肝昏迷患者经人工肝治疗后成功行跨血型肝移植1例报告
DOI: 10.12449/JCH240423
伦理学声明:本例报告已获得患者知情同意。
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:孙爽负责课题设计,资料分析,撰写论文;刘金泉、冯帅、王淑贤、徐祥美、戴德淑负责课题设计;王建红、蔡金贞负责拟定写作思路;许传屾负责指导撰写文章并最后定稿。
Successful trans-blood liver transplantation after artificial liver support therapy in a patient with hepatic coma: A case report
-
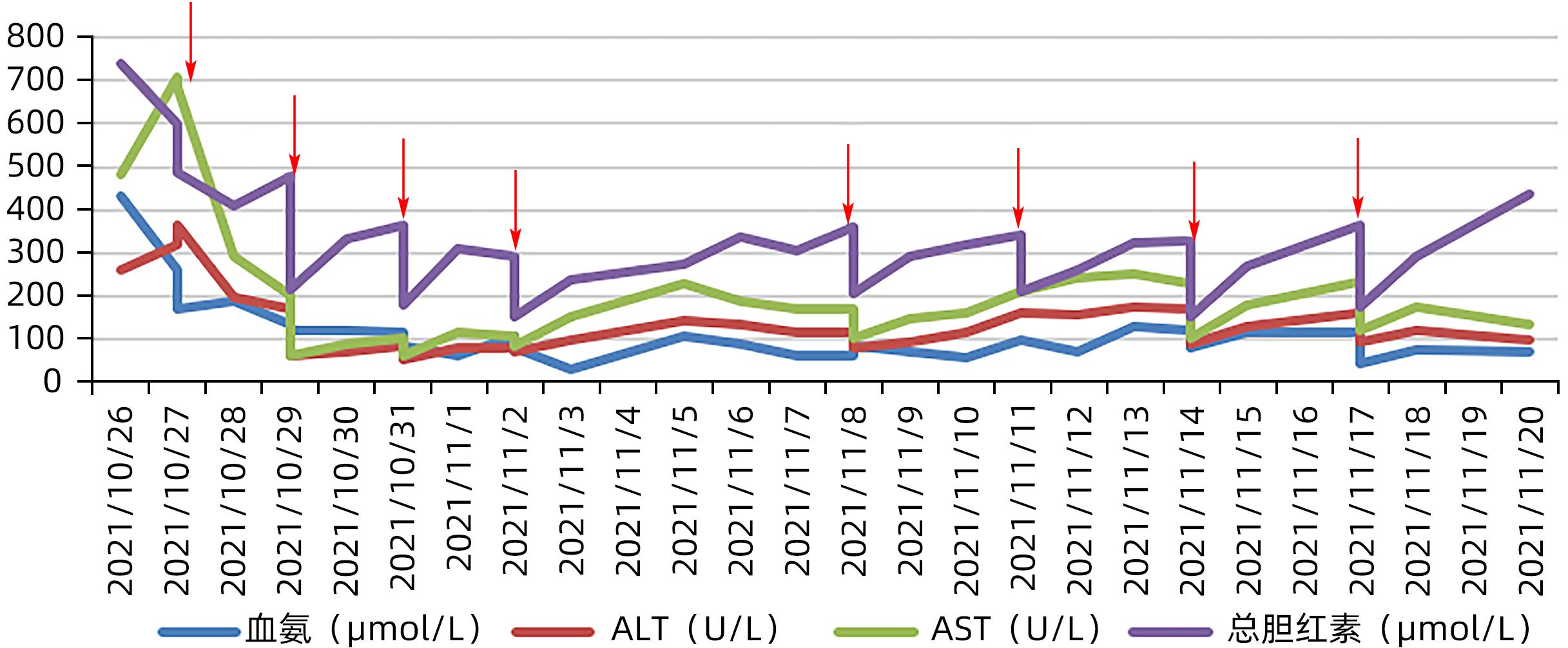
Abstract: This article reports a patient with hepatic coma who underwent artificial liver support therapy and liver transplantation successfully, and the patient recovered well in the later stage after active treatment. This article also discusses the timing of liver transplantation.
-
Key words:
- Liver Transplantation /
- Liver Failure /
- Liver, Artificial
-
-
[1] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [2] WU CB, ZHOU MX, MENG Y, et al. Application and research progress of non-bioartificial liver[J]. Biomed Eng Clin Med, 2021, 25( 5): 634- 638. DOI: 10.13339/j.cnki.sglc.20210820.009.吴春波, 周明雪, 孟彦, 等. 非生物型人工肝的应用及研究进展[J]. 生物医学工程与临床, 2021, 25( 5): 634- 638. DOI: 10.13339/j.cnki.sglc.20210820.009. [3] CHEN MJ, LI X, TANG SH. Advances in multi-dimensional assessment of liver function in the prognosis of patients with liver failure[J]. Clin J Med Offic, 2023, 51( 9): 901- 903, 907. DOI: 10.16680/j.1671-3826.2023.09.05.陈美娟, 李雪, 汤善宏. 多维度评估肝功能在肝衰竭患者预后中研究进展[J]. 临床军医杂志, 2023, 51( 9): 901- 903, 907. DOI: 10.16680/j.1671-3826.2023.09.05. [4] ARTRU F, LOUVET A, RUIZ I, et al. Liver transplantation in the most severely ill cirrhotic patients: A multicenter study in acute-on-chronic liver failure grade 3[J]. J Hepatol, 2017, 67( 4): 708- 715. DOI: 10.1016/j.jhep.2017.06.009. [5] KAMATH PS, WIESNER RH, MALINCHOC M, et al. A model to predict survival in patients with end-stage liver disease[J]. Hepatology, 2001, 33( 2): 464- 470. DOI: 10.1053/jhep.2001.22172. [6] MARTIN P, DIMARTINI A, FENG S, et al. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation[J]. Hepatology, 2014, 59( 3): 1144- 1165. DOI: 10.1002/hep.26972. [7] European Association for the Study of the Liver. EASL clinical practice guidelines: Liver transplantation[J]. J Hepatol, 2016, 64( 2): 433- 485. DOI: 10.1016/j.jhep.2015.10.006. [8] Hepatology Branch of the Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35( 11): 2408- 2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006.中华医学会肝病学分会. 肝硬化诊治指南[J]. 临床肝胆病杂志, 2019, 35( 11): 2408- 2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. [9] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of hepatic encephalopathy in cirrhosis[J]. J Clin Hepatol, 2018, 34( 10): 2076- 2089. DOI: 10.3969/j.issn.1001-5256.2018.10.007.中华医学会肝病学分会. 肝硬化肝性脑病诊疗指南[J]. 临床肝胆病杂志, 2018, 34( 10): 2076- 2089. DOI: 10.3969/j.issn.1001-5256.2018.10.007. [10] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of ascites and complications in cirrhosis[J]. J Clin Hepatol, 2017, 33( 10): 1847- 1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003.中华医学会肝病学分会. 肝硬化腹水及相关并发症的诊疗指南[J]. 临床肝胆病杂志, 2017, 33( 10): 1847- 1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003. [11] European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis[J]. J Hepatol, 2018, 69( 2): 406- 460. DOI: 10.1016/j.jhep.2018.03.024. [12] BOYER TD, SANYAL AJ, GARCIA-TSAO G, et al. Impact of liver transplantation on the survival of patients treated for hepatorenal syndrome type 1[J]. Liver Transpl, 2011, 17( 11): 1328- 1332. DOI: 10.1002/lt.22395. -



 PDF下载 ( 860 KB)
PDF下载 ( 860 KB)

 下载:
下载: