幽门螺杆菌与非酒精性脂肪性肝病关系的Meta分析
DOI: 10.12449/JCH240713
Association between Helicobacter pylori and nonalcoholic fatty liver disease: A Meta-analysis
-
摘要:
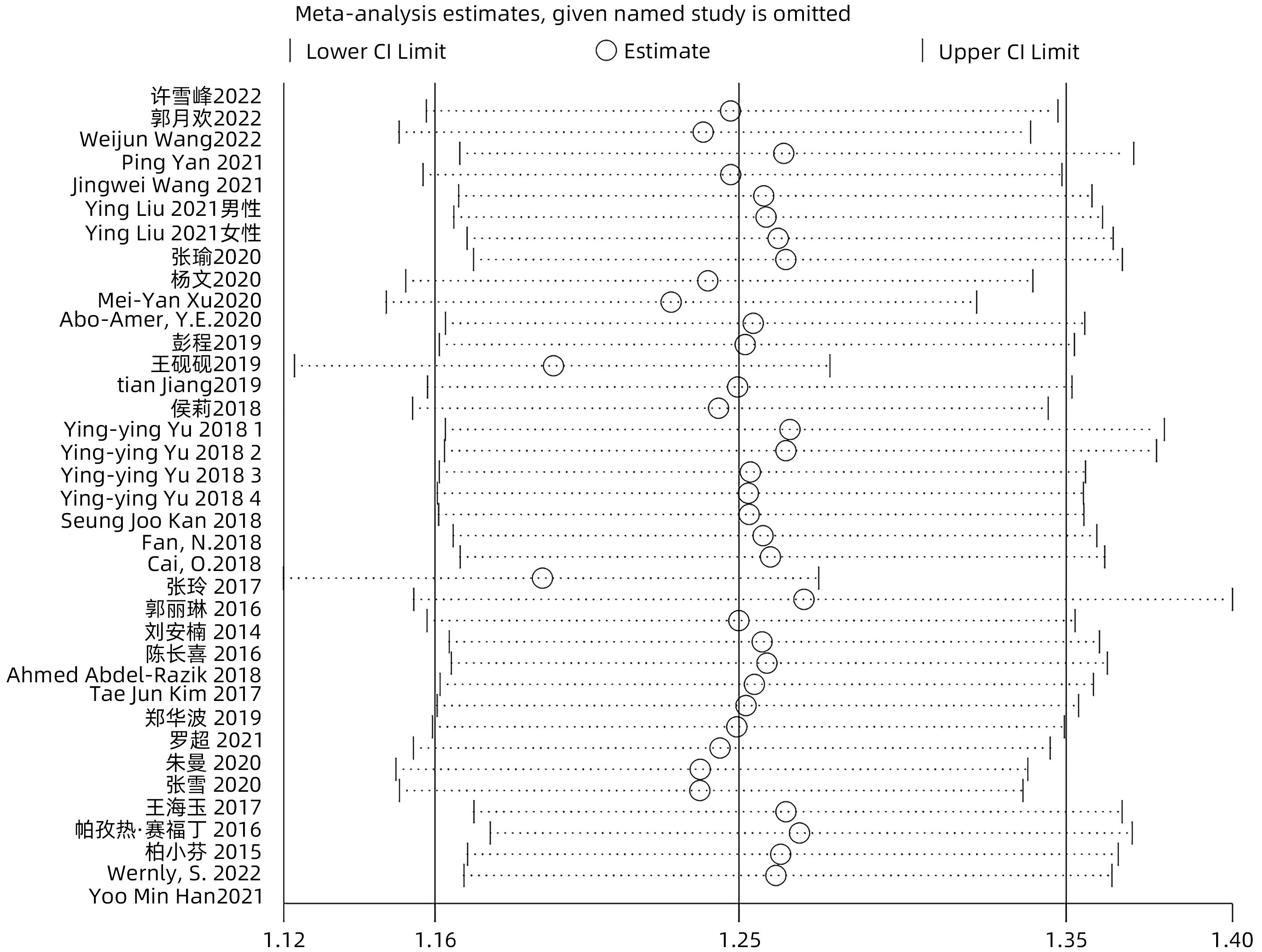
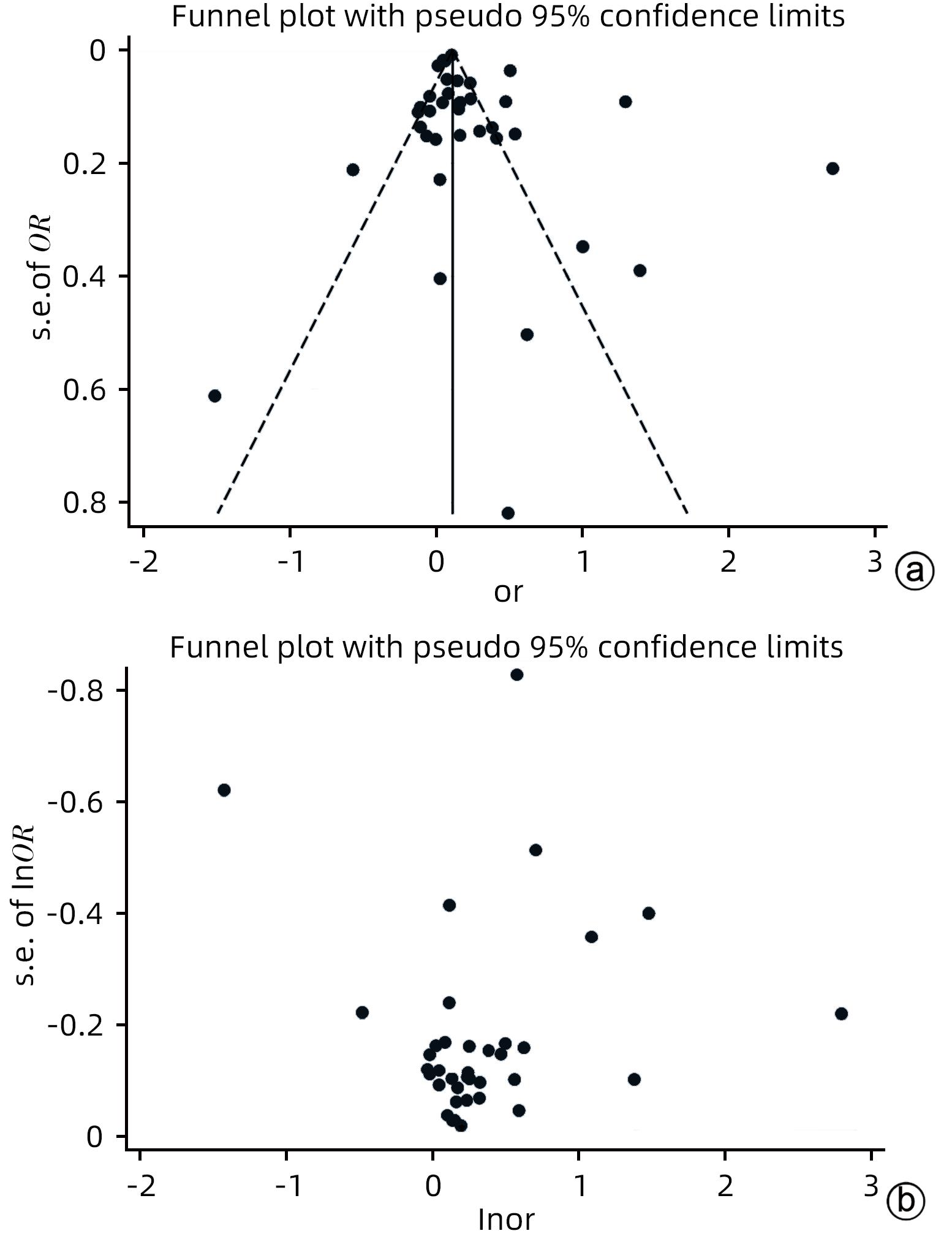
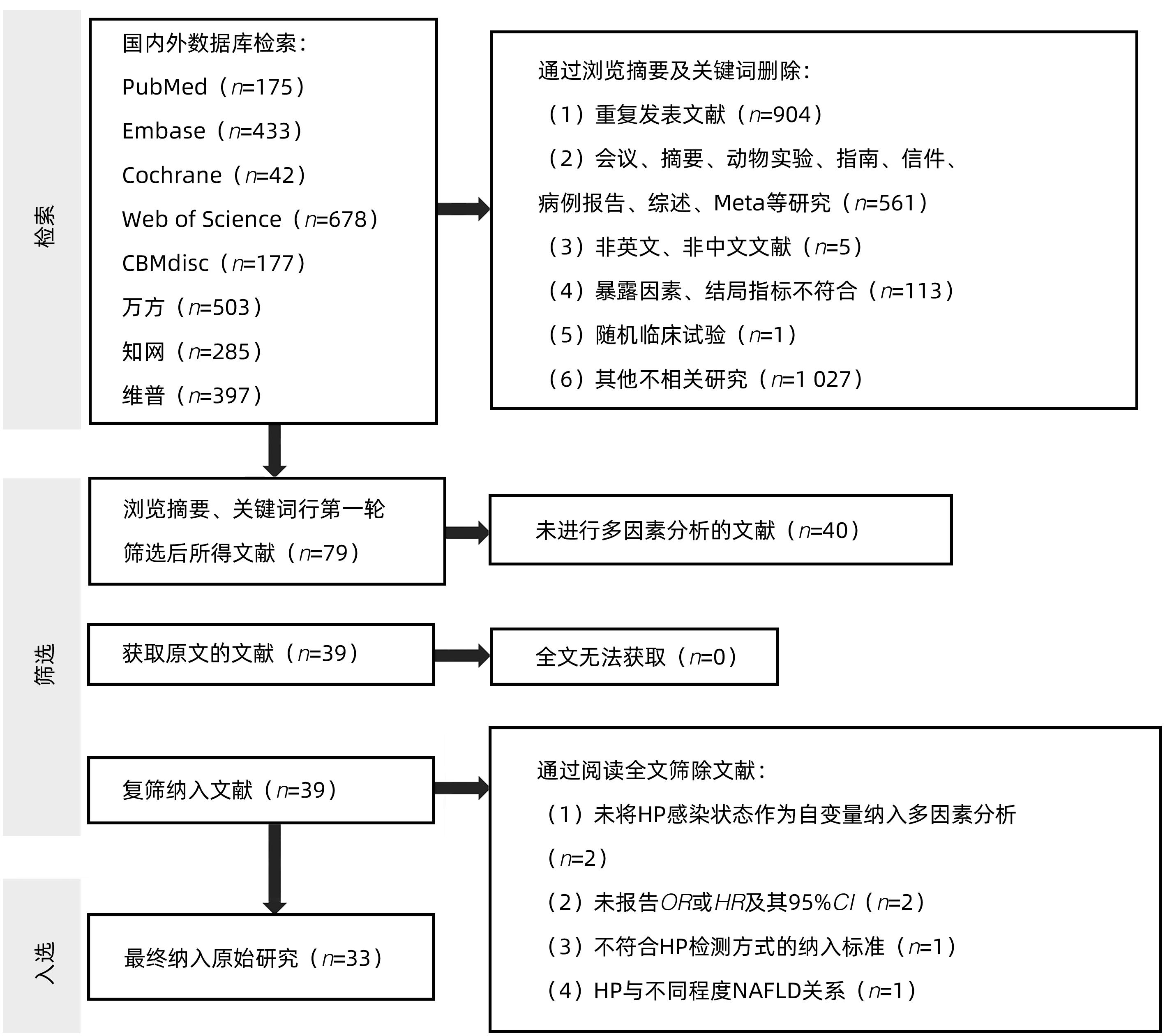
目的 探讨幽门螺杆菌(HP)感染与非酒精性脂肪性肝病(NAFLD)二者的关系。 方法 本研究根据PRISMA指南完成,PROSPERO注册号:CRD42023408932。检索PubMed、Cochrane Library、Web of Science、Embase、CBM、万方、中国知网、维普等数据库成立截至2023年6月的相关文献。选择纳入有明确HP检测标准及NAFLD评估标准,与此同时采用多因素分析评估二者相关性的病例对照研究、横断面研究及队列研究。选择优势比(OR)及其95%CI作为效应量,采用STATA 15.0软件进行Meta分析。 结果 共纳入33项原始研究,包含236 514例受试者。Meta分析结果提示,HP与NAFLD高患病率相关(OR=1.25,95%CI:1.16~1.35,P<0.05,I2=93.7%),在样本量、HP诊断方式、原始研究质量、受试者健康状况、原始研究类型方面分别行亚组分析,未找到明确的异质性来源。以样本量、HP诊断方式、原始研究质量、受试者健康状况、原始研究类型为协变量行Meta回归分析,结果提示受试者健康状况、原始研究类型可能为异质性来源。敏感性分析提示总体结果稳定,漏斗图及Egger检验未提示明显发表偏倚。 结论 在总体人群中,HP与NAFLD高患病率相关,仍需要大规模的前瞻性队列研究具体和全面地评价HP与NAFLD之间的相关性。 Abstract:Objective To investigate the association between Helicobacter pylori infection and nonalcoholic fatty liver disease (NAFLD). Methods This study was conducted acoording to the PRISMA guideline, with a PROSPERO registration number of CRD42023408932. Databases including PubMed, the Cochrane Library, Web of Science, Embase, CBM, Wanfang Data, CNKI, and VIP were searched for related articles published up to June 2023. This study was conducted for the case-control studies, cross-sectional studies, and cohort studies that included clear detection criteria for HP and evaluation criteria for NAFLD and performed the multivariate analysis to investigate the association between HP infection and NAFLD. Odds ratio (OR) and its 95% confidence interval (CI) were selected as the effect measures, and STATA 15.0 software was used to perform the Meta-analysis. Results A total of 33 primary studies were included, with 236 514 subjects in total. The Meta-analysis showed that HP was associated with the high prevalence rate of NAFLD (OR=1.25, 95%CI: 1.16 — 1.35, P<0.05, I2=93.7%). Subgroup analysis was conducted in terms of sample size, the diagnostic method for HP, the quality of primary study, the health status of subjects, and the type of primary study, but no clear source of heterogeneity was found. The Meta-regression analysis was conducted with the covariates of sample size, the diagnostic method for HP, the quality of primary study, the health status of subjects, and the type of primary study, and the results showed that the health status of subjects and the type of primary study might be the sources of heterogeneity. Sensitivity analysis showed that the overall results were stable, and funnel plots and the Egger test showed no significant publication bias. Conclusion HP is associated with the high prevalence rate of NAFLD in the general population, and large-scale prospective cohort studies are still needed to specifically and comprehensively evaluate the association between HP and NAFLD. -
Key words:
- Helicobacter Pylori /
- Non-alcoholic Fatty Liver Disease /
- Meta-analysis
-
表 1 检索策略
Table 1. Search strategy
搜索编号 检索词及检索字段 1 Helicobacterpylori [MeSH] 幽门螺杆菌[ti,ab,kw]OR 幽门螺旋菌[ti,ab,kw]OR 幽门螺旋杆菌[ti,ab,kw]OR 螺旋菌[ti,ab,kw] OR Helicobacterpylori[ti,ab,kw]OR Helicobacterpylon[ti,ab,kw] 2 Helicobactor pylori[ti,ab,kw]OR Campylobacterpylori[ti,ab,kw] OR Campylobacterpylorisubsp. Pylori[ti,ab,kw] OR Campylobacterpyloris[ti,ab,kw] OR H. Pylori[ti,ab,kw] OR Helicobacternemestrinae[ti,ab,kw] OR Helicobacterspp[ti,ab,kw] OR HP[ti,ab,kw] 3 #1 OR #2 4 non-alcoholic fatty liver disease [MeSH] 非酒精性脂肪肝[ti,ab,kw]OR 非酒精性脂肪肝病[ti,ab,kw]OR 单纯性脂肪肝[ti,ab,kw]OR 非乙醇性脂肪肝[ti,ab,kw]OR 非乙醇性脂肪性肝病[ti,ab,kw]OR 非酒精性脂肪性肝病[ti,ab,kw] 5 非酒精性肝[ti,ab,kw]OR NAFLD[ti,ab,kw]OR fatty liver [ti,ab,kw]OR fatty liver, nonalcoholic [ti,ab,kw]OR fatty livers, nonalcoholic [ti,ab,kw]OR NAFL[ti,ab,kw]OR NASH[ti,ab,kw]OR nonalcoholic fatty liver disease [ti,ab,kw]OR nonalcoholic hepatosteatosis [ti,ab,kw]OR nonalcoholic liver steatosis [ti,ab,kw]OR nonalcoholic steatotic hepatopathy[ti,ab,kw]OR nonalcoholic fatty livers [ti,ab,kw]OR nonalcoholic FLD[ti,ab,kw]OR nonalcoholic hepatic steatosis [ti,ab,kw]OR nonalcoholic hepatosteatosis [ti,ab,kw]OR nonalcoholic liver steatosis [ti,ab,kw]OR nonalcoholic steatohepatitis [ti,ab,kw]OR steatohepatitides, nonalcoholic [ti,ab,kw]OR steatohepatitis,nonalcoholic [ti,ab,kw] 6 #4 OR #5 7 #3 AND #6 注:ti,题目;ab,摘要;kw,关键词。 表 2 文章基本数据提取
Table 2. Article basic data extraction table
第一作者 年份 OR 95%CI 受试者来源 国家及 地区 样本量(例) NAFLD诊断方式 HP诊断方式 数据采集时间 研究类型 Kim[12] 2017 1.16 1.05~1.3 HP感染者 韩国 17 028 超声 HP IgG酶联免疫吸附试验 2005年1月—2013年12月 队列研究 Abdel-Razik[13] 2018 1.08 1.02~1.25 HP感染者 埃及 369 超声联合肝脂肪变性指数和脂肪肝指数计算 粪便抗原检测 2015年5月—2017年12月 队列研究 Abo-Amer[14] 2020 1.029 0.60~1.46 门诊就诊者 发展中 国家 646 超声(瞬时弹性成像) 粪便抗原检测 2019年6月— 10月 横断面研究 Wernly[15] 2022 0.96 0.82~1.13 筛查结直肠癌的无症状患者 奥地利 5 338 超声 组织学活检 2010年2月—2020年3月 横断面研究 张玲[16] 2017 15.09 10.0~22.8 住院患者 乌鲁木齐 712 超声 14C呼气试验 2014年10月—2015年10月 病例对照 郑华波[17] 2019 1.18 0.88~1.59 HP感染者 武汉 2 063 超声 13C呼气试验 2011年1月—2012年12月 队列研究 Wang[18] 2022 1.016 0.96~1.07 体检者 武汉 71 633 超声 13C呼气试验 2015年1月—2019年12月 横断面研究 郭月欢[20] 2022 1.721 1.29~2.3 体检者 安徽 960 超声 14C呼气试验 2019年5月—2021年6月 病例对照 Yan[21] 2021 1.35 1.02~1.79 体检者 大理 1 185 超声 13C呼气试验 2017年1月—2019年6月 横断面研究 杨文[22] 2020 2.733 1.38~5.4 住院患者 潍坊 160 超声 13C呼气试验 2019年1月— 7月 病例对照 Xu[23] 2020 1.664 1.55~1.79 体检者 北京 7 803 超声 HP IgG、IgM酶联免疫吸附试验 2012年—2015年 横断面研究 王砚砚[24] 2019 3.66 3.01~4.31 门诊及住院患者 大连 520 超声 14C呼气试验 2013年10月—2017年10月 病例对照 Jiang[25] 2019 1.27 1.07~1.5 体检者 唐山 4 081 超声 13C呼气试验 2015年 横断面研究 侯莉[26] 2018 1.516 1.28~2.35 体检及门诊患者 镇江 43 216 超声 13C呼气试验 2012年12月—2016年12月 横断面研究 Kang[27] 2018 1.17 0.95~1.43 全国人口 调查 美国 5 404 超声 HP IgG酶联免疫吸附试验 1988年—1994年第三次全国健康与营养调查 横断面研究 郭丽琳[28] 2016 1.115 1.1~1.14 体检者 四川 6 737 超声 14C呼气试验 2015年3月— 6月 横断面研究 刘安楠[29] 2014 1.265 1.12~1.4 体检者 北京 14 373 超声 14C呼气试验 2011年 横断面研究 朱曼[30] 2020 1.472 1.13~1.93 体检者 吉林 2 179 B超联合FibroTouch检查提示CAP值≥240 dB/m HP IgG酶联免疫吸附试验 2015年8月—2018年9月 横断面研究 张雪[31] 2020 1.614 1.35~1.93 体检者 宁夏 3 947 超声 14C呼气试验 2018年1月—12月 横断面研究 王海玉[32] 2017 4.041 1.88~8.67 体检者 陕西 856 超声 HP IgG酶联免疫吸附试验 2016年3月— 6月 横断面研究 柏小芬[33] 2015 0.568 0.38~0.86 体检及住院患者 暨南 1 031 超声 HP IgG酶联免疫吸附试验 2014年9月—2015年1月 横断面研究 Wang[34] 2021 0.221 0.07~0.74 体检者(≥ 20岁女性) 北京 1 898 超声 13C呼气试验 2018年7月—10月 横断面研究 许雪峰[35] 2022 1.867 0.7~5.0 住院患者(糖尿病) 福建 920 超声 快速尿素酶 试验 2018年1月— 9月 病例对照 彭程[36] 2019 1.031 0.47~2.28 体检者 徐州 317 超声 14C呼气试验 2016年4月—2018年8月 横断面研究 续表 表 3 亚组分析结果
Table 3. Subgroup analysis results
组别 OR(95%CI) I2值 P值 样本量(随机效应模型) <5 000例组 1.42(1.12~1.81) 94.2% 0.004 ≥5 000例组 1.14(1.07~1.21) 91.5% <0.001 受试者健康状况(随机效应模型) 健康组 1.16(1.09~1.23) 88.6% <0.001 不健康组 1.67(1.16~2.43) 96.9% 0.006 HP诊断方式1)(随机效应模型) 尿素呼气试验组 1.28(1.18~1.39) 94.0% <0.001 血清学抗体组 1.24(0.97~1.58) 92.0% 0.080 粪便抗原检测组 1.08(0.98~1.19) 0.0% 0.140 研究类型(随机效应模型) 病例对照组 2.77(1.25~6.13) 97.5% 0.012 横断面研究组 1.14(1.08~1.21) 87.9% <0.001 队列研究组 1.12(1.04~1.20) 0.0% 0.002 文章质量(随机效应模型) 高质量组 1.20(1.10~1.31) 91.7% <0.001 中质量组 1.17(1.04~1.32) 78.1% 0.010 低质量组 2.53(1.21~5.30) 94.7% 0.014 注:1)因组织学活检诊断HP、快速尿素酶试验仅1项研究,故不进行其分组。 表 4 Meta回归分析结果
Table 4. Meta regression analysis results
分组依据 P值 样本量 0.507 受试者健康状况 0.009 HP诊断方式 0.196 研究类型 0.002 文章质量 0.772 第一作者 年份 OR 95%CI 受试者来源 国家及 地区 样本量(例) NAFLD诊断方式 HP诊断方式 数据采集时间 研究类型 Yu[37]1) 2018 地区人口 浙江 20 389 超声 13C呼气试验 2015年1月—12月 横断面研究 分组1 1.053 1.02~1.09 分组2 1.067 1.01~1.09 分组3 1.165 1.02~1.49 分组4 1.183 1.09~1.56 张瑜[38] 2020 0.901 0.74~1.10 体检者 深圳 5 889 超声 13C呼气试验 2018年3月—2019年12月 病例对照 Han[39] 2021 0.96 0.78~1.19 体检者 首尔 1 784 CAP HP IgG酶联免疫吸附试验 2018年1月—12月 横断面研究 Liu[40] 2021 体检者 四川 超声 13C呼气试验 2018年2月—2019年6月 横断面研究 男性 1.048 0.87~1.26 3 089 女性 0.901 0.69~1.18 2 576 Fan[41] 2018 1 0.7~1.3 体检者 上海 21 456 超声 14C呼气试验 2013年5月—2014年6月 横断面研究 Cai[42] 2018 0.94 0.70~1.27 体检者 武汉 2 051 超声 14C呼气试验 2016年6月—12月 横断面研究 陈长喜[43] 2016 1.09 0.94~1.27 体检者 宁波 5 159 超声 14C呼气试验 2013年3月—11月 横断面研究 罗超[44] 2021 1.641 0.33~8.16 体检者 湖南 178 超声 14C呼气试验 2020年1月— 6月 横断面研究 帕孜热·赛福丁[45] 2016 0.887 0.70~1.08 体检者 新疆 2 323 超声 13C、14C呼气试验 2012年5月—2014年5月 横断面研究 注:CAP,受控衰减参数。1)分组1:白细胞<5.30×109/L;分组2:白细胞≥5.30×109/L~6.0×109/L;分组3:白细胞≥6.0×109/L~7.0×109/L;分组4:白细胞≥7.0×109/L。 -
[1] WANG CE, XU WT, GONG J, et al. Research progress in treatment of nonalcoholic fatty liver disease[J]. Clin J Med Off, 2022, 50( 9): 897- 899, 903. DOI: 10.16680/j.1671-3826.2022.09.06.王彩娥, 许文涛, 宫建, 等. 非酒精性脂肪性肝病治疗研究进展[J]. 临床军医杂志, 2022, 50( 9): 897- 899, 903. DOI: 10.16680/j.1671-3826.2022.09.06. [2] DIEHL AM, DAY C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis[J]. N Engl J Med, 2017, 377( 21): 2063- 2072. DOI: 10.1056/NEJMra1503519. [3] YOUNOSSI ZM, GOLABI P, PAIK JM, et al. The global epidemiology of nonalcoholic fatty liver disease(NAFLD) and nonalcoholic steatohepatitis(NASH): A systematic review[J]. Hepatology, 2023, 77( 4): 1335- 1347. DOI: 10.1097/HEP.0000000000000004. [4] GOLABI P, PAIK JM, ALQAHTANI S, et al. Burden of non-alcoholic fatty liver disease in Asia, the Middle East and North Africa: Data from Global Burden of Disease 2009-2019[J]. J Hepatol, 2021, 75( 4): 795- 809. DOI: 10.1016/j.jhep.2021.05.022. [5] National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: a 2018 update[J]. J Clin Hepatol, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007.中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. [6] ZHU L, SHEN XZ. Role of gut microbiota in progression of nonalcoholic fatty liver disease[J/CD]. Chin J Dig Med Imageology Electron Ed, 2014, 4( 6): 29- 32. DOI: 10.3877/cma.j.issn.2095-2015.2014.06.010.朱琳, 沈锡中. 肠道微生物在非酒精性脂肪肝发生发展中的作用机制[J/CD]. 中华消化病与影像杂志(电子版), 2014, 4( 6): 29- 32. DOI: 10.3877/cma.j.issn.2095-2015.2014.06.010. [7] XU XJ, ZHOU Y, LI X. Effects of intestinal microbiota and circadian rhythm on metabolism in nonalcoholic fatty liver disease[J]. Chem Life, 2021, 41( 11): 2434- 2444. DOI: 10.13488/j.smhx.20210261.徐小杰, 周燕, 李汛. 肠道微生物、昼夜节律对代谢的影响在非酒精性脂肪肝中的作用[J]. 生命的化学, 2021, 41( 11): 2434- 2444. DOI: 10.13488/j.smhx.20210261. [8] PARK JY, FORMAN D, WASKITO LA, et al. Epidemiology of Helicobacter pylori and CagA-positive infections and global variations in gastric cancer[J]. Toxins, 2018, 10( 4): 163. DOI: 10.3390/toxins10040163. [9] REN S, CAI PP, LIU YQ, et al. Prevalence of Helicobacter pylori infection in China: A systematic review and meta-analysis[J]. J Gastroenterol Hepatol, 2022, 37( 3): 464- 470. DOI: 10.1111/jgh.15751. [10] FU L, WANG TT, LIU LL, et al. Study on the relationship between carotid atherosclerosis and Helicobacter pylori infection in middle-aged and elderly people[J]. J Clin Exp Med, 2022, 21( 22): 2429- 2433. DOI: 10.3969/j.issn.1671-4695.2022.22.021.付丽, 王婷婷, 刘玲玲, 等. 中老年人群颈动脉粥样硬化与幽门螺杆菌感染的相关性研究[J]. 临床和实验医学杂志, 2022, 21( 22): 2429- 2433. DOI: 10.3969/j.issn.1671-4695.2022.22.021. [11] RABELO-GONÇALVES EM, ROESLER BM, ZEITUNE JM. Extragastric manifestations of Helicobacter pylori infection: Possible role of bacterium in liver and pancreas diseases[J]. World J Hepatol, 2015, 7( 30): 2968- 2979. DOI: 10.4254/wjh.v7.i30.2968. [12] KIM TJ, SINN DH, MIN YW, et al. A cohort study on Helicobacter pylori infection associated with nonalcoholic fatty liver disease[J]. J Gastroenterol, 2017, 52( 11): 1201- 1210. DOI: 10.1007/s00535-017-1337-y. [13] ABDEL-RAZIK A, MOUSA N, SHABANA W, et al. Helicobacter pylori and non-alcoholic fatty liver disease: A new enigma?[J]. Helicobacter, 2018, 23( 6): e12537. DOI: 10.1111/hel.12537. [14] ABO-AMER YEE, SABAL A, AHMED R, et al. Relationship between Helicobacter pylori infection and nonalcoholic fatty liver disease(NAFLD) in a developing country: A cross-sectional study[J]. Diabetes Metab Syndr Obes, 2020, 13: 619- 625. DOI: 10.2147/DMSO.S237866. [15] WERNLY S, WERNLY B, SEMMLER G, et al. Non-alcoholic fatty liver disease is not independently associated with Helicobacter pylori in a central European screening cohort[J]. Minerva Med, 2022, 113( 6): 936- 949. DOI: 10.23736/S0026-4806.22.07928-9. [16] ZHANG L, GAO F. Correlation between nonalcoholic fatty liver disease and Helicobacter pylori infection[J]. Chin J Dig, 2017, 37( 1): 43- 45. DOI: 10.3760/cma.j.issn.0254-1432.2017.01.012.张玲, 高峰. 非酒精性脂肪性肝病与幽门螺杆菌感染的相关性[J]. 中华消化杂志, 2017, 37( 1): 43- 45. DOI: 10.3760/cma.j.issn.0254-1432.2017.01.012. [17] ZHENG HB. Cohort study about correlation between Helicobacter pylori infection and nonalcoholic fatty liver disease[D]. Wuhan: Huazhong University of Science and Technology, 2019.郑华波. 幽门螺杆菌感染与非酒精性脂肪肝病相关性的队列研究[D]. 武汉: 华中科技大学, 2019. [18] WANG WJ, FAN MK, GONG R, et al. Helicobacter pylori infection is not an independent risk factor of non-alcoholic fatty liver disease in China[J]. BMC Gastroenterol, 2022, 22( 1): 81. DOI: 10.1186/s12876-022-02148-6. [19] HIGGINS JPT, THOMPSON SG, DEEKS JJ, et al. Measuring inconsistency in meta-analyses[J]. BMJ, 2003, 327( 7414): 557- 560. DOI: 10.1136/bmj.327.7414.557. [20] GUO YH. Correlation between Helicobacter pylori infection and nonalcoholic fatty liver disease[D]. Hefei: Anhui Medical University, 2022.郭月欢. 幽门螺杆菌感染与非酒精性脂肪性肝病的相关性研究[D]. 合肥: 安徽医科大学, 2022. [21] YAN P, YU BC, LI M, et al. Association between nonalcoholic fatty liver disease and Helicobacter pylori infection in Dali City, China[J]. Saudi Med J, 2021, 42( 7): 735- 741. DOI: 10.15537/smj.2021.42.7.20210040. [22] YANG W, WANG YJ, ZHANG ZG, et al. Correlation between helicobacter pylori infection and nonalcoholic fatty liver disease[J]. Chin J Health Care Med, 2020, 22( 2): 212- 213. DOI: 10.3969/j.issn.1674-3245.2020.02.032.杨文, 王要军, 张智高, 等. 幽门螺旋杆菌感染与非酒精性脂肪肝相关研究[J]. 中华保健医学杂志, 2020, 22( 2): 212- 213. DOI: 10.3969/j.issn.1674-3245.2020.02.032. [23] XU MY, MA JH, DU J, et al. Nonalcoholic fatty liver disease is associated with Helicobacter pylori infection in north urban Chinese: A retrospective study[J]. Gastroenterol Res Pract, 2020, 2020: 9797841. DOI: 10.1155/2020/9797841. [24] WANG YY, YU QG, LIU XX, et al. Study on association between Helicobacter pylori infection and nonalcoholic fatty liver disease[J]. Acta Agric Shanghai, 2019, 36( 5): 919- 921. DOI: 10.3969/j.issn.1671-7171.2019.05.029.王砚砚, 于庆功, 刘昕欣, 等. 幽门螺杆菌感染与非酒精性脂肪性肝病的相关性[J]. 医学临床研究, 2019, 36( 5): 919- 921. DOI: 10.3969/j.issn.1671-7171.2019.05.029. [25] JIANG T, CHEN X, XIA CM, et al. Association between Helicobacter pylori infection and non-alcoholic fatty liver disease in North Chinese: A cross-sectional study[J]. Sci Rep, 2019, 9( 1): 4874. DOI: 10.1038/s41598-019-41371-2. [26] HOU L, WU Y. Prevalence of nonalcoholic fatty liver disease and its correlation with Helicobacter pylori infection in Zhenjiang area[J]. Chin J Gerontol, 2018, 38( 4): 844- 845. DOI: 10.3969/j.issn.1005-9202.2018.04.033.侯莉, 吴莺. 镇江地区非酒精性脂肪性肝病患病情况及与幽门螺杆菌感染的相关性[J]. 中国老年学杂志, 2018, 38( 4): 844- 845. DOI: 10.3969/j.issn.1005-9202.2018.04.033. [27] KANG SJ, KIM HJ, KIM D, et al. Association between cagA negative Helicobacter pylori status and nonalcoholic fatty liver disease among adults in the United States[J]. PLoS One, 2018, 13( 8): e0202325. DOI: 10.1371/journal.pone.0202325. [28] GUO LL, LU MJ, HE M, et al. Research on the correlation between nonalcoholic fatty liver disease and Helicobacter pylori[J]. West China Med J, 2016, 31( 10): 1667- 1670. DOI: 10.7507/1002-0179.201600458.郭丽琳, 卢梦婕, 何敏, 等. 非酒精性脂肪性肝病与幽门螺杆菌的相关性研究[J]. 华西医学, 2016, 31( 10): 1667- 1670. DOI: 10.7507/1002-0179.201600458. [29] LIU AN, WANG LL, ZHANG Y, et al. Association between nonalcoholic fatty liver disease and Helicobacter pylori[J]. Chin J Gastroenterol Hepatol, 2014, 23( 12): 1451- 1454. DOI: 10.3969/j.issn.1006-5709.2014.12.023.刘安楠, 王蕾蕾, 张晏, 等. 非酒精性脂肪性肝病与幽门螺杆菌感染的相关性[J]. 胃肠病学和肝病学杂志, 2014, 23( 12): 1451- 1454. DOI: 10.3969/j.issn.1006-5709.2014.12.023. [30] ZHU M. Analysis of clinical features and identification of risk factors of nonalcoholic fatty liver disease in Changchun[D]. Changchun: Jilin University, 2020.朱曼. 长春市非酒精性脂肪性肝病患者临床特征分析及危险因素识别研究[D]. 长春: 吉林大学, 2020. [31] ZHANG X. Analysis of the correlation between Helicobacter pylori infection and non-alcoholic fatty liver disease[D]. Lanzhou: Northwest University for Nationalities, 2020.张雪. 幽门螺杆菌感染与非酒精性脂肪肝的相关性分析[D]. 兰州: 西北民族大学, 2020. [32] WANG HY. Research on the correlation between serum Helicobacter pylori antibody and nonalcoholic fatty liver disease[D]. Yan’an: Yan’an University, 2017.王海玉. 血清幽门螺旋杆菌抗体与非酒精性脂肪肝病的相关性研究[D]. 延安: 延安大学, 2017. [33] BAI XF. Relationship between Helicobacter pylori infection and nonalcoholic fatty liver disease[D]. Guangzhou: Jinan University, 2015.柏小芬. 幽门螺杆菌感染与非酒精性脂肪性肝病关系的研究[D]. 广州: 暨南大学, 2015. [34] WANG JW, DONG FX, SU H, et al. H. pylori is related to NAFLD but only in female: A Cross-sectional Study[J]. Int J Med Sci, 2021, 18( 11): 2303- 2311. DOI: 10.7150/ijms.50748. [35] XU XF, CHEN Y, ZHAO JX, et al. Relationship between Helicobacter pylori infection and nonalcoholic fatty liver disease[J]. Fujian Med J, 2022, 44( 4): 8- 11. DOI: 10.3969/j.issn.1002-2600.2022.04.004.许雪峰, 陈彦, 赵洁馨, 等. 幽门螺杆菌感染与非酒精性脂肪性肝病的关系探讨[J]. 福建医药杂志, 2022, 44( 4): 8- 11. DOI: 10.3969/j.issn.1002-2600.2022.04.004. [36] PENG C, WANG Y. The role of CagA-positive helicobacter pylori infection in the development of nonalcoholic fatty liver disease[J]. Chin J Integr Tradit West Med Dig, 2019, 27( 6): 461- 465. DOI: 10.3969/j.issn.1671-038X.2019.06.13.彭程, 王营. CagA基因幽门螺杆菌感染在非酒精性脂肪性肝病发生发展的作用[J]. 中国中西医结合消化杂志, 2019, 27( 6): 461- 465. DOI: 10.3969/j.issn.1671-038X.2019.06.13. [37] YU YY, CAI JT, SONG ZY, et al. The associations among Helicobacter pylori infection, white blood cell count and nonalcoholic fatty liver disease in a large Chinese population[J]. Medicine, 2018, 97( 46): e13271. DOI: 10.1097/MD.0000000000013271. [38] ZHANG Y, XU RJ, LI CH, et al. Analysis of the risk factors of non-alcoholic fatty liver disease and its correlation with helicobacter pylori in Shenzhen physical examination population[J]. Gansu Med J, 2020, 39( 8): 691- 694, 697. DOI: 10.15975/j.cnki.gsyy.2020.08.006.张瑜, 许瑞家, 李春华, 等. 深圳市体检人群非酒精性脂肪肝的危险因素及其与幽门螺杆菌的相关性分析[J]. 甘肃医药, 2020, 39( 8): 691- 694, 697. DOI: 10.15975/j.cnki.gsyy.2020.08.006. [39] HAN YM, LEE J, CHOI JM, et al. The association between Helicobacter pylori with nonalcoholic fatty liver disease assessed by controlled attenuation parameter and other metabolic factors[J]. PLoS One, 2021, 16( 12): e0260994. DOI: 10.1371/journal.pone.0260994. [40] LIU Y, LI DY, LIU YP, et al. Association between Helicobacter pylori infection and non-alcoholic fatty liver disease, hepatic adipose deposition and stiffness in southwest China[J]. Front Med, 2021, 8: 764472. DOI: 10.3389/fmed.2021.764472. [41] FAN NG, PENG L, XIA ZH, et al. Helicobacter pylori infection is not associated with non-alcoholic fatty liver disease: A cross-sectional study in China[J]. Front Microbiol, 2018, 9: 73. DOI: 10.3389/fmicb.2018.00073. [42] CAI O, HUANG ZP, LI M, et al. Association between Helicobacter pylori infection and nonalcoholic fatty liver disease: A single-center clinical study[J]. Gastroenterol Res Pract, 2018, 2018: 8040262. DOI: 10.1155/2018/8040262. [43] CHEN CX, GUO CY, MAO YS, et al. Relationship between nonalcoholic fatty liver disease and Helicobacter pylori infection in middle-aged and elderly people[J]. Chin J Dig, 2016, 36( 12): 839- 842. DOI: 10.3760/cma.j.issn.0254-1432.2016.12.010.陈长喜, 郭传勇, 毛玉山, 等. 中老年人群非酒精性脂肪性肝病和幽门螺杆菌感染的关系[J]. 中华消化杂志, 2016, 36( 12): 839- 842. DOI: 10.3760/cma.j.issn.0254-1432.2016.12.010. [44] LUO C. Expression and correlation analysis of fetuin A in non-alcoholic fatty liver disease[D]. Changsha: Hunan Normal University, 2021.罗超. 胎球蛋白A在非酒精性脂肪性肝病中的表达及相关性分析[D]. 长沙: 湖南师范大学, 2021. [45] PAZIRE SFD. Correlation analysis between nonalcoholic fatty liver disease and Helicobacter pylori infection[D]. Urumqi: Xinjiang Medical University, 2016.帕孜热·赛福丁. 非酒精性脂肪肝与幽门螺杆菌感染的相关性分析[D]. 乌鲁木齐: 新疆医科大学, 2016. [46] HEYDARI K, YOUSEFI M, ALIZADEH-NAVAEI R, et al. Helicobacter pylori infection and non-alcoholic fatty liver disease: A systematic review and meta-analysis[J]. Turk J Gastroenterol, 2022, 33( 3): 171- 181. DOI: 10.5152/tjg.2022.21467. [47] WEI L, DING HG. Relationship between Helicobacter pylori infection and nonalcoholic fatty liver disease: What should we expect from a meta-analysis?[J]. Medicine, 2021, 100( 31): e26706. DOI: 10.1097/MD.0000000000026706. [48] LUO YX, SHU XC, LI Q, et al. Advances in research related to Helicobacter pylori and non-alcoholic fatty liver disease[J]. Chin J Gastroenterol Hepatol, 2022, 31( 9): 980- 984. DOI: 10.3969/j.issn.1006-5709.2022.09.005.罗玉鑫, 舒小闯, 李强, 等. 幽门螺杆菌与非酒精性脂肪性肝病相关性研究进展[J]. 胃肠病学和肝病学杂志, 2022, 31( 9): 980- 984. DOI: 10.3969/j.issn.1006-5709.2022.09.005. -



 PDF下载 ( 1666 KB)
PDF下载 ( 1666 KB)

 下载:
下载: