FIB-4和APRI评估慢性HBV感染者肝纤维化程度的效果比较
DOI: 10.12449/JCH241212
Effectiveness of fibrosis-4 versus aspartate aminotransferase-to-platelet ratio index in evaluating liver fibrosis degree in patients with chronic HBV infection
-
摘要:
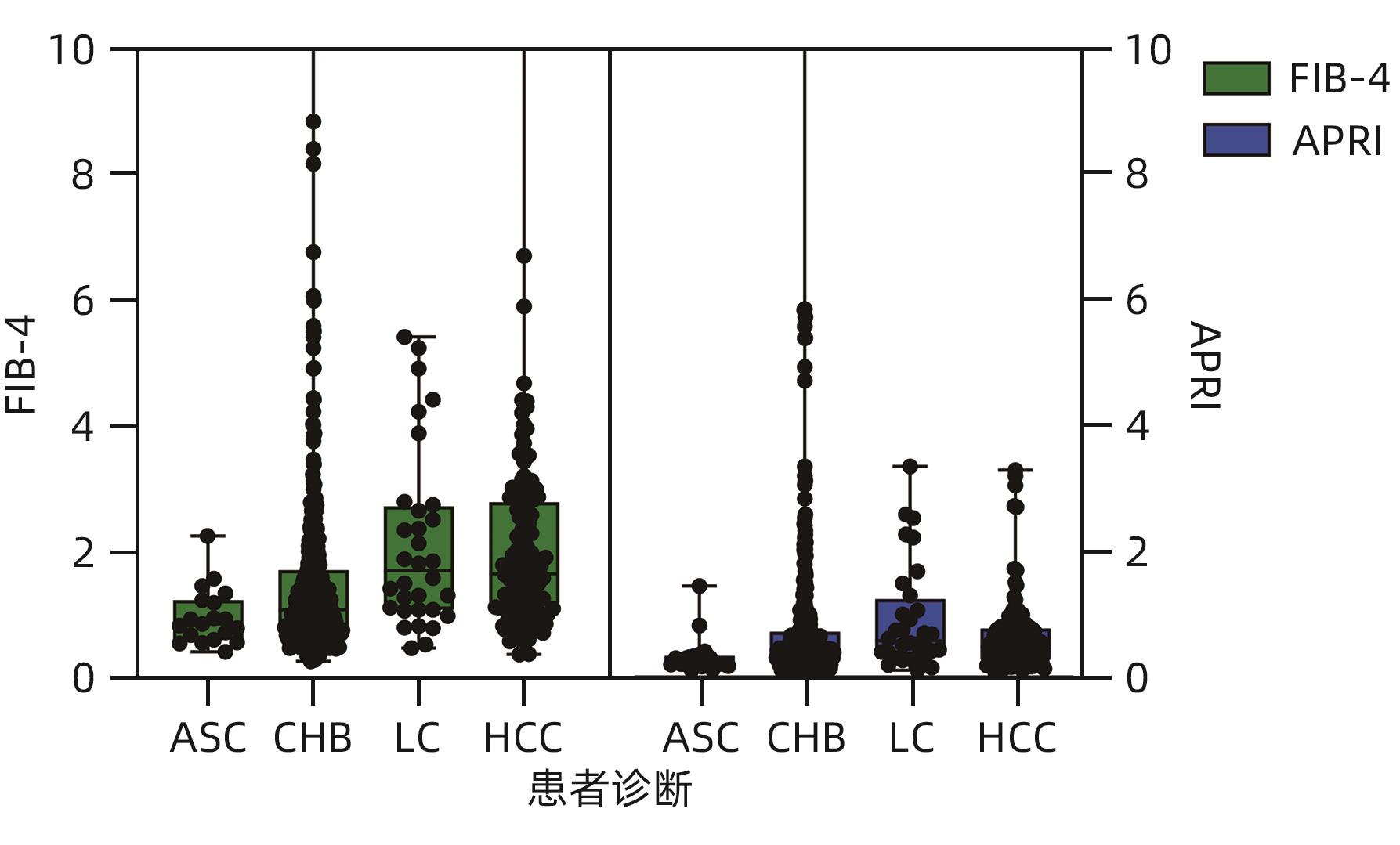
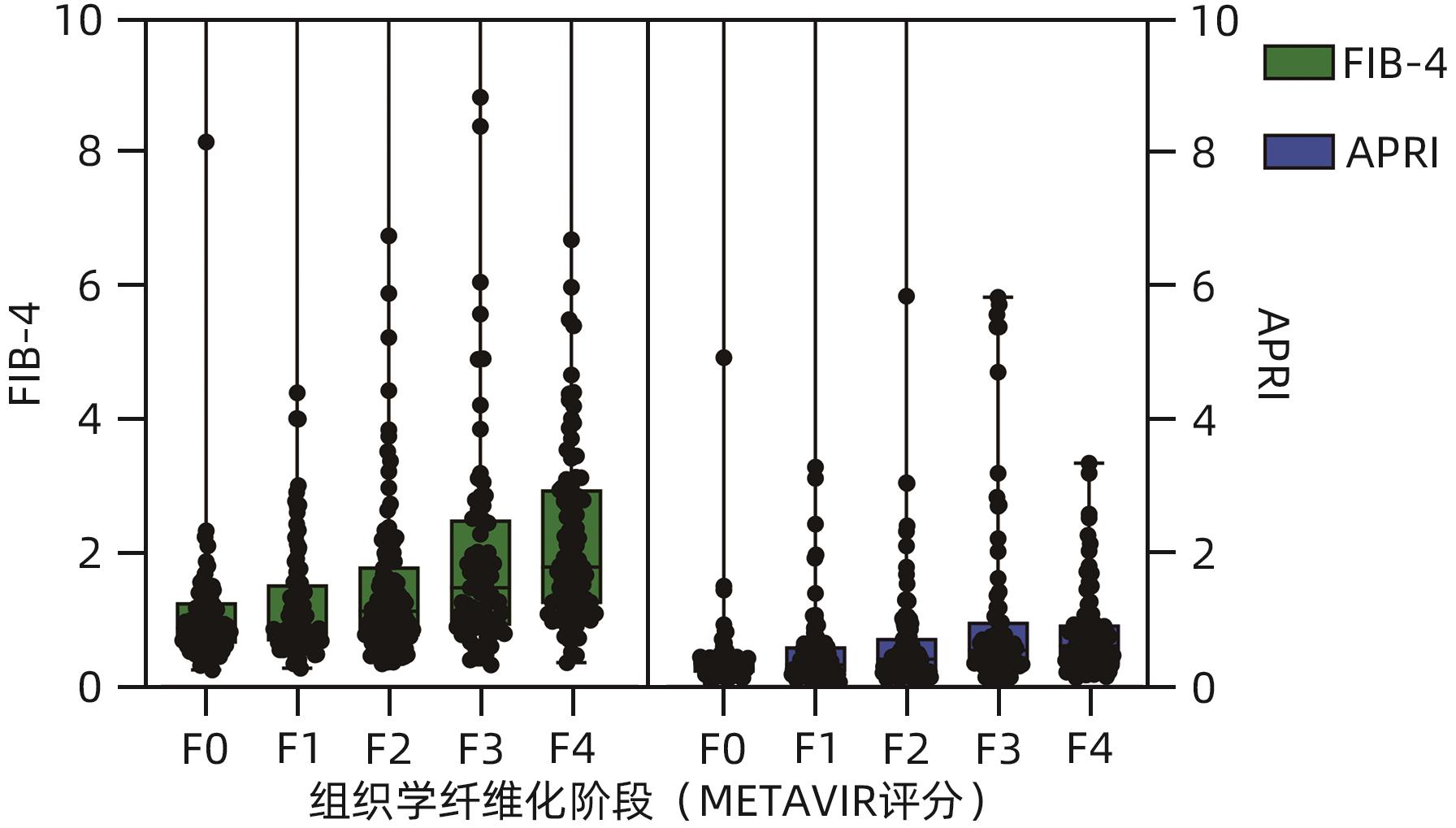
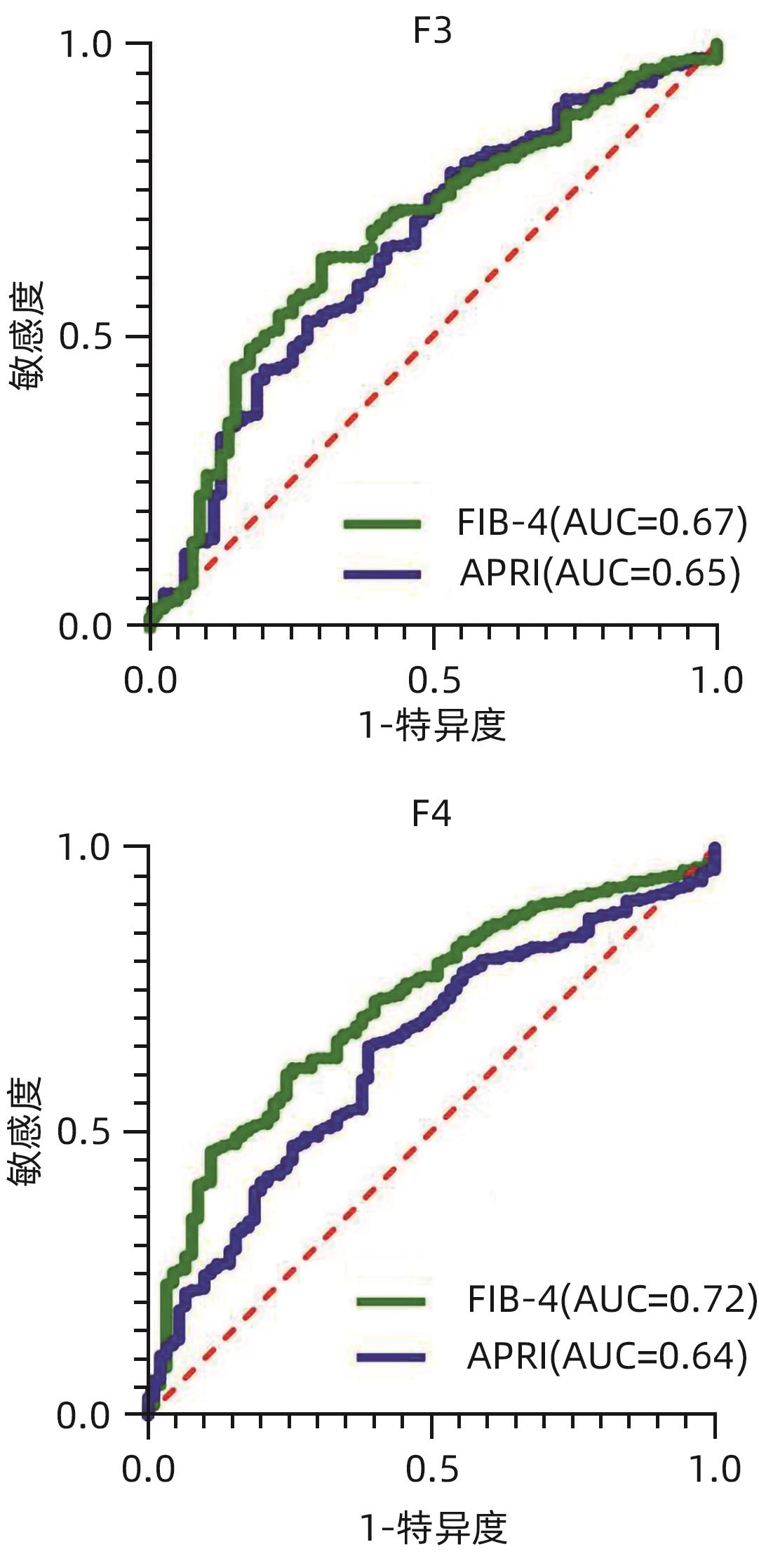
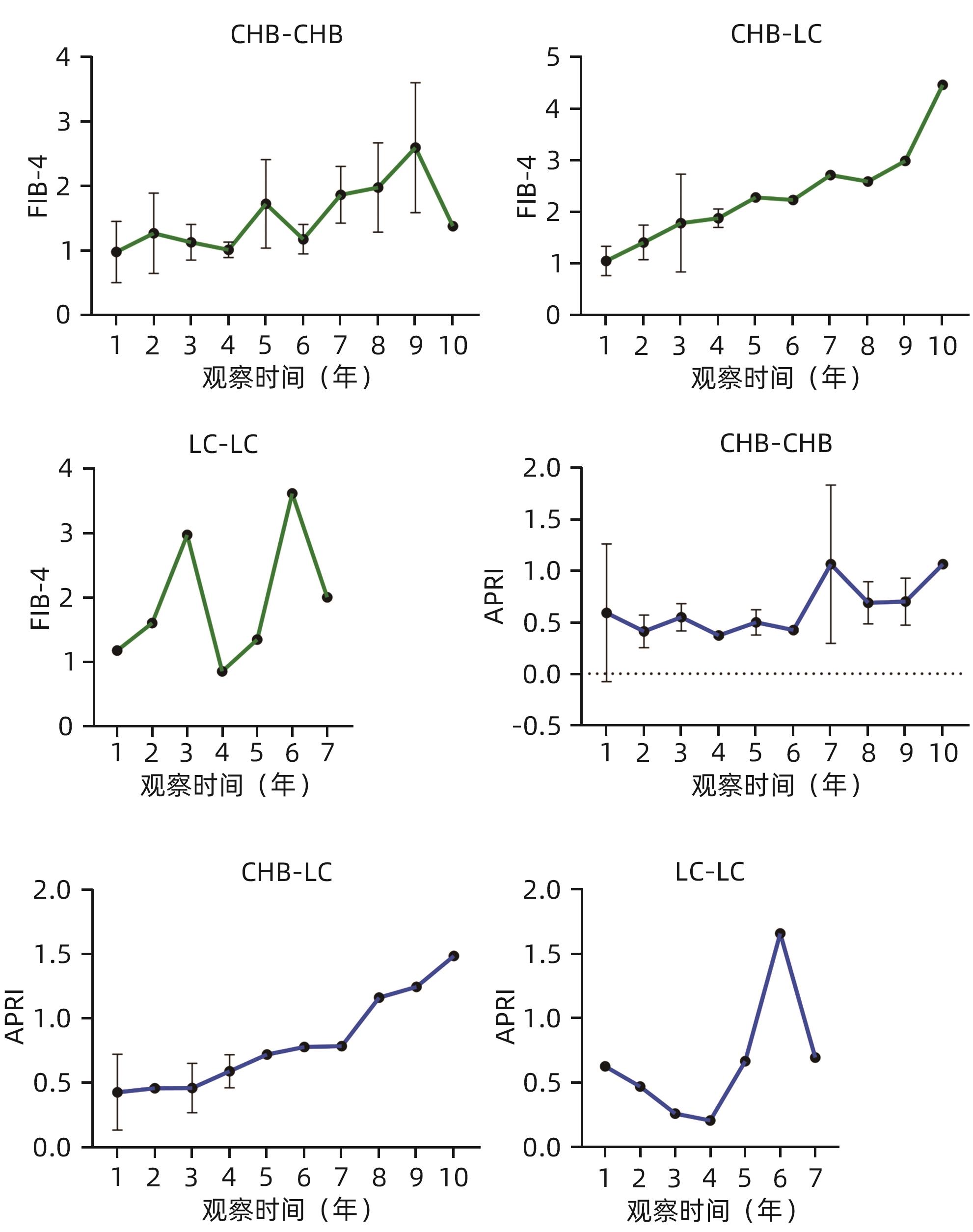
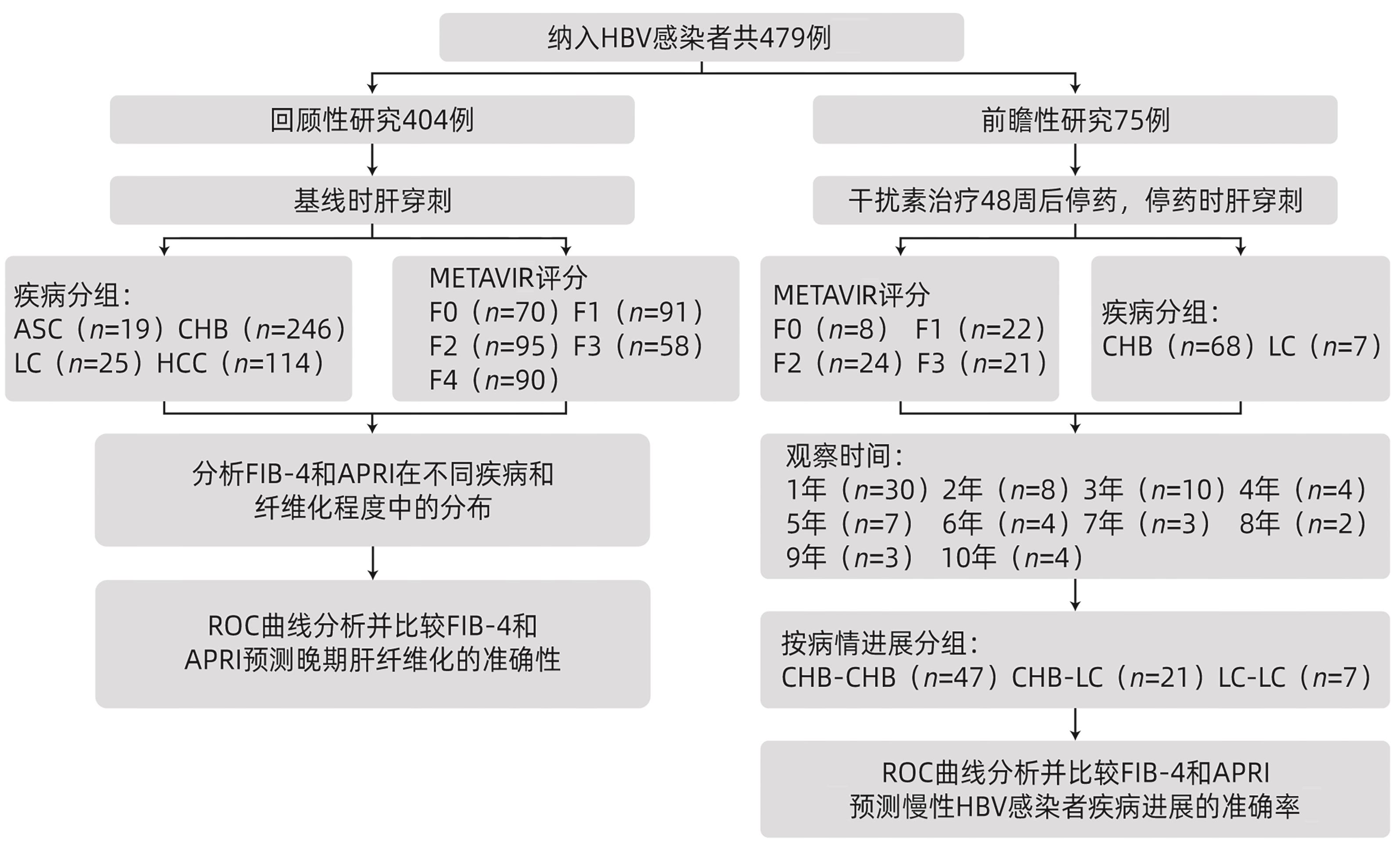
目的 比较FIB-4和APRI在慢性HBV感染者晚期肝纤维化和疾病进展中的预测效能。 方法 纳入2013年2月—2022年12月在广西医科大学第一附属医院感染科进行肝穿刺的慢性HBV感染者497例,其中回顾性研究404例,前瞻性研究75例。收集患者基线人口统计学特征(性别、年龄)、生化指标(ALT、AST)、血小板计数等指标,并计算FIB-4和APRI。非正态分布的计量资料两组间比较采用Mann-Whitney U检验,多组间数据比较采用Kruskal-Wallis H检验;计数资料组间比较采用χ2检验。采用ROC曲线下面积(AUC)分析评估APRI和FIB-4预测慢性HBV感染者肝纤维化程度和疾病进展的能力。 结果 在回顾性分析中,与FIB-4<2.67相比,FIB-4在高范围值(≥2.67)诊断为肝硬化和肝细胞癌的患者占比较高(66.19% vs 47.54%,χ2=12.75,P<0.001)。FIB-4和APRI在F0~F4期的中位值随着肝纤维化程度增加而增加,差异有统计学意义(H值分别为42.5、35.9,P值均<0.001)。在F0~F4各纤维化分期中,相同分期的FIB-4中位值均高于APRI(H=59.71,P<0.001)。FIB-4预测F3期的AUC值与APRI差异无统计学意义(0.67 vs 0.65,Z=0.71,P=0.480),预测F4期的AUC值高于APRI,差异有统计学意义(0.72 vs 0.64,Z=10.50,P<0.001)。在前瞻性研究队列中,FIB-4和APRI在出现疾病进展(慢性乙型肝炎-肝硬化)的患者中表现出随时间增加的趋势。FIB-4和APRI预测疾病进展(慢性乙型肝炎-肝硬化)的AUC分别为0.718(95%CI:0.476~0.760)和0.555(95%CI:0.408~0.703);FIB-4预测疾病进展的准确率高于APRI(χ2=12.44,P<0.001)。 结论 FIB-4和APRI均可作为评估晚期肝纤维化(F3和F4)以及预测疾病进展与否的依据,但FIB-4优于APRI。 Abstract:Objective To investigate the performance of fibrosis-4 (FIB-4) versus aspartate aminotransferase-to-platelet ratio index (APRI) in predicting advanced liver fibrosis and disease progression in patients with chronic HBV infection. Methods A total of 497 patients with chronic HBV infection who underwent liver biopsy in The First Affiliated Hospital of Guangxi Medical University from February 2013 to December 2022 were enrolled, among whom 404 were enrolled in a retrospective study and 75 were enrolled in a prospective study. Related indicators were collected, including demographic features (sex and age), biochemical indices (alanine aminotransferase [ALT] and aspartate aminotransferase [AST]), and platelet count, and FIB-4 and APRI were calculated. The Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups, and the Kruskal-Wallis H test was used for comparison between multiple groups; the chi-square test was used for comparison of categorical data between groups. The area under the ROC curve (AUC) was used to assess the ability of APRI and FIB-4 in evaluating liver fibrosis degree and disease progression in patients with chronic HBV infection. Results In the retrospective analysis, compared with the FIB-4<2.67 group, the FIB-4≥2.67 group had a significantly higher proportion of the patients who were diagnosed with liver cirrhosis or hepatocellular carcinoma (66.19% vs 47.54%, χ²=12.75, P<0.001). The medians of FIB-4 and APRI increased significantly with liver fibrosis degree from F0 to F4 (H=42.5 and 35.9, both P<0.001). As for the fibrosis stage of F0-F4, the median of FIB-4 was significantly higher than that of APRI in the patients with the same fibrosis stage (H=59.71, P<0.001). FIB-4 and APRI had a similar AUC for predicting stage F3 fibrosis (0.67 vs 0.65, Z=0.71, P=0.480), while FIB-4 had a higher AUC for predicting stage F4 fibrosis than APRI (0.72 vs 0.64, Z=10.50, P<0.001). In the prospective study cohort, FIB-4 and APRI showed an increasing trend over time in predicting disease progression (chronic hepatitis B to liver cirrhosis), with an AUC of 0.718 (95% confidence interval [CI]: 0.476 — 0.760) and 0.555 (95%CI: 0.408 — 0.703), respectively, and FIB-4 had a significantly higher accuracy than APRI in predicting disease progression (χ2=12.44, P<0.001). Conclusion FIB-4 and APRI can be used to evaluate advanced liver fibrosis (F3 and F4) and predict disease progression, and FIB-4 is superior to APRI in certain aspects. -
Key words:
- Hepatitis B Virus /
- Hepatic Fibrosis /
- Diagnosis
-
表 1 基线时AST、ALT、血小板及白蛋白水平
Table 1. Levels of AST, ALT, platelets, and albumin at baseline
指标 数值 ALT(U/L) 34(22~54) AST(U/L) 31(22~45) 血小板计数(×109/L) F0期 204.6(175.6~246.0) F1期 203.5(173.6~241.0) F2期 198.2(150.0~235.0) F3期 192.9(153.5~243.0) F4期 168.0(121.5~202.0) 白蛋白(g/L) F0期 43.2(38.9~45.9) F1期 42.3(38.9~45.0) F2期 41.3(38.6~44.0) F3期 41.5(36.9~43.4) F4期 39.8(37.0~42.8) 表 2 不同疾病分组的FIB-4和APRI比较
Table 2. FIB-4 and APRI indexes of different disease groups were compared
组别 FIB-4 APRI ASC和CHB 1.0(0.7~1.6) 0.4(0.2~0.6) LC和HCC 1.7(1.1~2.8) 1.2(0.8~1.9) Z值 6.79 3.49 P值 <0.001 <0.001 表 3 FIB-4和APRI诊断准确性对比
Table 3. Comparison of diagnostic accuracy between FIB-4 and APRI scores
项目 APRI FIB-4 F3 F4 F3 F4 AUC 0.65 0.64 0.67 0.72 临界值 0.249 0.264 0.329 0.357 敏感度 0.632 0.653 0.781 0.602 特异度 0.468 0.611 0.696 0.756 表 4 前瞻性研究队列基线时AST、ALT、血小板及白蛋白水平
Table 4. Levels of AST, ALT, platelets and albumin at baseline in a prospective study cohort
指标 数值 ALT(U/L) 44(26~85) AST(U/L) 36(26~60) 血小板计数(×109/L) F0期 204.5(161.0~254.8) F1期 186.5(160.6~221.2) F2期 187.0(146.3~238.3) F3期 148.9(128.5~178.0) 白蛋白(g/L) F0期 41.9(39.7~48.1) F1期 42.6(39.4~45.2) F2期 43.7(40.1~46.9) F3期 41.3(34.3~44.8) -
[1] ROEHLEN N, CROUCHET E, BAUMERT TF. Liver fibrosis: Mechanistic concepts and therapeutic perspectives[J]. Cells, 2020, 9( 4): 875. DOI: 10.3390/cells9040875. [2] SETO WK, LO YR, PAWLOTSKY JM, et al. Chronic hepatitis B virus infection[J]. Lancet, 2018, 392( 10161): 2313- 2324. DOI: 10.1016/S0140-6736(18)31865-8. [3] KUMARI B, KUMAR R, SHARMA S, et al. Diagnostic accuracy of FIB-4 and FIB-5 scores as compared to fibroscan for assessment of liver fibrosis in patients with non-alcoholic fatty liver disease[J]. Cureus, 2021, 13( 8): e17622. DOI: 10.7759/cureus.17622. [4] DAY JW, ROSENBERG WM. The enhanced liver fibrosis(ELF) test in diagnosis and management of liver fibrosis[J]. Br J Hosp Med(Lond), 2018, 79( 12): 694- 699. DOI: 10.12968/hmed.2018.79.12.694. [5] SINGH S, MUIR AJ, DIETERICH DT, et al. American Gastroenterological Association Institute technical review on the role of elastography in chronic liver diseases[J]. Gastroenterology, 2017, 152( 6): 1544- 1577. DOI: 10.1053/j.gastro.2017.03.016. [6] ITAKURA J, KUROSAKI M, SETOYAMA H, et al. Applicability of APRI and FIB-4 as a transition indicator of liver fibrosis in patients with chronic viral hepatitis[J]. J Gastroenterol, 2021, 56( 5): 470- 478. DOI: 10.1007/s00535-021-01782-3. [7] SHAH AG, LYDECKER A, MURRAY K, et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease[J]. Clin Gastroenterol Hepatol, 2009, 7( 10): 1104- 1112. DOI: 10.1016/j.cgh.2009.05.033. [8] RASMUSSEN DN, THIELE M, JOHANSEN S, et al. Prognostic performance of 7 biomarkers compared to liver biopsy in early alcohol-related liver disease[J]. J Hepatol, 2021, 75( 5): 1017- 1025. DOI: 10.1016/j.jhep.2021.05.037. [9] LU M, LI J, ZHANG T, et al. Serum biomarkers indicate long-term reduction in liver fibrosis in patients with sustained virological response to treatment for HCV infection[J]. Clin Gastroenterol Hepatol, 2016, 14( 7): 1044- 1055. DOI: 10.1016/j.cgh.2016.01.009. [10] SCHMID P, BREGENZER A, HUBER M, et al. Progression of liver fibrosis in HIV/HCV co-infection: a comparison between non-invasive assessment methods and liver biopsy[J]. PLoS One, 2015, 10( 9): e0138838. DOI: 10.1371/journal.pone.0138838. [11] GORDON SC, LAMERATO LE, RUPP LB, et al. Antiviral therapy for chronic hepatitis B virus infection and development of hepatocellular carcinoma in a US population[J]. Clin Gastroenterol Hepatol, 2014, 12( 5): 885- 893. DOI: 10.1016/j.cgh.2013.09.062. [12] LI J, GORDON SC, RUPP LB, et al. Long-term progression of viral load and serum markers of fibrosis among treated and untreated patients with chronic hepatitis B[J]. J Gastroenterol Hepatol, 2017, 32( 6): 1250- 1257. DOI: 10.1111/jgh.13667. [13] LI Q, REN X, LU C, et al. Evaluation of APRI and FIB-4 for noninvasive assessment of significant fibrosis and cirrhosis in HBeAg-negative CHB patients with ALT ≤2 ULN: A retrospective cohort study[J]. Medicine(Baltimore), 2017, 96( 12): e6336. DOI: 10.1097/MD.0000000000006336. [14] XIAO G, YANG J, YAN L. Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection: a systemic review and meta-analysis[J]. Hepatology, 2015, 61( 1): 292- 302. DOI: 10.1002/hep.27382. [15] GRAF C, MONDORF A, KNOP V, et al. Evaluation of point shear wave elastography using acoustic radiation force impulse imaging for longitudinal fibrosis assessment in patients with HBeAg-negative hbv infection[J]. J Clin Med, 2019, 8( 12): 2101. DOI: 10.3390/jcm8122101. [16] SANAI FM, FARAH T, ALBELADI K, et al. Diminished accuracy of biomarkers of fibrosis in low replicative chronic hepatitis B[J]. BMC Gastroenterol, 2017, 17( 1): 101. DOI: 10.1186/s12876-017-0658-x. [17] AMERNIA B, MOOSAVY SH, BANOOKH F, et al. FIB-4, APRI, and AST/ALT ratio compared to FibroScan for the assessment of hepatic fibrosis in patients with non-alcoholic fatty liver disease in Bandar Abbas, Iran[J]. BMC Gastroenterol, 2021, 21( 1): 453. DOI: 10.1186/s12876-021-02038-3. [18] SHIHA G, SEIF S, ELDESOKY A, et al. A simple bedside blood test(Fibrofast; FIB-5) is superior to FIB-4 index for the differentiation between non-significant and significant fibrosis in patients with chronic hepatitis C[J]. Hepatol Int, 2017, 11( 3): 286- 291. DOI: 10.1007/s12072-017-9796-z. [19] GRAUPERA I, THIELE M, SERRA-BURRIEL M, et al. Low accuracy of FIB-4 and NAFLD fibrosis scores for screening for liver fibrosis in the population[J]. Clin Gastroenterol Hepatol, 2022, 20( 11): 2567- 2576. DOI: 10.1016/j.cgh.2021.12.034. [20] HAYMART MR, MILLER DC, HAWLEY ST. Active surveillance for low-risk cancers-a viable solution to overtreatment?[J]. N Engl J Med, 2017, 377( 3): 203- 206. DOI: 10.1056/NEJMp1703787. [21] JOHANSSON M, JØRGENSEN KJ, BRODERSEN J. The benefits of screening-and its harms[J]. Lancet, 2016, 388( 10044): 563- 564. DOI: 10.1016/S0140-6736(16)31219-3. -



 PDF下载 ( 1514 KB)
PDF下载 ( 1514 KB)

 下载:
下载: