非酒精性脂肪性肝病伴肥胖患者血清25羟维生素D的表达及其临床意义
DOI: 10.12449/JCH240711
Expression of serum 25-hydroxyvitamin D and its clinical significance in patients with nonalcoholic fatty liver disease and obesity
-
摘要:
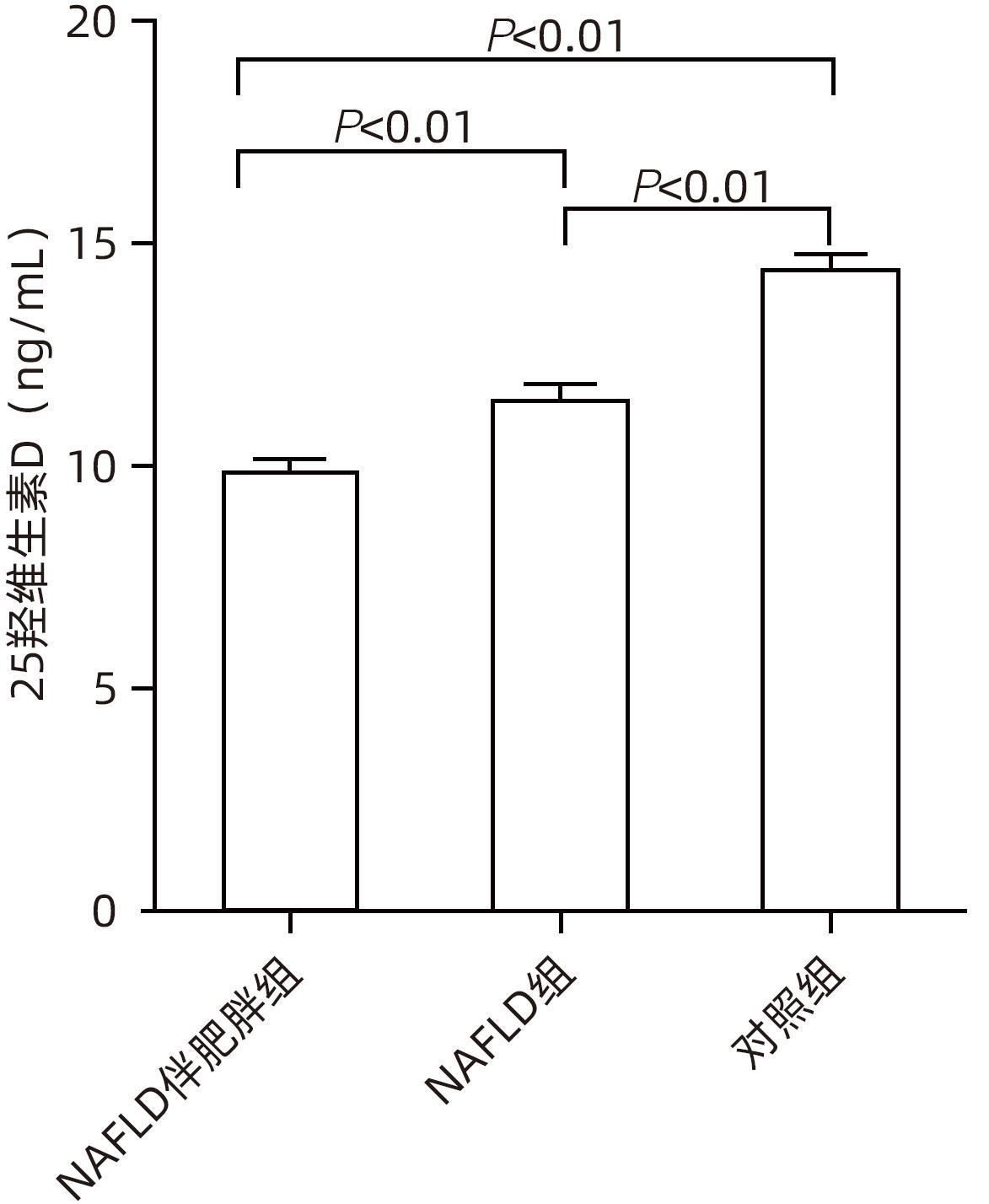
目的 检测非酒精性脂肪性肝病(NAFLD)伴肥胖患者血清25羟维生素D的表达水平,分析25羟维生素D与机体肝功能、血脂及炎症指标的关系。 方法 选取2022年1月—2023年3月于山西白求恩医院就诊的NAFLD患者90例,根据BMI分为NAFLD伴肥胖组60例(BMI≥28 kg/m2)和NAFLD组30例(BMI<28 kg/m2);另选取同期健康体检者30例作为对照组。检测3组人群血清25羟维生素D、肝功能指标(ALT、AST、ALP、GGT、TBil、DBil)、血脂指标(HDL、LDL、TC、TG)、炎症指标(H-CRP、GP-73)以及细胞因子水平(IL-2、IL-4、IL-6、IL-10、IL-17、IL-1β、TNF-α、IFN-γ),测量肝脾体积比值。正态分布的计量资料多组间比较采用单因素方差分析,进一步两两比较采用LSD-t检验或Tamhane’s T2法;非正态分布的计量资料多组间比较及进一步两两比较均采用Kruskal-Wallis H检验。相关性采用Pearson或Spearman相关性分析。 结果 与对照组相比,NAFLD伴肥胖组25羟维生素D,HDL,细胞因子IL-2、IL-4、IL-10、IFN-γ和肝脾体积比值均显著降低(P值均<0.05),而肝功能指标ALT、AST、ALP、GGT、TBil、DBil,血脂指标LDL、TC、TG,炎症指标H-CRP、GP-73及细胞因子IL-1β、IL-17、TNF-α均明显升高(P值均<0.05)。NAFLD伴肥胖组与NAFLD组比较,除肝脾体积比值和H-CRP水平外,上述指标差异均有统计学意义(P值均<0.05)。相关性分析结果显示,25羟维生素D水平与ALT(r=-0.324,P=0.012)、AST(r=-0.421,P=0.001)、ALP(r=-0.435,P=0.001)、GGT(r=-0.343,P=0.007)、TBil(r=-0.532,P<0.001)、DBil(r=-0.521,P<0.001)、LDL(r=-0.405,P=0.001)、TC(r=-0.466,P<0.001)、TG(r=-0.551,P<0.001)、H-CRP(r=-0.434,P=0.014)、GP-73(r=-0.421,P=0.001)、IL-1β(r=-0.433,P=0.001)、IL-17(r=-0.465,P<0.001)和TNF-α(r=-0.533,P<0.001)呈负相关;与HDL(r=0.632,P<0.001)、IL-2(r=0.546,P<0.001)、IL-4(r=0.533,P<0.001)、IL-10(r=0.456,P<0.001)及肝脾体积比值(r=0.543,P<0.001)呈正相关。 结论 NAFLD伴肥胖患者血清25羟维生素D与肝功能、血脂及炎症指标均存在显著相关性,25羟维生素D可能通过减轻炎症反应缓解NAFLD伴肥胖患者症状,为NAFLD治疗提供新的干预策略。 Abstract:Objective To investigate the serum level of 25-hydroxyvitamin D in patients with nonalcoholic fatty liver disease (NAFLD) and obesity, as well as the correlation of 25-hydroxyvitamin D with liver function, blood lipids, and inflammatory indicators. Methods A total of 90 patients with NAFLD who attended Shanxi Bethune Hospital from January 2022 to March 2023 were enrolled, and according to the body mass index (BMI), they were divided into NAFLD+obesity group with 60 patients (BMI≥28 kg/m2) and NAFLD group with 30 patients (BMI<28 kg/m2); 30 individuals who underwent physical examination during the same period of time were enrolled as control group. Related indications were measured for all three groups, including serum 25-hydroxyvitamin D, liver function parameters (alanine aminotransferase [ALT], aspartate aminotransferase [AST], alkaline phosphatase [ALP], gamma-glutamyl transpeptidase [GGT], total bilirubin [TBil], and direct bilirubin [DBil]), blood lipid parameters (high-density lipoprotein [HDL], low-density lipoprotein [LDL], total cholesterol [TC], and triglyceride [TG]), inflammatory indicators (high-sensitivity C-reactive protein [H-CRP] and Golgi protein 73 [GP-73]), cytokines (interleukin-2 [IL-2], interleukin-4 [IL-4], interleukin-6 [IL-6], interleukin-10 [IL-10], interleukin-17 [IL-17], interleukin-1β [IL-1β], tumor necrosis factor-α [TNF-α], and interferon gamma [IFN-γ]), and liver/spleen volume ratio. A one-way analysis of variance was used for comparison of normally distributed continuous data between multiple groups, and the least significant difference t-test or the Tamhane’s T2 test was used for further comparison between two groups; the Kruskal-Wallis H test was used for comparison of non-normally distributed continuous data between multiple groups and further comparison between two groups. A Pearson or Spearman correlation analysis was performed. Results Compared with the control group, the NAFLD+obesity group had significant reductions in 25-hydroxyvitamin D, HDL, cytokines (IL-2, IL-4, IL-10, and IFN-γ), and liver/spleen volume ratio (all P<0.05), as well as significant increases in liver function parameters (ALT, AST, ALP, GGT, TBil, and DBil), blood lipid parameters (LDL, TC, and TG), inflammatory indicators (H-CRP and GP-73), and cytokines (IL-1β, IL-17, and TNF-α) (all P<0.05). There were significant differences between the NAFLD+obesity group and the NAFLD group in all the above indicators except liver/spleen volume ratio and H-CRP (all P<0.05). The correlation analysis showed that 25-hydroxyvitamin D level was negatively correlated with ALT (r=-0.324, P=0.012), AST (r=-0.421, P=0.001), ALP (r=-0.435, P=0.001), GGT (r=-0.343, P=0.007), TBil (r=-0.532, P<0.001), DBil (r=-0.521, P<0.001), LDL (r=-0.405, P=0.001), TC (r=-0.466, P<0.001), TG (r=-0.551, P<0.001), H-CRP (r=-0.434, P=0.014), GP-73 (r=-0.421, P=0.001), IL-1β (r=-0.433, P=0.001), IL-17 (r=-0.465, P<0.001), and TNF-α (r=-0.533, P<0.001), and it was positively correlated with HDL (r=0.632, P<0.001), IL-2 (r=0.546, P<0.001), IL-4 (r=0.533, P<0.001), IL-10 (r=0.456, P<0.001), and liver/spleen volume ratio (r=0.543, P<0.001). Conclusion Serum 25-hydroxyvitamin D is significantly correlated with liver function parameters, blood lipid parameters, and inflammatory indicators in patients with NAFLD and obesity, and it may alleviate the symptoms of patients with NAFLD and obesity by reducing inflammatory response, which provides new intervention strategies for the treatment of NAFLD. -
Key words:
- Non-alcoholic Fatty Liver Disease /
- Obesity /
- 25 hydroxyvitamin D
-
表 1 3组人群肝功能、血脂指标及肝脾体积比较
Table 1. Comparison of liver function and blood lipid indicators, the ratio of liver to spleen volumes in three population groups
项目 NAFLD伴肥胖组(n=60) NAFLD组(n=30) 对照组(n=30) 统计值 P值 ALT(U/L) 27.42±4.321)2) 22.32±3.421) 19.34±2.34 F=7.652 0.009 AST(U/L) 26.35±4.341)2) 23.43±3.441) 20.32±3.45 F=6.673 0.003 ALP(U/L) 124.34±23.451)2) 112.34±23.561) 106.54±24.35 F=7.844 <0.001 GGT(U/L) 37.67±7.231)2) 32.54±6.751) 27.52±5.34 F=11.904 <0.001 TBil(μmol/L) 14.45±0.781)2) 12.43±3.221) 11.45±0.56 F=7.996 <0.001 DBil(μmol/L) 5.56±0.321)2) 4.33±0.331) 3.45±0.25 F=10.897 <0.001 HDL(mmol/L) 0.34±0.121)2) 0.85±0.21 0.83±0.14 F=14.927 <0.001 LDL(mmol/L) 6.35±0.841)2) 2.72±0.34 2.73±0.45 F=17.453 0.003 TC(mmol/L) 4.79(3.81~5.14)1)2) 3.16(1.63~4.30) 2.60(1.63~3.11) H=25.594 <0.001 TG(mmol/L) 1.62(1.28~2.80)1)2) 1.60(1.25~1.91) 1.52(1.12~2.05) H=11.633 0.003 肝脾体积比值 0.95±0.321) 1.06±0.321) 1.25±0.34 F=11.656 <0.001 注:与对照组比较,1)P<0.05;与NAFLD组比较,2)P<0.05。 表 2 3组人群炎症指标和细胞因子比较
Table 2. Comparison of inflammatory indicators and cytokine levels in three groups
项目 NAFLD伴肥胖组(n=60) NAFLD组(n=30) 对照组(n=30) 统计值 P值 H-CRP(mg/L) 3.92(1.79~10.05)1) 1.70(1.17~2.50)1) 0.52(0.32~0.72) H=25.225 <0.001 GP-73(ng/mL) 186.33±27.441)2) 178.33±26.441) 42.63±12.45 F=7.084 <0.001 IL-2(pg/mL) 3.66±0.871)2) 4.62±1.421) 5.55±1.34 F=7.746 <0.001 IL-4(pg/mL) 3.35±0.341)2) 4.56±0.561) 5.89±0.45 F=9.052 <0.001 IL-6(pg/mL) 8.57±4.221)2) 5.85±1.741) 3.39±0.68 F=12.596 <0.001 IL-10(pg/mL) 1.64±0.351)2) 2.34±0.341) 3.34±1.44 F=11.963 <0.001 IL-17(pg/mL) 3.95±0.781)2) 2.98±0.351) 1.45±0.36 F=10.925 0.003 IL-1β(pg/mL) 66.56±10.071)2) 60.87±9.051) 42.65±8.65 F=10.883 <0.001 TNF-α(pg/mL) 4.77±2.331)2) 3.92±2.011) 2.65±1.32 F=9.855 0.007 IFN-γ(pg/mL) 2.06±0.321)2) 2.95±0.541) 3.85±1.25 F=10.092 <0.001 注:与对照组比较,1)P<0.05;与NAFLD组比较,2)P<0.05。 -
[1] DUAN YM, PAN XF, LUO JY, et al. Association of inflammatory cytokines with non-alcoholic fatty liver disease[J]. Front Immunol, 2022, 13: 880298. DOI: 10.3389/fimmu.2022.880298. [2] ESTES C, ANSTEE QM, ARIAS-LOSTE MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030[J]. J Hepatol, 2018, 69( 4): 896- 904. DOI: 10.1016/j.jhep.2018.05.036. [3] BAEKE F, TAKIISHI T, KORF H, et al. Vitamin D: Modulator of the immune system[J]. Curr Opin Pharmacol, 2010, 10( 4): 482- 496. DOI: 10.1016/j.coph.2010.04.001. [4] FU LK, CUI HM, ZOU CY, et al. Correlation between serum 25(OH) vitamin D and liver fibrosis in nonalcoholic fatty liver disease[J/CD]. Chin J Oper Proced Gen Surg(Electronic Edition), 2019, 13( 6): 603- 605. DOI: 10.3877/cma.j.issn.1674-3946.2019.06.019.付丽坤, 崔红梅, 邹春燕, 等. 血清25(OH)维生素D与非酒精性脂肪性肝病肝纤维化的相关性研究[J/CD]. 中华普外科手术学杂志(电子版), 2019, 13( 6): 603- 605. DOI: 10.3877/cma.j.issn.1674-3946.2019.06.019. [5] China Working Group on Obesity. Guidelines for adult overweight and obesity prevention and control in China(excerpt)[J]. Acta Nutr Sin, 2004, 26( 1): 1- 4. DOI: 10.13325/j.cnki.acta.nutr.sin.2004.01.001.中国肥胖问题工作组. 中国成人超重和肥胖症预防与控制指南(节录)[J]. 营养学报, 2004, 26( 1): 1- 4. DOI: 10.13325/j.cnki.acta.nutr.sin.2004.01.001. [6] National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007.中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. [7] YUAN S, LARSSON SC. Inverse association between serum 25-hydroxyvitamin D and nonalcoholic fatty liver disease[J]. Clin Gastroenterol Hepatol, 2023, 21( 2): 398- 405. DOI: 10.1016/j.cgh.2022.01.021. [8] BARCHETTA I, CIMINI FA, CAVALLO MG. Vitamin D and metabolic dysfunction-associated fatty liver disease(MAFLD): An update[J]. Nutrients, 2020, 12( 11): 3302. DOI: 10.3390/nu12113302. [9] LI HL, DENG QM. The clinical significance of the alteration of serum 25(OH)D levels in obese children with nonalcoholic fatty liver disease[J]. Chin Hepatol, 2023, 28( 7): 810- 813. DOI: 10.3969/j.issn.1008-1704.2023.07.018.李洪林, 邓全敏. 肥胖儿童非酒精性脂肪性肝病血清25(OH)D水平变化及临床意义[J]. 肝脏, 2023, 28( 7): 810- 813. DOI: 10.3969/j.issn.1008-1704.2023.07.018. [10] RAO J, ZHANG R, HUANG XD, et al. Clinical effect of vitamin D combined with silybin capsule in the treatment of non-alcoholic fatty liver disease and its effect on serum plas-minogen activator inhibitor-1 and cathepsin D[J]. Clin J Med Offic, 2023, 51( 6): 582- 586. DOI: 10.16680/j.1671-3826.2023.06.09.饶静, 张汝, 黄旭东, 等. 维生素D联合水飞蓟宾胶囊治疗非酒精性脂肪性肝病临床效果及其对血清纤溶酶原激活剂抑制物、组织蛋白酶D影响[J]. 临床军医杂志, 2023, 51( 6): 582- 586. DOI: 10.16680/j.1671-3826.2023.06.09. [11] JU XL, PEI DM. Relationship between 25 hydroxyvitamin D deficiency and abnormal blood lipid, overweight or obesity[J]. J Clin Med Pract, 2020, 24( 6): 101- 104. DOI: 10.7619/jcmp.202006028.鞠香丽, 裴冬梅. 25羟维生素D缺乏与血脂异常及超重/肥胖的关系[J]. 实用临床医药杂志, 2020, 24( 6): 101- 104. DOI: 10.7619/jcmp.202006028. [12] ELIADES M, SPYROU E. Vitamin D: A new player in non-alcoholic fatty liver disease?[J]. World J Gastroenterol, 2015, 21( 6): 1718- 1727. DOI: 10.3748/wjg.v21.i6.1718. [13] SHEKA AC, ADEYI O, THOMPSON J, et al. Nonalcoholic steatohepatitis: A review[J]. JAMA, 2020, 323( 12): 1175- 1183. DOI: 10.1001/jama.2020.2298. [14] ZHANG H, LIU JC. Role of serum Golgi protein 73 in nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2023, 39( 3): 657- 662. DOI: 10.3969/j.issn.1001-5256.2023.03.028.张航, 刘近春. 血清高尔基体蛋白73在非酒精性脂肪性肝病中的作用[J]. 临床肝胆病杂志, 2023, 39( 3): 657- 662. DOI: 10.3969/j.issn.1001-5256.2023.03.028. [15] ZHANG JJ, YU HC, LI Y, et al. Association between serum 25-hydroxy vitamin D concentrations and mortality among individuals with metabolic dysfunction-associated fatty liver disease: A prospective cohort study[J]. Am J Clin Nutr, 2022, 116( 5): 1409- 1417. DOI: 10.1093/ajcn/nqac260. [16] ZHANG YY, LI JY, NI YQ, et al. Correlational study on the levels of 25-hydroxyvitamin D and non-alcoholic fatty liver disease in type 2 diabetic patients[J]. BMC Endocr Disord, 2021, 21( 1): 100. DOI: 10.1186/s12902-021-00762-1. [17] CACCIOTTOLO TM, KUMAR A, GODFREY EM, et al. Spleen size does not correlate with histological stage of liver disease in people with nonalcoholic fatty liver disease[J]. Clin Gastroenterol Hepatol, 2023, 21( 2): 535- 537. DOI: 10.1016/j.cgh.2022.01.007. [18] PATEL M, TANN M, LIANGPUNSAKUL S. CT-scan based liver and spleen volume measurement as a prognostic indicator for patients with cirrhosis[J]. Am J Med Sci, 2021, 362( 3): 252- 259. DOI: 10.1016/j.amjms.2020.10.031. -



 PDF下载 ( 662 KB)
PDF下载 ( 662 KB)

 下载:
下载:


