基于临床指标和MRI征象构建的列线图对原发性肝癌中医证型的诊断效能
DOI: 10.12449/JCH240720
Performance of a nomogram model established based on clinical indices and magnetic resonance imaging signs in the diagnosis of traditional Chinese medicine syndrome types of primary liver cancer
-
摘要:
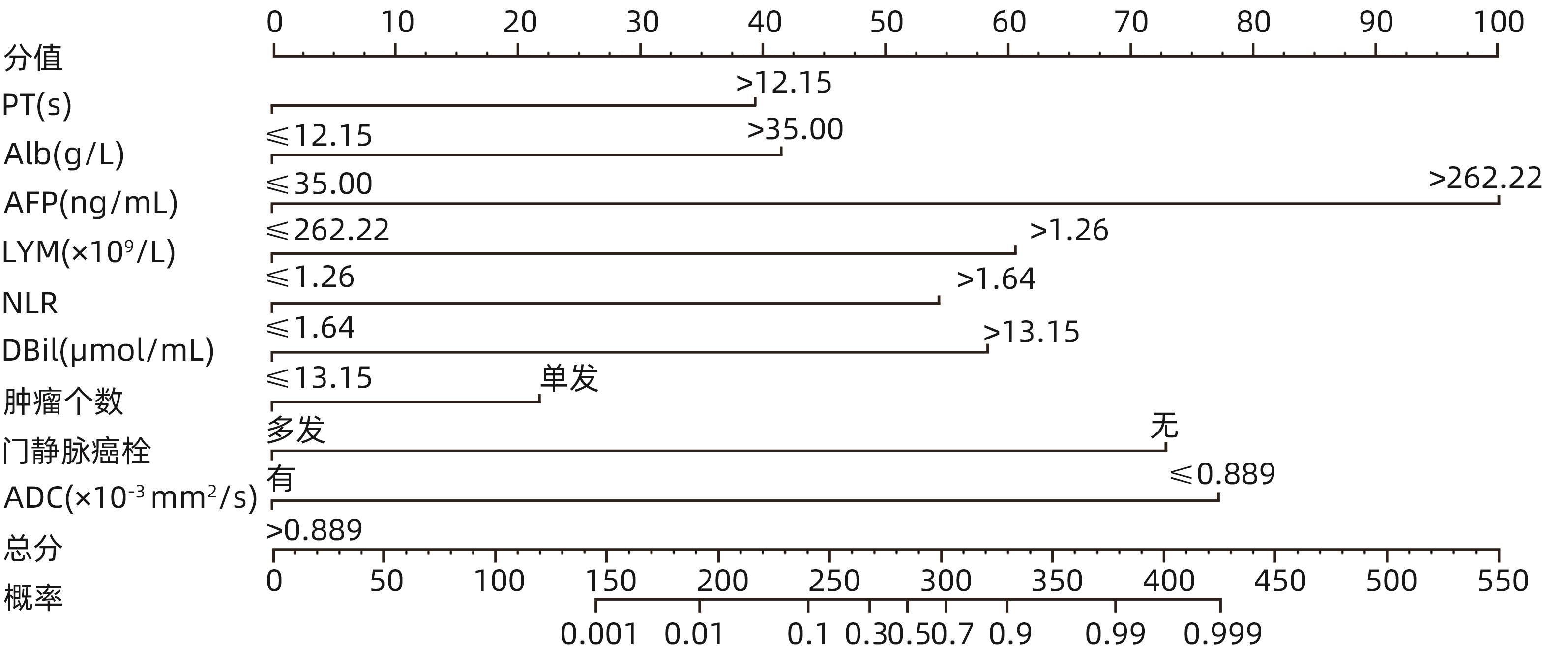
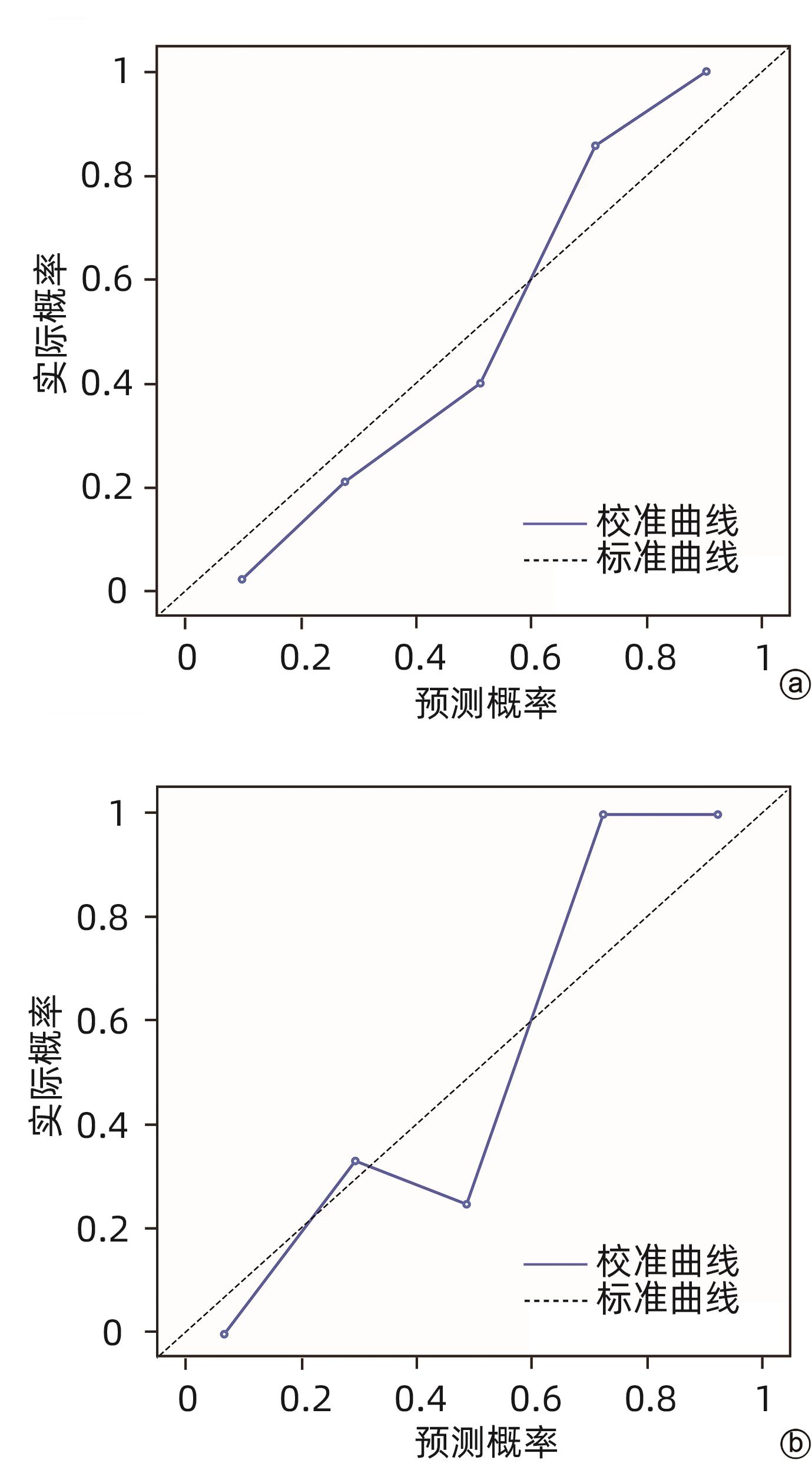
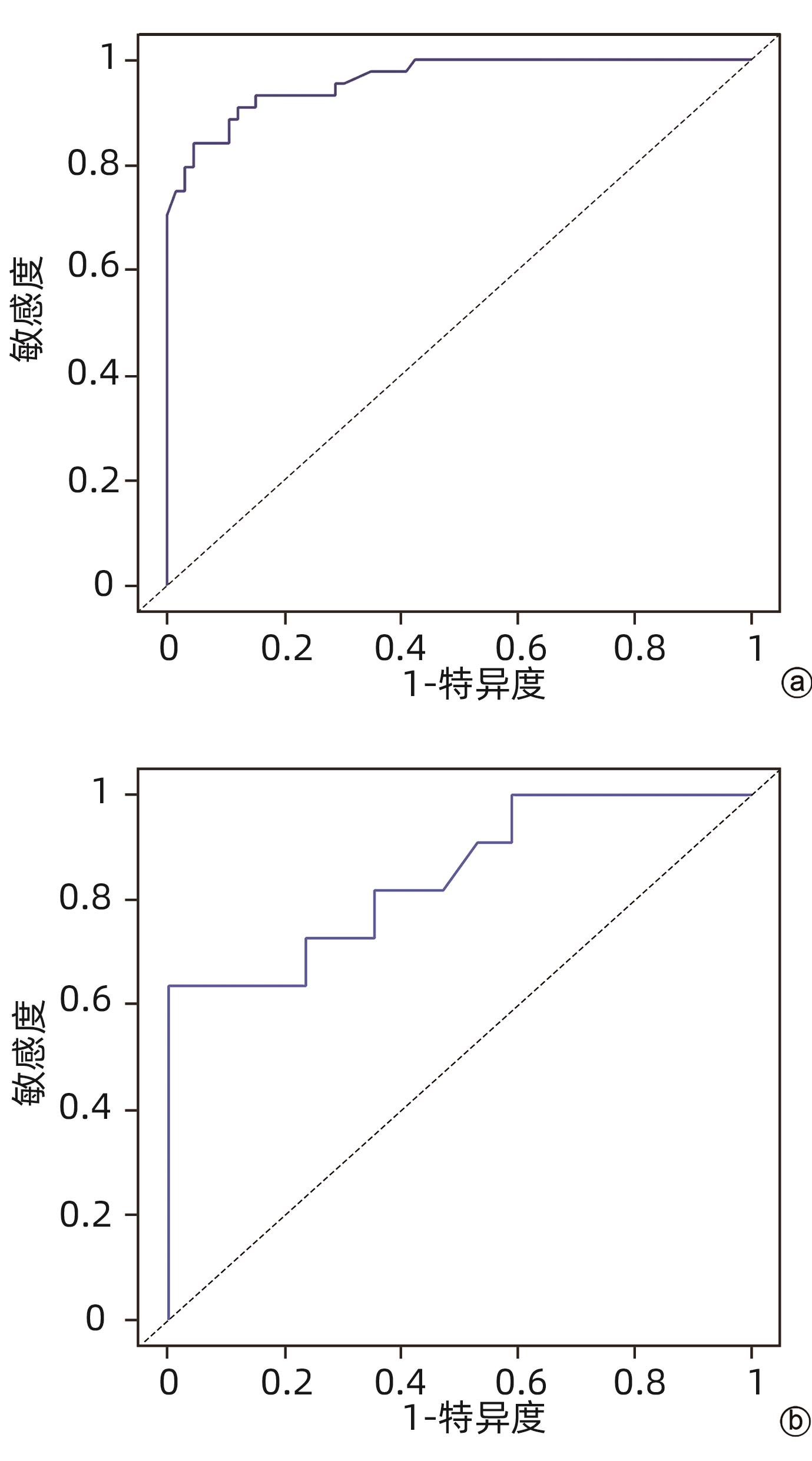
目的 探究临床指标联合MRI征象的列线图模型对原发性肝癌中医证型的判断效能。 方法 回顾性收集2018年9月—2023年7月在陕西中医药大学附属医院住院的138例原发性肝癌患者临床资料,并分为实证组(n=84)和虚证组(n=54),所有患者均在治疗前行钆塞酸二钠增强MRI扫描。计数资料组间比较采用χ2检验或Fisher确切概率检验。计量资料两组间比较采用成组t检验。应用Logistic回归分析原发性肝癌中医证型的独立预测因子,并构建列线图模型,将所有患者按8∶2随机分为训练组(n=110)和验证组(n=28)。通过校准曲线、受试者工作特征曲线(ROC曲线)和决策曲线评估模型的临床效能。 结果 实证组与虚证组比较,中性粒细胞、淋巴细胞、血小板、白蛋白、中性粒细胞/淋巴细胞比值、凝血酶原时间、甲胎蛋白、直接胆红素、间接胆红素、总胆红素、有无门静脉侵犯、肿瘤个数、肝胆期肿瘤信号和表观扩散系数差异均有统计学意义(P值均<0.05)。Logistic回归分析结果显示,甲胎蛋白(OR=0.003,95%CI:0.000~0.052,P<0.001)、凝血酶原时间(OR=0.032,95%CI:0.004~0.286,P=0.002)、淋巴细胞(OR=0.032,95%CI:0.004~0.268,P=0.002)、白蛋白(OR=0.009,95%CI:0.001~0.163,P=0.001)、中性粒细胞/淋巴细胞比值(OR=0.040,95%CI:0.003~0.457,P=0.010)、直接胆红素(OR=0.014,95%CI:0.001~0.198,P=0.002)、门静脉癌栓(OR=0.005,95%CI:0.000~0.115,P=0.001)、肿瘤个数(OR=12.740,95%CI:1.212~133.937,P=0.034)和表观扩散系数(OR=19.269,95%CI:3.163~117.387,P=0.001)是原发性肝癌中医证型分型的独立预测因子。训练组的ROC曲线下面积(AUC)、敏感度、特异度和准确度分别为0.962、84.1%、92.4%和89.1%,验证组的AUC、敏感度、特异度和准确度分别为0.848、63.6%、100.0%和85.7%。校准曲线显示列线图模型在训练组和验证组中的预测证型与实际证型之间有较好的一致性。决策曲线显示列线图在较大的阈值概率范围内有较好的净收益。 结论 基于临床指标联合MRI征象的列线图模型在判断原发性肝癌中医证型方面具有良好的临床效能和价值。 Abstract:Objective To investigate the performance of a nomogram model established based on clinical indices and magnetic resonance imaging (MRI) signs in determining the traditional Chinese medicine (TCM) syndrome types of primary liver cancer. Methods A retrospective analysis was performed for the clinical data of 138 patients with primary liver cancer who were hospitalized in The Affiliated Hospital of Shaanxi University of Chinese Medicine from September 2018 to July 2023, and the patients were divided into excess syndrome group with 84 patients and deficiency syndrome group with 54 patients. All patients underwent Gd-EOB-DTPA contrast-enhanced MRI scan before treatment. The independent-samples t test was used for comparison of continuous data between two groups, and the chi-square or the Fisher’s exact test was used for comparison of categorical data between groups. A Logistic regression analysis was used to investigate the independent predictive factors for the TCM syndrome type of primary liver cancer, and a nomogram model was established. The patients were randomly divided into training group with 110 patients and validation group with 28 patients at a ratio of 8∶2, and the calibration curve, the receiver operating characteristic (ROC) curve, and the decision curve were used to evaluate the clinical performance of this model. Results There were significant differences between the excess syndrome group and the deficiency syndrome group in neutrophils, lymphocyte count (LYM), platelet count, albumin (Alb), neutrophil-lymphocyte ratio (NLR), prothrombin time (PT), alpha-fetoprotein (AFP), direct bilirubin (DBil), indirect bilirubin, total bilirubin, presence or absence of portal vein invasion, number of tumors, hepatobiliary tumor signal, and apparent diffusion coefficient (ADC) (all P<0.05). The Logistic regression analysis showed that AFP (odds ratio [OR]=0.003, 95% confidence interval [CI]: 0.000 — 0.052, P<0.001), PT (OR=0.032, 95%CI: 0.004 — 0.286, P=0.002), LYM (OR=0.032, 95%CI: 0.004 — 0.286, P=0.002), Alb (OR=0.009, 95%CI: 0.001 — 0.163, P=0.001), NLR (OR=0.040, 95%CI: 0.003 — 0.457, P=0.010), DBil (OR=0.014, 95%CI: 0.001 — 0.198, P=0.002), portal vein cancer thrombus (OR=0.005, 95%CI: 0.000 — 0.115, P=0.001), number of tumors (OR=12.740, 95%CI: 1.212 — 133.937, P=0.034), and ADC (OR=19.269, 95%CI: 3.163 — 117.387, P=0.001) were independent predictive factors for TCM syndrome types of primary liver cancer. In the training group, the model had an area under the ROC curve (AUC) of 0.962, a sensitivity of 84.1%, a specificity of 92.4%, and an accuracy of 89.1%, and in the validation group, the model had an AUC of 0.848, a sensitivity of 63.6%, a specificity of 100.0%, and an accuracy of 85.7%. The calibration curve showed that the nomogram model had good consistency between predicted syndrome types and actual syndrome types in the training group and the validation group, and the decision curve showed that the nomogram model had good net benefits within a relatively wide range of threshold probability. Conclusion The nomogram model based on clinical indices and MRI signs has good clinical efficacy and value in judging the TCM syndrome type of primary liver cancer. -
表 1 肝癌中医证型间一般资料的单因素分析
Table 1. Single factor analysis of general data between TCM syndrome types of liver cancer
项目 实证组(n=84) 虚证组(n=54) 统计值 P值 性别[例(%)] χ2=0.003 0.957 男 65(77.4) 42(77.8) 女 19(22.6) 12(22.2) 年龄(岁) 56.40±1.09 54.50±1.56 t=1.032 0.304 乙型肝炎病史[例(%)] χ2=0.144 0.704 有 72(85.7) 45(83.3) 无 12(14.3) 9(16.7) 肝硬化[例(%)] >0.05 有 82(97.6) 53(98.1) 无 2(2.4) 1(1.9) Child-Pugh分级[例(%)] χ2=2.928 0.231 A级 52(61.9) 40(74.1) B级 24(28.6) 12(22.2) C级 8(9.5) 2(3.7) 表 2 肝癌中医证型间实验室指标的单因素分析
Table 2. Single factor analysis of laboratory indexes between TCM syndrome types of liver cancer
项目 实证组(n=84) 虚证组(n=54) χ2值 P值 NEUT[例(%)] 44.024 0.045 ≤3.87×109/L 62(73.8) 31(57.4) >3.87×109/L 22(26.2) 23(42.6) LYM[例(%)] 5.603 0.018 ≤1.26×109/L 50(59.5) 21(38.9) >1.26×109/L 34(40.5) 33(61.1) PLT[例(%)] 4.963 0.026 ≤125.50×109/L 55(65.5) 25(46.3) >125.50×109/L 29(34.5) 29(53.7) ALBI评分[例(%)] 3.809 0.051 ≤0.87 56(66.7) 27(50.0) >0.87 28(33.3) 27(50.0) Alb[例(%)] 9.459 0.002 ≤35.00 g/L 35(41.7) 9(16.7) >35.00 g/L 49(58.3) 45(83.3) NLR[例(%)] 7.925 0.005 ≤1.64 29(34.5) 7(13.0) >1.64 55(65.5) 47(87.0) PT[例(%)] 15.592 <0.001 ≤12.15 s 49(58.3) 13(24.1) >12.15 s 35(41.7) 41(75.9) AFP[例(%)] 31.446 <0.001 ≤262.22 ng/mL 79(94.0) 29(53.7) >262.22 ng/mL 5(6.0) 25(46.3) AST[例(%)] 11.289 0.256 ≤61.50 U/L 69(82.1) 40(74.1) >61.50 U/L 15(17.9) 14(25.9) ALT[例(%)] 1.826 0.177 ≤42.50 U/L 62(73.8) 34(63.0) >42.50 U/L 22(26.2) 20(37.0) LDH[例(%)] 2.762 0.097 ≤222.50 ng/mL 33(39.3) 29(53.7) >222.50 ng/mL 51(60.7) 25(46.3) CEA[例(%)] 1.876 0.171 ≤4.09 ng/mL 58(69.0) 43(79.6) >4.09 ng/mL 26(31.0) 11(20.4) DBil[例(%)] 6.194 0.013 ≤13.15 μmol/mL 65(77.4) 31(57.4) >13.15 μmol/mL 19(22.6) 23(42.6) IBil[例(%)] 5.846 0.016 ≤8.85 μmol/mL 26(31.0) 7(13.0) >8.85 μmol/mL 58(69.0) 47(87.0) TBil[例(%)] 5.263 0.022 ≤22.65 μmol/mL 51(60.7) 22(40.7) >22.65 μmol/mL 33(39.3) 32(59.3) 注:ALBI评分=0.66×log10(TBil)±(-0.085)×Alb。 表 3 肝癌中医证型间影像特征的单因素分析
Table 3. Single factor analysis of imaging features between TCM syndrome types of liver cancer
项目 实证组(n=84) 虚证组(n=54) χ2值 P值 门静脉癌栓[例(%)] 5.253 0.022 有 29(34.5) 9(16.7) 无 55(65.5) 45(83.3) 肝外转移[例(%)] 0.219 0.640 有 13(15.5) 10(18.5) 无 71(84.5) 44(81.5) 肿瘤最大直径[例(%)] 1.755 0.185 ≤4.54 cm 66(78.6) 37(68.5) >4.54 cm 18(21.4) 17(31.5) 肿瘤个数[例(%)] 6.540 0.011 单发(1个) 53(63.1) 45(83.3) 多发(≥2个) 31(36.9) 9(16.7) 肿瘤形态[例(%)] 0.545 0.761 结节型 68(81.0) 41(75.9) 块状型 14(16.7) 11(20.4) 弥漫型 2(2.4) 2(3.7) 包膜情况[例(%)] 1.071 0.301 完整 47(56.0) 35(64.8) 不完整 37(44.0) 19(35.2) 肿瘤边缘[例(%)] 0.599 0.439 光滑 43(51.2) 24(44.4) 不光滑 41(48.8) 30(55.6) 肝胆期信号[例(%)] 4.702 0.030 减低 71(84.5) 52(96.3) 不减低 13(15.5) 2(3.7) DWI信号[例(%)] 0.528 高信号 76(90.5) 51(94.4) 等信号 8(9.5) 3(5.6) ADC[例(%)] 29.826 <0.001 ≤0.889×10-3 mm2/s 21(25.0) 39(72.2) >0.889×10-3 mm2/s 63(75.0) 15(27.8) 表 4 Logistic回归分析结果
Table 4. Results of Logistic regression analysis
项目 OR 95%CI P值 AFP(ng/mL) 0.003 0.000~0.052 <0.001 PT(s) 0.032 0.004~0.286 0.002 LYM(×109/L) 0.032 0.004~0.268 0.002 Alb(g/L) 0.009 0.001~0.163 0.001 NLR 0.040 0.003~0.457 0.010 DBil(μmol/mL) 0.014 0.001~0.198 0.002 门静脉癌栓 0.005 0.000~0.115 0.001 肿瘤个数 12.740 1.212~133.937 0.034 ADC(×10-3 mm2/s) 19.269 3.163~117.387 0.001 -
[1] CHEN LC, WEI XF, GU DY, et al. Human liver cancer organoids: Biological applications, current challenges, and prospects in hepatoma therapy[J]. Cancer Lett, 2023, 555: 216048. DOI: 10.1016/j.canlet.2022.216048. [2] BROWN ZJ, TSILIMIGRAS DI, RUFF SM, et al. Management of hepatocellular carcinoma: A review[J]. JAMA Surg, 2023, 158( 4): 410- 420. DOI: 10.1001/jamasurg.2022.7989. [3] General Office of National Health Commission. Standard for diagnosis and treatment of primary liver cancer(2022 edition)[J]. J Clin Hepatol, 2022, 38( 2): 288- 303. DOI: 10.3969/j.issn.1001-5256.2022.02.009.国家卫生健康委办公厅. 原发性肝癌诊疗指南(2022年版)[J]. 临床肝胆病杂志, 2022, 38( 2): 288- 303. DOI: 10.3969/j.issn.1001-5256.2022.02.009. [4] CHEN YZ, CHEN C. Research progress in TCM syndromes objectification of primary liver cancer[J]. West J Tradit Chin Med, 2023, 36( 2): 146- 149. DOI: 10.12174/j.issn.2096-9600.2023.02.34.陈一贞, 陈闯. 原发性肝癌中医证型客观化研究进展[J]. 西部中医药, 2023, 36( 2): 146- 149. DOI: 10.12174/j.issn.2096-9600.2023.02.34. [5] LI CD, WU CY. Diagnostics of traditional Chinese medicine[M]. 3rd ed. Beijing: China Press of Traditional Chinese Medicine, 2012.李灿东, 吴承玉. 中医诊断学[M]. 3版. 北京: 中国中医药出版社, 2012. [6] China Association of Chinese Medicine. Guidelines for the diagnosis and treatment of common diseases in TCM internal medicine: Part of symptoms of Chinese medicine[M]. Beijing: China Press of Traditional Chinese Medicine, 2008.中华中医药学会. 中医内科常见病诊疗指南: 中医病症部分[M]. 北京: 中国中医药出版社, 2008. [7] WANG HX, YU ZJ, LIU JP, et al. Correlation analysis of TCM syndrome types with T lymphocytes and biochemical indices in patients with HBV-related primary liver cancer[J]. J Hainan Med Univ, 2021, 27( 22): 1692- 1697, 1703. DOI: 10.13210/j.cnki.jhmu.20210817.002.王晗笑, 于中杰, 刘建鹏, 等. HBV相关原发性肝癌患者中医证型与T淋巴细胞和生化指标的相关性分析[J]. 海南医学院学报, 2021, 27( 22): 1692- 1697, 1703. DOI: 10.13210/j.cnki.jhmu.20210817.002. [8] LIN DY, PENG B, ZHENG JH, et al. Value of a logistic regression model based on the clinical features of liver cancer in judging the traditional Chinese medicine syndrome types of primary liver cancer[J]. J Clin Hepatol, 2020, 36( 6): 1293- 1298. DOI: 10.3969/j.issn.1001-5256.2020.06.021.林栋毅, 彭波, 郑景辉, 等. 基于肝癌临床特征构建的logistic回归模型对原发性肝癌中医证型的判断效能[J]. 临床肝胆病杂志, 2020, 36( 6): 1293- 1298. DOI: 10.3969/j.issn.1001-5256.2020.06.021. [9] LIN LZ, LAN SQ, ZHOU DH. Study on relation of TCM syndrome types of primary liver cancer with relative objective indexes[J]. J Tradit Chin Med, 2001, 42( 8): 486- 488. DOI: 10.3321/j.issn:1001-1668.2001.08.023.林丽珠, 蓝韶清, 周岱翰. 原发性肝癌中医证型与相关客观化指标的关系研究[J]. 中医杂志, 2001, 42( 8): 486- 488. DOI: 10.3321/j.issn:1001-1668.2001.08.023. [10] FENG YZ, YE Z. The relationship between CT perfusion imaging and TCM syndrome of liver cancer patients[J]. J Zhejiang Chin Med Univ, 2015, 39( 6): 467- 469. DOI: 10.16466/j.issn1005-5509.2015.06.013.冯贻正, 叶子. 肝癌患者CT灌注成像与中医辨证分型的关系[J]. 浙江中医药大学学报, 2015, 39( 6): 467- 469. DOI: 10.16466/j.issn1005-5509.2015.06.013. [11] PENG J, JIA YH, LI H. Study on the relationship between CT imaging characteristics of primary liver cancer and TCM syndrome differentiation[J]. J Sichuan Tradit Chin Med, 2021, 39( 10): 57- 60.彭进, 贾燕华, 李宏. 原发性肝癌CT影像学特征与中医辨证分型的关系研究[J]. 四川中医, 2021, 39( 10): 57- 60. [12] SHANG TZ, MAO YK. Synopsis of the Golden Chamber[M]. Lanzhou: Gansu People’s Publishing House, 1980.尚坦之, 毛翼楷. 金匮要略释义[M]. 兰州: 甘肃人民出版社, 1980. [13] HUI YY, XUE JD, GAO GY, et al. Literature study on TCM syndromes and syndrome elements of primary liver cancer[J]. World Chin Med, 2023, 18( 3): 401- 405. DOI: 10.3969/j.issn.1673-7202.2023.03.018.惠友谊, 薛敬东, 高改娅, 等. 原发性肝癌中医证型及证素的文献研究[J]. 世界中医药, 2023, 18( 3): 401- 405. DOI: 10.3969/j.issn.1673-7202.2023.03.018. [14] XU CY, ZHANG GJ. Discussion on the pathogenesis of liver cancer from the pathogenesis theory of‘blood stasis and toxin interaction’[J]. China J Tradit Chin Med Pharm, 2023, 38( 4): 1469- 1472.徐楚韵, 张光霁. 试从“瘀毒互结”病机理论探析肝癌的发病机制[J]. 中华中医药杂志, 2023, 38( 4): 1469- 1472. [15] YUAN JH, ZHENG LP, WU Y. Exploration of the pathogenesis of primary liver cancer from“phlegm” pathogenic theory[J]. Tianjin J Tradit Chin Med, 2017, 34( 5): 323- 326. DOI: 10.11656/j.issn.1672-1519.2017.05.11.袁菊花, 郑丽平, 吴煜. 从“痰”之致病学说探讨原发性肝癌的发病机制[J]. 天津中医药, 2017, 34( 5): 323- 326. DOI: 10.11656/j.issn.1672-1519.2017.05.11. [16] WU YR, ZHOU T, TIAN S, et al. Study on the pathogenesis of traditional Chinese medicine of Hepatocellular carcinoma based on the“deficiency, depression and stagnation”[J]. Glob Tradit Chin Med, 2019, 12( 12): 1796- 1799. DOI: 10.3969/j.issn.1674-1749.2019.12.005.吴泳蓉, 周婷, 田莎, 等. 从“虚-郁-滞”病机浅谈肝癌的发病机理[J]. 环球中医药, 2019, 12( 12): 1796- 1799. DOI: 10.3969/j.issn.1674-1749.2019.12.005. [17] ZHANG SQ, HU H, LUO SJ, et al. Study on environmental immune mechanism of spleen deficiency in hepatocellular carcinoma[J]. Lishizhen Med Mater Med Res, 2020, 31( 8): 1961- 1963. DOI: 10.3969/j.issn.1008-0805.2020.08.059.张书侨, 胡浩, 罗绍驹, 等. 肝癌脾虚内环境免疫机制研究[J]. 时珍国医国药, 2020, 31( 8): 1961- 1963. DOI: 10.3969/j.issn.1008-0805.2020.08.059. [18] YANG XB, LONG SQ, WU WY, et al. The distribution of Chinese medicine syndrome types in primary liver cancer and their differences of the survival time: A clinical study[J]. Chin J Integr Tradit West Med, 2013, 33( 7): 911- 914. DOI: 10.7661/CJIM.2013.07.0911.杨小兵, 龙顺钦, 吴万垠, 等. 原发性肝癌中医证型分布及生存期差异研究[J]. 中国中西医结合杂志, 2013, 33( 7): 911- 914. DOI: 10.7661/CJIM.2013.07.0911. [19] LI MH, WEN GH, ZHONG JH, et al. Personalized intelligent syndrome differentiation guided by TCM consultation philosophy[J]. J Healthc Eng, 2022, 2022: 6553017. DOI: 10.1155/2022/6553017. [20] MA JL, GONG XQ, WANG ZJ, et al. SDTM: A novel topic model framework for syndrome differentiation in traditional Chinese medicine[J]. J Healthc Eng, 2022, 2022: 6938506. DOI: 10.1155/2022/6938506. [21] FANG JW, LI JF. Research on classification of primary liver cancer syndrome based on data mining technology[J]. J Healthc Eng, 2022, 2022: 2629509. DOI: 10.1155/2022/2629509. [22] OUYANG BH, XIE QQ, TANG J, et al. Changes and significances of platelet parameters in hepatocellular carcinoma patients with different syndrome classified by traditional Chinese medicine[J]. China Med Her, 2018, 15( 1): 102- 105.欧阳博慧, 谢晴晴, 唐健, 等. 不同中医证型原发性肝癌患者中血小板参数的变化及意义[J]. 中国医药导报, 2018, 15( 1): 102- 105. [23] OU J, CHEN C, HU LR, et al. Research on relationship between TCM syndrome patterns of 175 primary liver cancer patients and albumin[J]. Liaoning J Tradit Chin Med, 2015, 42( 12): 2355- 2356. DOI: 10.13192/j.issn.1000-1719.2015.12.034.欧杰, 陈闯, 胡利荣, 等. 175例原发性肝癌中医证型与血清白蛋白相关性的研究[J]. 辽宁中医杂志, 2015, 42( 12): 2355- 2356. DOI: 10.13192/j.issn.1000-1719.2015.12.034. [24] SANG XX, YANG HY, WANG ZX, et al. Distribution of CM constitutions, syndrome types, and clinical characteristics in 180 patients with HBV related liver cancer[J]. Chin J Integr Tradit West Med, 2018, 38( 12): 1425- 1429. DOI: 10.7661/j.cjim.20180926.146.桑秀秀, 杨慧银, 王仲霞, 等. 180例乙肝相关性肝癌患者的中医体质分布、证侯类型及临床特点分析[J]. 中国中西医结合杂志, 2018, 38( 12): 1425- 1429. DOI: 10.7661/j.cjim.20180926.146. [25] CHEN C, LIU L, LI JT, et al. Study on the correlation between TCM syndromes and clinical indicators of precancerous lesions of liver cancer[J]. Chin J Integr Tradit West Med Liver Dis, 2021, 31( 3): 205- 208. DOI: 10.3969/j.issn.1005-0264.2021.03.005.陈晨, 刘力, 李京涛, 等. 肝癌癌前病变中医证型与临床指标的相关性研究[J]. 中西医结合肝病杂志, 2021, 31( 3): 205- 208. DOI: 10.3969/j.issn.1005-0264.2021.03.005. [26] ZHANG Z, ZENG PH, GAO WH, et al. Discussion on the relationship between cell death and liver cancer based on the pathogenesis theory of deficiency, toxin and blood stasis[J]. J Basic Chin Med, 2021, 27( 5): 818- 820, 852. DOI: 10.19945/j.cnki.issn.1006-3250.2021.05.027.张振, 曾普华, 郜文辉, 等. 基于虚毒瘀病机理论探讨细胞焦亡与肝癌关系[J]. 中国中医基础医学杂志, 2021, 27( 5): 818- 820, 852. DOI: 10.19945/j.cnki.issn.1006-3250.2021.05.027. [27] CHANG XJ, CHANG CZ, CHANG QC, et al. On the pathogenesis and treatment of primary liver cancer from the perspective of“life instinct”[J]. Chin J Integr Tradit West Med Liver Dis, 2023, 33( 5): 444- 446. DOI: 10.3969/j.issn.1005-0264.2023.005.016.常秀娟, 常城祯, 常庆慈, 等. 从“生命本能”论原发性肝癌的病机和治疗[J]. 中西医结合肝病杂志, 2023, 33( 5): 444- 446. DOI: 10.3969/j.issn.1005-0264.2023.005.016. [28] QIAO LJ, SHAO MY. Preliminary study on the relationship between TCM syndromes of primary liver cancer and serum AFP and VEGF[J]. Acta Chin Med, 2019, 34( 3): 595- 599. DOI: 10.16368/j.issn.1674-8999.2019.03.140.乔丽娟, 邵明义. 原发性肝癌中医证型与血清AFP及VEGF相关性初步研究[J]. 中医学报, 2019, 34( 3): 595- 599. DOI: 10.16368/j.issn.1674-8999.2019.03.140. [29] QIN Y, XIE XK, KOU XN. A survey of studies on clinical indexes of common TCM syndrome patterns of primary liver cancer[J]. Jilin J Chin Med, 2022, 42( 8): 989- 992. DOI: 10.13463/j.cnki.jlzyy.2022.08.029.秦揶, 解新科, 寇小妮. 原发性肝癌常见中医证型的临床指标研究概况[J]. 吉林中医药, 2022, 42( 8): 989- 992. DOI: 10.13463/j.cnki.jlzyy.2022.08.029. [30] WANG S, ZHANG SJ, ZHANG JJ, et al. Application of magnetic resonance diffusion-weighted imaging in different TCM syndrome types of liver cancer[C]// Proceedings of the 13th National Symposium on Integrated Traditional Chinese and Western Medicine Imaging and the 8th Fujian Provincial Symposium on Integrated Traditional Chinese and Western Medicine Imaging. 2014: 34- 35.王嵩, 张世界, 张建军, 等. 肝癌不同中医证型磁共振扩散加权成像应用研究[C]// 全国第十三次中西医结合影像学术研讨会暨福建省第八次中西医结合影像学术研讨会论文集. 2014: 34- 35. [31] JIANG RY, RONG Z, MAN TT, et al. Study on the correlation between TCM patterns, histological and morphological types of primary liver cancer[J]. West J Tradit Chin Med, 2021, 34( 10): 99- 102. DOI: 10.12174/j.issn.2096-9600.2021.10.24.蒋锐沅, 荣震, 满婷婷, 等. 原发性肝癌中医证型与组织学分型及形态学分型的相关性研究[J]. 西部中医药, 2021, 34( 10): 99- 102. DOI: 10.12174/j.issn.2096-9600.2021.10.24. [32] GAO YJ, GUO XD, CHEN Y, et al. Relationship between primary liver cancer with different TCM syndromes and blood supply of color Doppler ultrasound[J]. Guid J Tradit Chin Med Pharm, 2013, 19( 12): 41- 43. DOI: 10.13862/j.cnki.cn43-1446/r.2013.12.022.皋月娟, 郭晓东, 陈艳, 等. 不同中医证型原发性肝癌与彩色多普勒超声血供关系[J]. 中医药导报, 2013, 19( 12): 41- 43. DOI: 10.13862/j.cnki.cn43-1446/r.2013.12.022. [33] ZHANG JN, LIU XA. Correlation between TCM classification of primary liver cancer and MRI imaging manifestations[J]. Chin J Pract Med, 2020, 47( 10): 7- 10. DOI: 10.3760/cma.j.cn115689-20200103-00055.张瑾宁, 刘新爱. 原发性肝癌的中医分型与MRI影像学表现的相关性研究[J]. 中国实用医刊, 2020, 47( 10): 7- 10. DOI: 10.3760/cma.j.cn115689-20200103-00055. [34] LIU XA, ZHANG YF. Study on the correlation between the TCM syndrome types of primary liver cancer and the imaging manifestations of liver specific contrast agent[J]. Acta Chin Med, 2020, 35( 5): 1093- 1097. DOI: 10.16368/j.issn.1674-8999.2020.05.244.刘新爱, 张玉峰. 原发性肝癌的中医证型与肝脏特异性对比剂影像表现相关性研究[J]. 中医学报, 2020, 35( 5): 1093- 1097. DOI: 10.16368/j.issn.1674-8999.2020.05.244. -



 PDF下载 ( 2232 KB)
PDF下载 ( 2232 KB)


 下载:
下载: