.10 (3.08~5.14) 26.21 (18.95~33.75) 28.80 (21.67~36.16) 0.341) (0.21~0.47) 27.01 (19.08~35.23) 22.46 (17.56~27.59) -0.621) (-0.74~-0.50) 患病 男 1 696.61 (1 559.05~1 825.14) 2 411.17 (2 232.71~2 608.07) 27 809.61 (25 550.37~29 911.23) 33 265.74 (30 803.61~35 982.27) 0.601) (0.54~0.67) 29 089.68 (26 950.72~31 191.98) 26 654.11 (24 649.46~28 814.63) -0.321) (-0.39~-0.24) 女 1 328.43 (1 225.20~2 068.62) 1 868.66 (1 713.65~2 068.62) 23 163.84 (21 363.76~25 079.75) 26 789.77 (24 567.43~29 656.42) 0.541) (0.39~0.70) 24 399.14 (22 561.81~26 407.65) 20 409.60 (18 709.74~22 449.43) -0.551) (-0.73~-0.36) 合计 3 025.34 (2 789.66~3 262.05) 4 279.83 (3 955.16~4 652.38) 25 558.73 (23 567.62~27 558.50) 30 089.89 (27 807.21~32 709.07) 0.581) (0.50~0.67) 26 805.60 (24 822.53~28 828.76) 23 561.25 (21 807.83~25 635.19) -0.441) (-0.53~-0.35) 死亡 男 1.12 (0.91~1.33) 1.10 (0.88~1.36) 18.37 (14.93~21.86) 15.17 (12.16~18.78) -0.691) (-0.76~-0.62) 25.01 (20.47~29.56) 11.85 (9.63~14.42) -2.591) (-2.68~-2.50) 女 0.56 (0.45~0.66) 0.42 (3.39~5.20) 9.69 (7.81~11.50) 6.06 (4.86~7.46) -1.63 (-1.75~-1.50) 12.92 (10.51~15.18) 4.20 (3.37~5.15) -3.821) (-3.95~-3.69) 合计 1.68 (1.44~1.92) 1.52 (1.28~1.80) 14.17 (12.18~16.20) 10.70 (9.01~12.64) -0.991) (-1.13~-0.85) 18.89 (16.53~21.46) 7.81 (6.62~9.16) -3.021) (-3.12~-2.93) 注:1),P<0.05。AAPC,平均年度变化百分比。 表 2 1990-2019年中国肝硬化疾病负担流行情况
Table 2. Epidemic situation of liver cirrhosis disease burden in China from 1990 to 2019
组别 粗率及95%CI(1/10万) 标化率及95%CI(1/10万) 1990年 2019年 AAPC 1990年 2019年 AAPC DALY 男 657.97 (532.01~784.02) 458.83 (363.98~569.17) -1.27 (-1.35~-1.19)1) 776.28 (632.13~922.04) 337.02 (269.40~415.58) -2.87 (-2.97~-2.78)1) 女 293.54 (233.17~349.59) 145.85 (117.21~180.36) -2.41 (-2.58~-2.23)1) 353.06 (283.27~418.99) 100.50 (80.78~124.00) -4.26 (-4.39~-4.13)1) 合计 481.40 (412.00~552.59) 305.34 (255.95~361.80) -1.60 (-1.68~-1.52)1) 570.18 (489.60~653.76) 217.77 (183.43~256.92) -3.27 (-3.37~-3.18)1) YLL 男 647.45 (521.62~773.43) 447.45 (352.26~557.30) -1.30 (-1.38~-1.22)1) 763.99 (618.62~910.22) 328.49 (260.78~406.67) -2.91 (-3.01~-2.81)1) 女 287.76 (226.28~343.87) 140.31 (110.93~174.63) -2.48 (-2.65~-2.30)1) 346.36 (275.31~411.62) 96.37 (76.48~119.96) -4.34 (-4.48~-4.20)1) 合计 473.18 (404.50~545.34) 296.83 (247.70~353.81) -1.64 (-1.72~-1.56)1) 560.61 (478.58~645.16) 211.46 (177.14~251.25) -3.32 (-3.42~-3.22)1) YLD 男 10.52 (7.06~15.28) 11.37 (7.69~16.44) 0.28 (0.22~0.34)1) 12.29 (8.25~17.85) 8.53 (5.72~12.25) -1.25 (-1.30~-1.19)1) 女 5.77 (3.71~7.93) 5.54 (3.71~7.93) -0.14 (-0.26~-0.01)1) 6.70 (4.53~9.67) 4.12 (2.79~5.88) -1.64 (-1.78~-1.49)1) 合计 8.22 (5.76~12.16) 8.51 (5.76~12.16) 0.13 (0.08~0.18)1) 9.58 (6.46~13.96) 6.32 (4.24~9.06) -1.42 (-1.49~-1.34)1) 注:1)P<0.001。 表 3 1990-2019年中国肝硬化疾病负担预测模型拟合
Table 3. Fitting of the Prediction Model for the Burden of Liver Cirrhosis in China from 1990 to 2019
指标 方误差 平均绝对误差 平均绝对百分误差(%) 拟合精度(%) 标化发病率 0.023 4 0.121 1 0.541 7 99.458 3 标化患病率 28 700.474 9 143.026 9 0.604 2 99.395 8 标化死亡率 0.005 3 0.059 3 0.678 5 99.321 5 标化DALY率 5.233 8 1.769 4 0.7616 99.238 4 表 4 2020-2030年中国肝硬化疾病负担预测情况
Table 4. Prediction of the Burden of Liver Cirrhosis in China from 2020 to 2030
年份 标化发病率及95%CI (1/10万) 标化患病率及95%CI (1/10万) 标化死亡率及95%CI(1/10万) 标化DALY率及95%CI (1/10万) 2020 22.32(22.13~22.52) 22 922.43(22 737.44~23 107.43) 7.63(7.45~7.82) 214.10(208.96~219.23) 2021 22.21(21.63~22.78) 22 463.17(21 953.43~22 972.91) 7.33(6.96~7.70) 209.79(197.49~222.10) 2022 22.12(21.06~23.17) 22 161.06(21 319.50~23 002.63) 6.90(6.35~7.44) 201.08(180.37~221.79) 2023 22.05(20.42~23.67) 21 941.05(20 812.88~23 069.21) 6.36(5.68~7.04) 192.94(165.08~220.81) 2024 22.00(19.73~24.27) 21 745.21(20 382.61~23 107.82) 5.76(4.99~6.52) 182.42(147.50~217.34) 2025 21.98(19.00~24.96) 21 545.95(19 990.06~23 101.83) 5.13(4.34~5.93) 172.68(131.63~213.73) 2026 21.98(18.23~25.73) 21 336.59(19 615.40~23 057.79) 4.54(3.74~5.35) 161.56(114.65~208.47) 2027 22.00(17.43~26.58) 21 119.58(19 251.16~22 988.00) 4.02(3.22~4.82) 151.12(98.98~203.25) 2028 22.05(16.60~27.50) 20 898.97(18 895.32~22 902.62) 3.58(2.77~4.39) 139.83(82.72~196.94) 2029 22.12(15.74~28.50) 20 677.52(18 547.28~22 807.76) 3.23(2.41~4.06) 129.06(67.41~190.72) 2030 22.21(14.85~29.57) 20 456.41(18 206.43~22 706.39) 2.96(2.11~3.81) 117.75(51.76~183.75) -
[1] PAROLA M, PINZANI M. Liver fibrosis: Pathophysiology, pathogenetic targets and clinical issues[J]. Mol Aspects Med, 2019, 65: 37- 55. DOI: 10.1016/j.mam.2018.09.002. [2] DEVARBHAVI H, ASRANI SK, ARAB JP, et al. Global burden of liver disease: 2023 update[J]. J Hepatol, 2023, 79( 2): 516- 537. DOI: 10.1016/j.jhep.2023.03.017. [3] XU XY, DING HG, LI WG, et al. Chinese guidelines on the management of liver cirrhosis(abbreviated version)[J]. World J Gastroenterol, 2020, 26( 45): 7088- 7103. DOI: 10.3748/wjg.v26.i45.7088. [4] HUANG DQ, MATHURIN P, CORTEZ-PINTO H, et al. Global epidemiology of alcohol-associated cirrhosis and HCC: Trends, projections and risk factors[J]. Nat Rev Gastroenterol Hepatol, 2023, 20( 1): 37- 49. DOI: 10.1038/s41575-022-00688-6. [5] HUANG DQ, TERRAULT NA, TACKE F, et al. Global epidemiology of cirrhosis- aetiology, trends and predictions[J]. Nat Rev Gastroenterol Hepatol, 2023, 20( 6): 388- 398. DOI: 10.1038/s41575-023-00759-2. [6] 2019 VIEWPOINT COLLABORATORS GBD. Five insights from the Global Burden of Disease Study 2019[J]. Lancet, 2020, 396( 10258): 1135- 1159. DOI: 10.1016/S0140-6736(20)31404-5. [7] 2019 RISK FACTORS COLLABORATORS GBD. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019[J]. Lancet, 2020, 396( 10258): 1223- 1249. DOI: 10.1016/S0140-6736(20)30752-2. [8] KIM HJ, FAY MP, FEUER EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates[J]. Stat Med, 2000, 19( 3): 335- 351. DOI: 3.0.co;2-z">10.1002/(sici)1097-0258(20000215)19: 3<335: aid-sim336>3.0.co;2-z. [9] LI HZ, DU LB. Application of Joinpoint regression model in cancer epidemiological time trend analysis[J]. Chin J Prev Med, 2020, 54( 8): 908- 912. DOI: 10.3760/cma.j.cn112150-20200616-00889.李辉章, 杜灵彬. Joinpoint回归模型在肿瘤流行病学时间趋势分析中的应用[J]. 中华预防医学杂志, 2020, 54( 8): 908- 912. DOI: 10.3760/cma.j.cn112150-20200616-00889. [10] XU D, HU JC, WANG SY, et al. Trends in the prevalence of hypertensive heart disease in China from 1990 to 2019: A joinpoint and age-period-cohort analysis[J]. Front Public Health, 2022, 10: 833345. DOI: 10.3389/fpubh.2022.833345. [11] ZHENG RS, CHEN WQ. Introduction of age-period-queue prediction model based on Bayesian method[J]. Chin J Prev Med, 2012, 46( 7): 648- 650. DOI: 10.3760/cma.j.issn.0253-9624.2012.07.016.郑荣寿, 陈万青. 基于贝叶斯方法的年龄-时期-队列预测模型的介绍[J]. 中华预防医学杂志, 2012, 46( 7): 648- 650. DOI: 10.3760/cma.j.issn.0253-9624.2012.07.016. [12] ROSENBERG PS. A new age-period-cohort model for cancer surveillance research[J]. Stat Methods Med Res, 2019, 28( 10-11): 3363- 3391. DOI: 10.1177/0962280218801121. [13] HUA SM. Application and development of“age-period-queue” effect model[J]. China CIO Issues, 2019( 9): 73- 74. DOI: 10.3969/j.issn.1001-2362.2019.09.046.华淑名.“年龄-时期-队列” 效应模型的应用与发展[J]. 信息系统工程, 2019( 9): 73- 74. DOI: 10.3969/j.issn.1001-2362.2019.09.046. [14] 2017 CIRRHOSIS COLLABORATORS GBD. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet Gastroenterol Hepatol, 2020, 5( 3): 245- 266. DOI: 10.1016/S2468-1253(19)30349-8. [15] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association, et al. Guidelines for the prevention and treatment of chronic hepatitis B(version 2022)[J]. J Pract Hepatol, 2023, 26( 3): 457- 478. DOI: 10.3969/j.issn.1007-8134.2023.01.01.中华医学会肝病学分会, 中华医学会感染病学分会. 慢性乙型肝炎防治指南(2022年版)[J]. 实用肝脏病杂志, 2023, 26( 3): 457- 478. DOI: 10.3969/j.issn.1007-8134.2023.01.01. [16] LIU ZH, LIANG XE, HOU JL. Thoughts on expert opinion on expanding antiviral therapy for chronic hepatitis B[J]. J Clin Hepatol, 2023, 39( 1): 14- 21. DOI: 10.3969/j.issn.1001-5256.2023.01.002.刘智泓, 梁携儿, 侯金林. 关于《扩大慢性乙型肝炎抗病毒治疗的专家意见》的几点思考[J]. 临床肝胆病杂志, 2023, 39( 1): 14- 21. DOI: 10.3969/j.issn.1001-5256.2023.01.002. [17] WANG GS, XIE W, WAN G, et al. Diseases spectrum changes of inpatients with liver diseases in a general hospital during 15 years[J/OL]. Chin J Exp Clin Infect Dis Electron Ed, 2021, 15( 1): 29- 36. DOI: 10.3877/cma.j.issn.1674-1358.2021.01.006.王桂爽, 谢雯, 万钢, 等. 某综合医院15年间肝病住院患者疾病谱变化分析[J/OL]. 中华实验和临床感染病杂志(电子版), 2021, 15( 1): 29- 36. DOI: 10.3877/cma.j.issn.1674-1358.2021.01.006. [18] CHEN QQ, RUI FJ, NI WJ, et al. Research progress in epidemiology and risk factors of primary liver cancer[J]. Chin Gen Pract, 2024, 27( 6): 637- 642. DOI: 10.12114/j.issn.1007-9572.2023.0479.陈倩倩, 芮法娟, 倪文婧, 等. 原发性肝癌的流行病学及其危险因素研究进展[J]. 中国全科医学, 2024, 27( 6): 637- 642. DOI: 10.12114/j.issn.1007-9572.2023.0479. [19] LI YR, WANG M, HE FL, et al. Etiological and non-etiological therapies for cirrhotic portal hypertension[J]. J Clin Hepatol, 2022, 38( 6): 1224- 1228. DOI: 10.3969/j.issn.1001-5256.2022.06.003.李悦榕, 王民, 何福亮, 等. 肝硬化门静脉高压的病因和非病因治疗[J]. 临床肝胆病杂志, 2022, 38( 6): 1224- 1228. DOI: 10.3969/j.issn.1001-5256.2022.06.003. [20] FALLOWFIELD JA, JIMENEZ-RAMOS M, ROBERTSON A. Emerging synthetic drugs for the treatment of liver cirrhosis[J]. Expert Opin Emerg Drugs, 2021, 26( 2): 149- 163. DOI: 10.1080/14728214.2021.1918099. [21] PATEL R, MUELLER M. Alcoholic Liver Disease[EB/OL].( 2023-7-23). https://www.ncbi.nlm.nih.gov/books/NBK546632/. https://www.ncbi.nlm.nih.gov/books/NBK546632/ [22] WANG SY, DONG C, CHANG CD, et al. Opportunities and challenges of surveillance for liver cancer in primary care institutions in China[J]. Chin Gen Pract, 2023, 26( 36): 4498- 4504, 4520. DOI: 10.12114/j.issn.1007-9572.2023.0337.王世越, 董晨, 常楚迪, 等. 中国原发性肝癌基层筛查的机遇与挑战[J]. 中国全科医学, 2023, 26( 36): 4498- 4504, 4520. DOI: 10.12114/j.issn.1007-9572.2023.0337. [23] TONG YN, ZHENG JM, HAN D, et al. Analysis of etiology and clinical characteristics in 986 patients with liver cirrhosis[J]. Chin Hepatol, 2022, 27( 8): 871- 873, 880. DOI: 10.14000/j.cnki.issn.1008-1704.2022.08.008.佟印妮, 郑吉敏, 韩丹, 等. 986例肝硬化患者病因及临床特点分析[J]. 肝脏, 2022, 27( 8): 871- 873, 880. DOI: 10.14000/j.cnki.issn.1008-1704.2022.08.008. [24] LIN Y. Epidemiological Analysis of the Etiology of Cirrhosis in Central China[D]. Wuhan: Huazhong University of Science and Technology, 2022.林易. 华中地区肝硬化病因的流行病学变化趋势分析: 单中心研究[D]. 武汉: 华中科技大学, 2022. [25] HUANG DQ, MATHURIN P, CORTEZ-PINTO H, et al. Global epidemiology of alcohol-associated cirrhosis and HCC: Trends, projections and risk factors[J]. Nat Rev Gastroenterol Hepatol, 2023, 20( 1): 37- 49. DOI: 10.1038/s41575-022-00688-6. [26] ZHOU EH. The Effect of Drinking on the Progress of Hepatitis B to Cirrhosis[D]. Chongqing: Chongqing Medical University, 2021.周恩豪. 饮酒对慢乙肝进展为肝硬化的研究[D]. 重庆: 重庆医科大学, 2021. [27] BUZZETTI E, PARIKH PM, GERUSSI A, et al. Gender differences in liver disease and the drug-dose gender gap[J]. Pharmacol Res, 2017, 120: 97- 108. DOI: 10.1016/j.phrs.2017.03.014. [28] YUE TT, ZHANG QQ, CAI T, et al. Trends in the disease burden of HBV and HCV infection in China from 1990-2019[J]. Int J Infect Dis, 2022, 122: 476- 485. DOI: 10.1016/j.ijid.2022.06.017. [29] LIU YB, CHEN MK. Epidemiology of liver cirrhosis and associated complications: Current knowledge and future directions[J]. World J Gastroenterol, 2022, 28( 41): 5910- 5930. DOI: 10.3748/wjg.v28.i41.5910. -



 PDF下载 ( 1660 KB)
PDF下载 ( 1660 KB)


 下载:
下载: