血清内皮细胞特异性分子1水平与肝硬化心肌病的相关性
DOI: 10.12449/JCH240614
Association between serum endothelial cell-specific molecule 1 and cirrhotic cardiomyopathy
-
摘要:
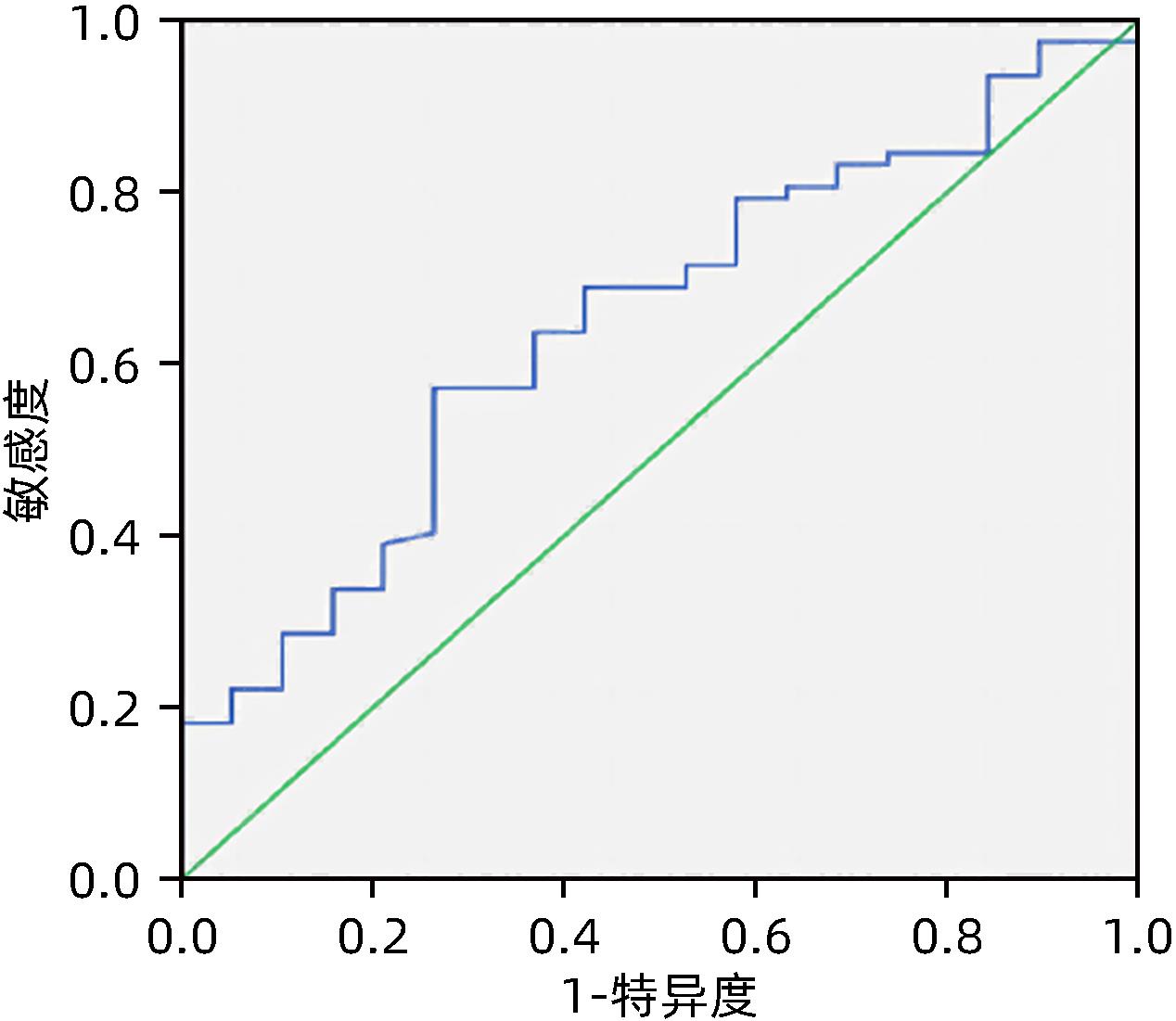
目的 肝硬化性心肌病(CCM)是肝硬化引起的心脏功能障碍和电生理紊乱,与肝硬化患者预后密切相关。血管内皮细胞特异性分子1(endocan)作为心血管疾病的诊断指标,是否参与CCM发病机制尚不明确。本研究拟检测CCM患者血清endocan的表达量及其与CCM的关系,推测在CCM发病中的可能作用。 方法 本研究为横断面研究,连续入组2019年1月—2021年1月首都医科大学附属北京佑安医院住院的肝硬化患者,根据有无CCM,分为CCM组(n=19)和无CCM组(n=106)。采用ELISA方法检测不同组血清endocan水平以及与肝功能、心脏功能的相关性。正态分布的计量资料两组间比较采用成组t检验,偏态分布的计量资料两组间比较采用Mann-Whitney U秩和检验。计数资料组间比较采用χ2检验。采用Pearson或Spearman相关分析进行相关性检验,应用受试者工作特征曲线(ROC曲线)评价CCM预测模型。 结果 CCM组患者血清endocan的表达量为[(2.69±0.43)ng/mL]明显高于无CCM组[(2.23±0.52)ng/mL](t=2.247,P=0.034)。在代偿期肝硬化患者血清endocan表达量[(2.41±0.37)ng/mL]显著低于失代偿期肝硬化组[(2.72±0.49)ng/mL](t=3.214,P=0.02)。CCM组患者血清endocan水平与肝功能Child-Pugh评分(r=0.509,P=0.026)、MELD-Na评分(r=0.484,P=0.036)呈正相关,与平均动脉压(r=-0.591,P=0.013)、二尖瓣舒张早期血流早峰值E波和舒张晚期血流峰值A波(E/A)比值(r=-0.515,P=0.042)呈负相关。血清endocan预测CCM的ROC曲线下面积为0.658(95%CI:0.522~0.781),当截断值为2.61 ng/mL时,敏感度为67.1%,特异度为73.7%。 结论 血清endocan与CCM的发生具有一定相关性,可能参与了CCM的发病机制。 -
关键词:
- 肝硬化 /
- 心肌疾病 /
- 内皮细胞特异性分子1
Abstract:Objective Cirrhotic cardiomyopathy (CCM) refers to cardiac dysfunction and electrophysiological disorder caused by liver cirrhosis and is closely associated with the prognosis of patients with liver cirrhosis. Endothelial cell-specific molecule 1 (endocan) can be used as a diagnostic marker for cardiovascular diseases, and it remains unclear whether it is involved in the pathogenesis of CCM. The aim of this study is to investigate the expression of serum endocan in patients with CCM and its possible role in the development of CCM. Methods This cross-sectional study was conducted among the patients with liver cirrhosis who were consecutively admitted to Beijing YouAn Hospital, Capital Medical University, from January 2019 to January 2021, and according to the presence or absence of CCM, the patients were divided into CCM group with 19 patients and non-CCM group with 106 patients. ELISA was used to measure the serum level of endocan, and its correlation with liver function and cardiac function was analyzed. The independent-samples t test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U rank sum test was used for comparison of continuous data with skewed distribution between two groups; the chi-square test was used for comparison of categorical data between groups. A Pearson or Spearman correlation analysis was used to investigate the correlation between indicators, and the receiver operating characteristic (ROC) curve was used to assess the CCM predictive model. Results The CCM group had a significantly higher expression level of serum Endocan than the non-CCM group (2.69±0.43 ng/mL vs 2.23±0.52 ng/mL, t=2.247, P=0.034). The patients with compensated cirrhosis had a significantly lower expression level of serum endocan than those with decompensated cirrhosis (2.41±0.37 ng/mL vs 2.72±0.49 ng/mL, t=3.214, P=0.02). In the CCM group, the serum level of endocan was positively correlated with Child-Pugh score (r=0.509, P=0.026) and MELD-Na score (r=0.484, P=0.036) and was negatively correlated with mean arterial pressure (r=-0.591, P=0.013) and mitral ratio of peak early to late diastolic filling velocity (r=-0.515, P=0.042). The serum endocan had an area under the ROC curve of 0.658 (95%CI: 0.522~0.781) in predicting CCM, when the cut-off value was 2.61 ng/mL, the sensitivity was 67.1% and the specificity was 73.7%. Conclusion There is a certain association between serum endocan and CCM, and serum endocan may be involved in the pathogenesis of CCM. -
Key words:
- Liver Cirrhosis /
-
Cardiomyopathies / - Endocan
-
表 1 肝硬化CCM组及无CCM组患者一般资料比较
Table 1. Comparison of general data between CCM and no-CCM
项目 CCM组(n=19) 无CCM组(n=106) 统计值 P值 男性[例(%)] 12(63.2) 71(67.0) χ2=2.834 0.632 年龄(岁) 58.0±9.1 56.2±8.8 t=0.536 0.335 肝硬化病因[例(%)] χ2=2.534 0.894 HBV 5(26.3) 36(34.0) HCV 9(47.4) 42(39.6) 原发性胆汁性胆管炎 1(5.3) 6(5.7) 药物性肝损伤 4(21.1) 22(20.8) 平均动脉压(mmHg) 89.7±11.0 87.0±9.8 t=0.043 0.291 心率(次/min) 76.3±13.9 76.3±13.8 t=0.125 0.993 Child-Pugh分级[例(%)] χ2=-2.134 0.172 A级 12(63.2) 50(47.2) B级 4(21.1) 39(36.8) C级 3(15.8) 17(16.0) MELD评分(分) 6(5~7) 6(5~10) Z=-3.345 0.593 MELD-Na评分(分) 8.1(5.1~10.2) 7.5(4.7~11.2) Z=-1.236 0.744 ALT(U/L) 39.1(29.5~57.1) 25.8(15.4~38.5) Z=-0.232 0.552 AST(U/L) 29.0(25.8~84.0) 39.1(29.2~57.1) Z=-0.134 0.361 白蛋白(g/L) 31.4±0.5 31.8±0.2 t=0.123 0.762 总胆红素(μmol/L) 25.9(18.4~33.7) 31.9(17.9~50.0) Z=-1.207 0.335 肌酐(μmol/L) 59.3±0.5 62.1±0.23 t=0.042 0.553 尿素氮(mmol/L) 4.4(3.8~5.7) 5.2(4.1~6.3) Z=-1.356 0.191 国际标准化比值 1.2(1.1~1.5) 13.(1.2~1.5) Z=-2.237 0.493 腹水[例(%)] 8(42.1) 64(60.4) χ2=0.018 0.227 自发性腹膜炎[例(%)] 3(15.8) 13(12.3) χ2=0.346 0.961 肝性脑病[例(%)] 1(5.3) 14(13.2) χ2=1.235 0.554 食管静脉曲张[例(%)] 10(52.6) 70(66.0) χ2=0.234 0.397 胃静脉曲张[例(%)] 6(31.6) 44(41.5) χ2=0.156 0.571 门静脉内径(mm) 13(11~15) 13(12~14) Z=-1.239 0.857 脾静脉内径(mm) 8(7~12) 10(8~12) Z=-1.670 0.144 脾脏厚度(mm) 45.0±10.3 54.0±14.2 t=0.126 0.051 白细胞(×109/L) 3.52(1.94~4.97) 3.99(2.24~5.23) Z=-0.467 0.633 血红蛋白(g/L) 106.2±32.2 98.0±33.4 t=0.114 0.621 血小板(×109/L) 74(48~129) 64(39~99) Z=-0.674 0.820 血钠(mmol/L) 138.0±3.6 138.0±3.7 t=0.047 0.814 血钾(mmol/L) 3.9(3.3~4.1) 3.8(3.5~4.1) Z=-1.345 0.886 总胆固醇(mmol/L) 2.9±1.2 3.1±0.9 t=0.124 0.651 甘油三酯(mmol/L) 0.8(0.6~1.1) 0.8(0.6~1.0) Z=-0.736 0.392 NT-proBNP(pg/mL) 220(160~250) 119(108~160) Z=-3.028 <0.001 cTNI(ng/mL) 0.27(0.21~0.28) 0.27(0.27~0.28) Z=-1.239 0.937 使用利尿剂[例(%)] 8(42.1) 59(55.7) χ2=0.876 0.404 表 2 肝硬化CCM组及无CCM组患者超声心动图和心电图各指标比较
Table 2. Comparison of echocardiography and electrocardiogram parameters between CCM and no-CCM
参数 CCM组(n=19) 无CCM组(n=106) 统计值 P值 QT间期(ms) 397.1±31.1 398.2±31.7 t=0.053 0.832 E/A比值 0.76(0.63~0.88) 0.98(0.77~1.30) Z=-5.789 <0.001 左心室射血分数(%) 54.2±7.8 68.3±6.6 t=1.146 0.011 左心房内径(mm) 34.6±4.5 34.5±5.1 t=0.347 0.963 左心室舒张末内径(mm) 48.3±6.7 47.9±5.4 t=0.089 0.744 左心室收缩末内径(mm) 32.2±7.5 29.1±4.5 t=0.157 0.096 左室短轴缩短率(%) 34.3±5.7 39.8±4.5 t=3.248 <0.001 左心室后壁厚度(mm) 10.1±1.7 8.9±1.5 t=1.324 0.064 室间隔厚度(mm) 11.2(9.2~11.4) 10.6(9.3~11.6) Z=-1.663 0.161 -
[1] LIU HQ, NGUYEN HH, YOON KT, et al. Pathogenic mechanisms underlying cirrhotic cardiomyopathy[J]. Front Netw Physiol, 2022, 2: 849253. DOI: 10.3389/fnetp.2022.849253. [2] WANG WW, LI HY, WANG ZC, et al. Progress in the application of ultrasonic cardiogram in cirrhotic cardiomyopathy[J]. Clin J Med Offic, 2022, 50( 9): 900- 903. DOI: 10.16680/j.1671-3826.2022.09.07.王微微, 李宏宇, 王忠超, 等. 超声心动图在肝硬化心肌病中应用进展[J]. 临床军医杂志, 2022, 50( 9): 900- 903. DOI: 10.16680/j.1671-3826.2022.09.07. [3] MØLLER S, LEE SS. Cirrhotic cardiomyopathy[J]. J Hepatol, 2018, 69( 4): 958- 960. DOI: 10.1016/j. jhep.2018.01.006. [4] MØLLER S, DANIELSEN KV, WIESE S, et al. An update on cirrhotic cardiomyopathy[J]. Expert Rev Gastroenterol Hepatol, 2019, 13( 5): 497- 505. DOI: 10.1080/17474124.2019.1587293. [5] LIANG SY, LIN Q, SONG JL, et al. Role of bile acids in cirrhosis-related cardiomyopathy[J]. J Clin Hepatol, 2022, 38( 10): 2383- 2386. DOI: 10.3969/j.issn.1001-5256.2022.10.035.梁世洋, 林强, 宋俊良, 等. 胆汁酸在肝硬化心肌病中的作用[J]. 临床肝胆病杂志, 2022, 38( 10): 2383- 2386. DOI: 10.3969/j.issn.1001-5256.2022.10.035. [6] KIM JS, KO GJ, KIM YG, et al. Plasma endocan as a predictor of cardiovascular event in patients with end-stage renal disease on hemodialysis[J]. J Clin Med, 2020, 9( 12): 4086. DOI: 10.3390/jcm9124086. [7] TOSHIKUNI N, OZAKI K, GEORGE J, et al. Serum endocan as a survival predictor for patients with liver cirrhosis[J]. Can J Gastroenterol Hepatol, 2015, 29( 8): 427- 430. DOI: 10.1155/2015/153805. [8] BALTA S, BALTA I, MIKHAILIDIS DP. Endocan: A new marker of endothelial function[J]. Curr Opin Cardiol, 2021, 36( 4): 462- 468. DOI: 10.1097/HCO.0000000000000867. [9] CELIK ZE, DEMIR F, YONAR H, et al. Association of endocan expression with clinicopathological prognostic parameters in breast carcinoma[J]. Cancer Biomark, 2021, 32( 4): 471- 477. DOI: 10.3233/CBM-201026. [10] KECHAGIA M, PAPASSOTIRIOU I, GOURGOULIANIS KI. Endocan and the respiratory system: A review[J]. Int J Chron Obstruct Pulmon Dis, 2016, 11: 3179- 3187. DOI: 10.2147/COPD.S118692. [11] SENOCAK GNC, YAPCA OE, YILMAZ EPT, et al. May endocan be a new biomarker in the diagnosis of endometriosis?[J]. J Gynecol Obstet Hum Reprod, 2022, 51( 7): 102423. DOI: 10.1016/j.jogoh.2022.102423. [12] OKYAY K. Cardiac biomarkers in coronary slow flow: Endocan and omentin-1[J]. Turk Kardiyol Dern Ars, 2019, 47( 4): 249- 250. DOI: 10.5543/tkda.2019.14701. [13] BEHNOUSH AH, KHALAJI A, BAHIRAIE P, et al. Endocan as a marker of endothelial dysfunction in hypertension: A systematic review and meta-analysis[J]. Hypertens Res, 2023, 46( 10): 2388- 2399. DOI: 10.1038/s41440-023-01402-y. [14] DELEHEDDE M, DEVENYNS L, MAURAGE CA, et al. Endocan in cancers: A lesson from a circulating dermatan sulfate proteoglycan[J]. Int J Cell Biol, 2013, 2013: 705027. DOI: 10.1155/2013/705027. [15] ZUWALA-JAGIELLO J, PAZGAN-SIMON M, SIMON K, et al. Serum endocan level in diabetes mellitus of patients with cirrhosis and risk of subsequent development of spontaneous bacterial peritonitis[J]. J Physiol Pharmacol, 2019, 70( 3): 10.26402/jpp.2019.3.06. DOI: 10.26402/jpp.2019.3.06. [16] HEN J, JIANG L, YU X, et al. Endocan: a key player of cardiovascular disease[J]. Front Cardiovasc Med, 2022, 8. DOI: 10.3389/fcvm.2021.798699. [17] BALTA S, MIKHAILIDIS DP, DEMIRKOL S, et al. Endocan: A novel inflammatory indicator in cardiovascular disease?[J]. Atherosclerosis, 2015, 243( 1): 339- 343. DOI: 10.1016/j.atherosclerosis.2015.09.030. [18] HIROOKA Y. How can endocan be used as a specific biomarker of endothelial dysfunction in hypertension?[J]. Hypertens Res, 2024, 47( 3): 794- 795. DOI: 10.1038/s41440-023-01542-1. [19] HSU SJ, LIN TY, WANG SS, et al. Endothelin receptor blockers reduce shunting and angiogenesis in cirrhotic rats[J]. Eur J Clin Invest, 2016, 46( 6): 572- 580. DOI: 10.1111/eci.12636. [20] KLISIĆ A, KAVARIĆ N, ABENAVOLI L, et al. Is endocan a novel potential biomarker of liver steatosis and fibrosis?[J]. J Med Biochem, 2020, 39( 3): 363- 371. DOI: 10.2478/jomb-2019-0042. [21] YANG JH, SHENG SH, YANG QW, et al. Endocan silencing induces programmed cell death in hepatocarcinoma[J]. Oncol Lett, 2017, 14( 5): 5333- 5339. DOI: 10.3892/ol.2017.6857. [22] HUANG X, CHEN C, WANG X, et al. Prognostic value of endocan expression in cancers: Evidence from meta-analysis[J]. Onco Targets Ther, 2016, 9: 6297- 6304. DOI: 10.2147/OTT.S110295. [23] SCHWABL P, BUCSICS T, SOUCEK K, et al. Risk factors for development of spontaneous bacterial peritonitis and subsequent mortality in cirrhotic patients with ascites[J]. Liver Int, 2015, 35( 9): 2121- 2128. DOI: 10.1111/liv.12795. [24] JR WTF. Endocan in hypertension and cardiovascular disease[J]. Angiology, 2014, 65( 9): 757- 759. DOI: 10.1177/0003319713514478. [25] VOIOSU AM, BĂLĂNESCU P, DAHA I, et al. The diagnostic and prognostic value of serum endocan in patients with cirrhotic cardiomyopathy[J]. Rom J Intern Med, 2018, 56( 3): 182- 192. DOI: 10.2478/rjim-2018-0007. -



 PDF下载 ( 699 KB)
PDF下载 ( 699 KB)

 下载:
下载:


