肝硬化食管胃静脉曲张二级预防患者内镜治疗后再出血的影响因素分析
DOI: 10.12449/JCH241213
Influencing factors for rebleeding after endoscopic therapy in patients with liver cirrhosis receiving secondary prevention of gastroesophageal varices
-
摘要:
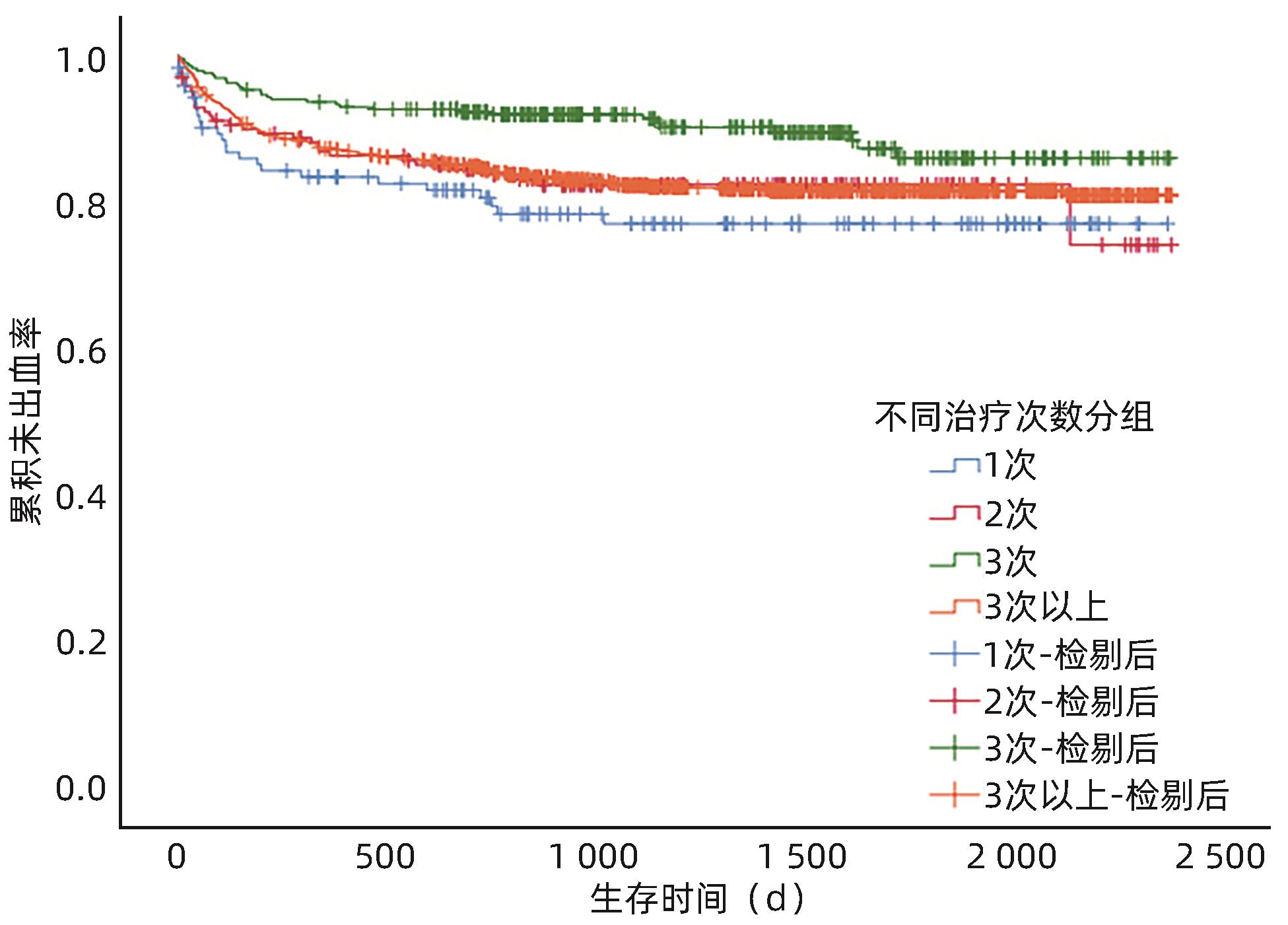
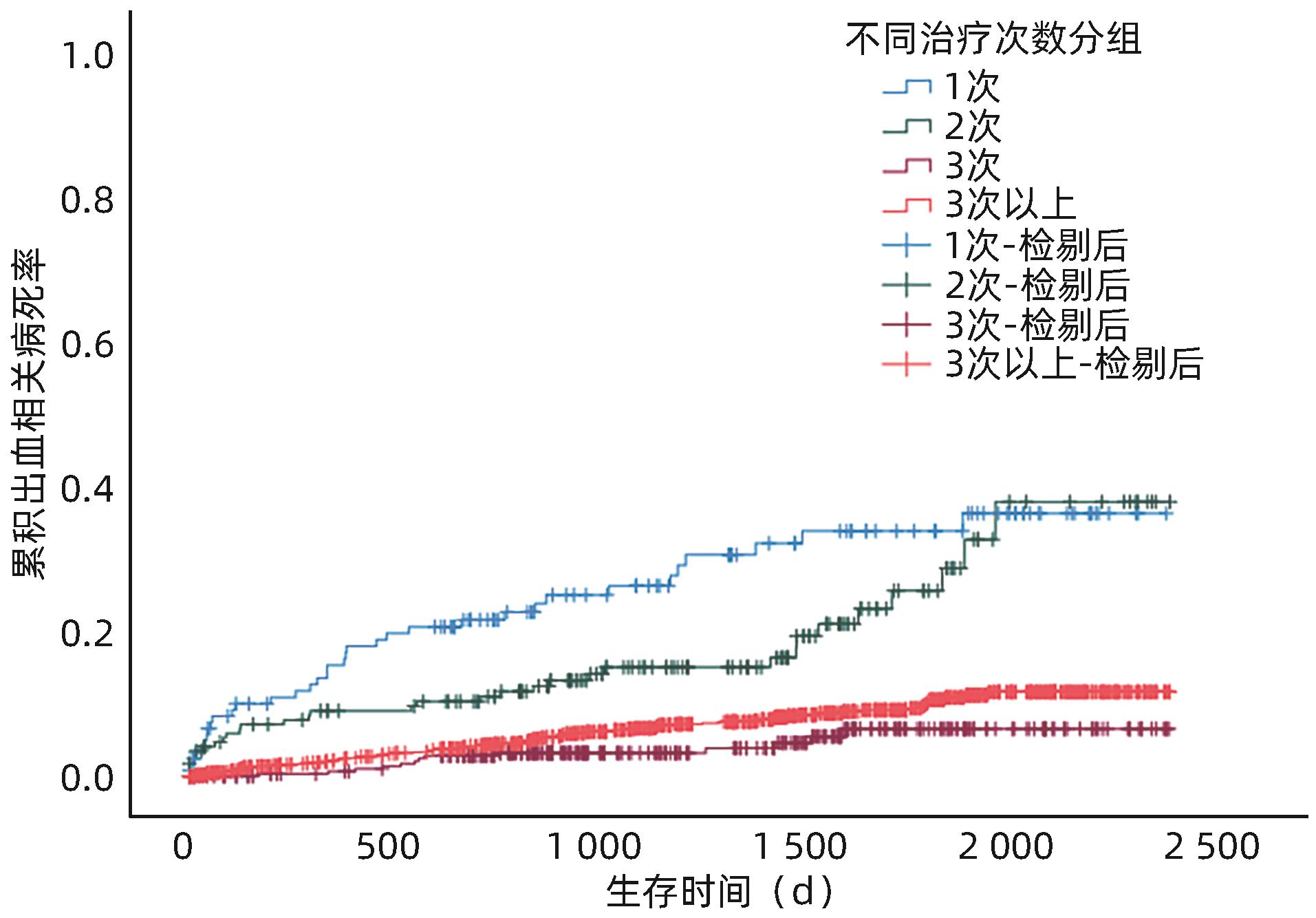
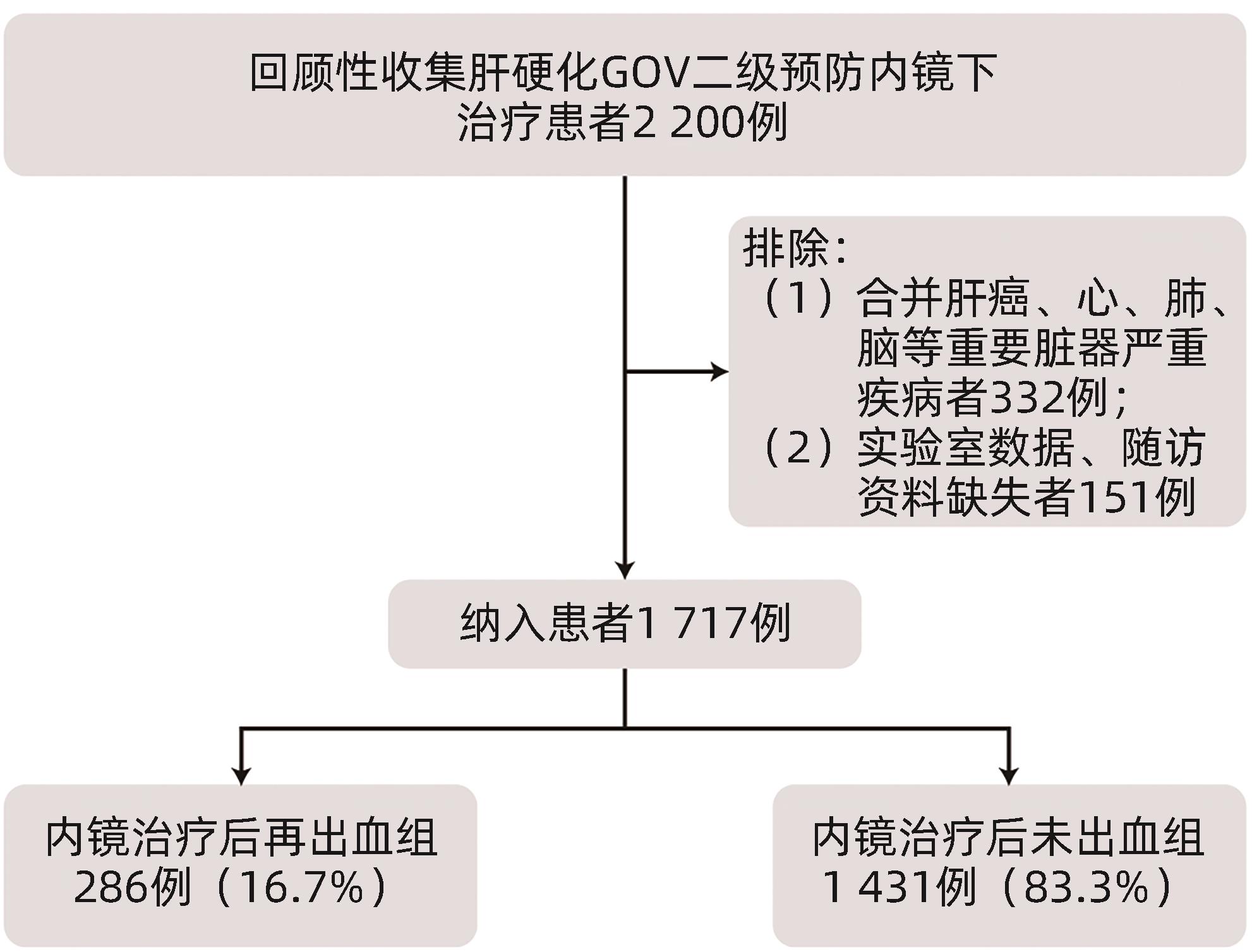
目的 探究肝硬化食管胃静脉曲张(GOV)二级预防患者经内镜治疗后再出血的影响因素,及序贯治疗次数对术后再出血的影响。 方法 选取2017年1月—2021年12月于中国人民解放军联勤保障部队第九六〇医院就诊的1 717例肝硬化GOV二级预防患者,根据内镜治疗后是否发生出血,分为未出血组和再出血组。分析患者再出血的影响因素,并研究内镜下治疗次数与再出血的关系。计数资料组间比较采用χ2检验。计量资料两组间比较采用成组t检验或Mann-Whitney U检验;多组间比较采用Kruskal-Wallis H检验,进一步两两比较采用Wilcoxon检验。应用Cox回归模型分析再出血的影响因素。Kaplan-Meier法绘制生存曲线,组间比较采用Log-rank检验。 结果 内镜治疗后286例(16.7%)患者发生再出血,1 431例(83.3%)患者未出血。两组患者比较,吸烟史、饮酒史、肝硬化病因、Hb、凝血酶原时间(PT)、凝血酶原活动度(PTA)、国际标准化比值(INR)、Alb、空腹血糖(GLU)、尿素氮(BUN)、Child-Pugh分级、APRI评分、ALBI评分、术前是否服用非选择性β受体阻滞剂(NSBB)、治疗方式、静脉曲张类型及最大静脉曲张直径等,差异均有统计学意义(P值均<0.05)。单因素Cox回归分析显示,肝硬化GOV二级预防患者再出血与吸烟史、饮酒史、肝硬化病因、术前NSBB、治疗方式、最大静脉曲张直径、Hb、PLT、PT、PTA、INR、Alb、TBil、ALP、GGT、GLU、BUN、Child-Pugh分级及ALBI评分有关(P值均<0.05);多因素Cox回归分析结果显示,Hb(HR=0.989,95%CI:0.983~0.994,P<0.001)、TBil(HR=1.020,95%CI:1.006~1.034,P=0.005)、Alb(HR=0.868,95%CI:0.758~0.994,P=0.041)、治疗方式(硬化剂HR=2.158,95%CI:1.342~3.470,P=0.002;组织胶HR=2.709,95%CI:1.343~5.462,P=0.005;套扎+硬化剂HR=3.181,95%CI:1.522~6.645,P=0.002;硬化剂+组织胶HR=1.851,95%CI:1.100~3.113,P=0.020)、ALP(HR=1.003,95%CI:1.001~1.004,P=0.002)、最大静脉曲张直径(HR=1.346,95%CI:1.119~1.618,P=0.002)是内镜治疗后再出血的独立影响因素。不同序贯治疗次数后再出血率比较结果显示,治疗3次的再出血率较1次和2次的患者再出血率低,差异均有统计学意义(χ2值分别为8.643、5.277,P值分别为0.003、0.022)。生存分析结果显示,随着治疗次数的增多,患者再出血间隔时间延长(P=0.006)、病死率降低(P<0.001)。 结论 肝硬化GOV内镜治疗后再出血的主要预测因素包括入院时TBil、ALP、Hb、Alb水平、内镜治疗方式、最大静脉曲张直径,临床中应多加强对预测因素的监测。规律内镜治疗可以降低肝硬化GOV患者再出血率和病死率,延长再出血间隔时间。 Abstract:Objective To investigate the influencing factors for rebleeding after endoscopic therapy and the effect of the number of sequential treatment sessions on postoperative rebleeding in patients with liver cirrhosis receiving secondary prevention of gastroesophageal varices (GOV). Methods A total of 1 717 patients with liver cirrhosis who received secondary prevention of GOV and attended The 960th Hospital of the PLA Joint Logistice Support Force from January 2017 to December 2021 were enrolled, and according to the presence or absence of bleeding after endoscopic therapy, they were divided into non-bleeding group and rebleeding group. The influencing factors for rebleeding were analyzed, as well as the association between the number of endoscopic treatment sessions and rebleeding. The chi-square test was used for comparison of categorical data between groups; the independent-samples t test or the Mann-Whitney U test was used for comparison of continuous data between the two groups; the Kruskal-Wallis H test was used for comparison bertween multiple groups, and the Wilcoxon test was used for further comparison between two groups. The Cox regression model was used to investigate the influencing factors for rebleeding, and the Kaplan-Meier method was used to plot survival curves, while the Log-rank test was used for comparison between groups. Results Of all patients, 286 (16.7%) experienced rebleeding after endoscopic therapy, and 1 431 (83.3%) did not experience bleeding. There were significant differences between the two groups in history of smoking and drinking, etiology of liver cirrhosis, hemoglobin (Hb), prothrombin time (PT), prothrombin activity (PTA), international normalized ratio (INR), albumin (Alb), fasting blood glucose, blood urea nitrogen, Child-Pugh class, aspartate aminotransferase-to-platelet ratio index (APRI) score, albumin-bilirubin (ALBI) score, use of non-selective beta-blocker (NSBB) before surgery, treatment modality, type of varices, and maximal varicose vein diameter (all P<0.05). The univariate Cox regression analysis showed that in the patients with liver cirrhosis who received secondary prevention of GOV, rebleeding was associated with history of smoking and drinking, etiology of liver cirrhosis, use of NSBB before surgery, treatment modality, maximal varicose vein diameter, Hb, platelet count, PT, PTA, INR, Alb, total bilirubin (TBil), alkaline phosphatase (ALP), gamma-glutamyl transpeptidase, blood glucose, Child-Pugh class, and ALBI score (all P<0.05). The multivariate Cox regression analysis showed that Hb (hazard ratio [HR]=0.989, 95% confidence interval [CI]: 0.983 — 0.994, P<0.001), TBil (HR=1.020, 95%CI: 1.006 — 1.034, P=0.005), Alb (HR=0.868, 95%CI: 0.758 — 0.994, P=0.041), treatment modality (sclerosing agent: HR=2.158, 95%CI: 1.342 — 3.470, P=0.002; tissue adhesive: HR=2.709, 95%CI: 1.343 — 5.462, P=0.005; ligation+sclerosing agent: HR=3.181, 95%CI: 1.522 — 6.645, P=0.002; sclerosing agent+tissue adhesive: HR=1.851, 95%CI: 1.100 — 3.113, P=0.020), ALP (HR=1.003, 95%CI: 1.001 — 1.004, P=0.002), and maximal varicose vein diameter (HR=1.346, 95%CI: 1.119 — 1.618, P=0.002) were independent influencing factors for rebleeding after endoscopic therapy. Comparison of rebleeding rate after different numbers of sequential treatment sessions showed that the patients treated for three sessions had a significantly lower rebleeding rate than those treated for one or two sessions (χ2=8.643 and 5.277, P=0.003 and 0.022). The survival analysis showed that with the increase in the number of treatment sessions, there was a significantly longer interval between rebleeding (P=0.006) and a significantly lower mortality rate (P<0.001). Conclusion The levels of TBil, ALP, Hb, and Alb on admission, endoscopic treatment modality, and maximal varicose vein diameter were the main predictive factors for rebleeding after endoscopic therapy for GOV in liver cirrhosis, and such predictive factors should be closely monitored in clinical practice. Regular endoscopic therapy can reduce the rebleeding and mortality rates of patients with liver cirrhosis and GOV and prolonmg the interval between rebleeding. -
Key words:
- Liver Cirrhosis /
- Esophageal and Gastric Varices /
- Endoscopy /
- Re-bleeding
-
表 1 出血组与未出血组患者基线特征比较
Table 1. Comparison of baseline characteristics of clinical data between patients in the bleeding and non-bleeding groups
项目 出血组(n=286) 未出血组(n=1 431) 统计值 P值 性别[例(%)] χ2=2.340 0.126 男 190(66.4) 882(61.6) 女 96(33.6) 549(38.4) 年龄(岁) 54(46~63) 55(49~64) Z=-1.524 0.127 吸烟史[例(%)] χ2=8.873 0.003 是 104(36.4) 395(27.6) 否 182(63.6) 1 036(72.4) 饮酒史[例(%)] χ2=3.851 0.049 是 96(33.6) 398(27.8) 否 190(66.4) 1 033(72.2) 肝硬化病因[例(%)] χ2=15.758 0.015 HBV 124(43.4) 715(50.0) 酒精 59(20.6) 205(14.3) HCV 12(4.2) 38(2.7) 自身免疫性 2(0.7) 25(1.7) HBV+酒精 9(3.1) 22(1.5) HBV+HCV 0(0.0) 1(0.1) 病因不明 80(28.0) 425(29.7) 合并糖尿病[例(%)] 66(23.1) 278(19.4) χ2=1.982 0.159 合并高血压[例(%)] 40(14.0) 184(12.9) χ2=0.267 0.605 合并冠心病[例(%)] 18(6.3) 68(4.8) χ2=1.191 0.275 手术介入史 脾切除术[例(%)] χ2=1.966 0.161 是 64(22.4) 377(26.3) 否 222(77.6) 1 054(73.7) 脾栓塞术[例(%)] χ2=1.567 0.211 是 23(8.0) 150(10.5) 否 263(92.0) 1 281(89.5) 断流术[例(%)] χ2=2.782 0.095 是 13(4.5) 104(7.3) 否 273(95.5) 1 327(92.7) 分流术[例(%)] χ2=0.403 0.526 是 2(0.7) 6(0.4) 否 284(99.3) 1 425(99.6) TIPS[例(%)] χ2=2.213 0.137 是 0(0.0) 11(0.8) 否 286(100.0) 1 420(99.2) BRTO[例(%)] χ2=0.200 0.655 是 0(0.0) 1(0.1) 否 286(100.0) 1 430(99.9) Hb(g/L) 86.0(68.0~111.5) 99.0(79.0~118.0) Z=-4.552 <0.001 WBC(×109/L) 3.34(2.29~4.82) 3.24(2.24~4.62) Z=-0.665 0.506 PLT(×109/L) 82.0(52.5~151.0) 86.0(58.0~156.3) Z=-1.593 0.111 PT(s) 14.0(13.0~15.5) 13.8(12.8~15.0) Z=-2.647 0.008 PTA(%) 69.1(59.9~79.1) 71.1(62.4~80.0) Z=-2.384 0.017 INR 1.19(1.10~1.32) 1.18(1.09~1.29) Z=-2.899 0.004 ALT(U/L) 23.0(17.0~34.5) 24.0(17.0~34.0) Z=-0.493 0.622 AST(U/L) 29.0(22.0~40.5) 29.0(22.0~38.0) Z=-0.561 0.575 Alb(g/L) 33.8(30.0~37.1) 35.3(31.4~38.5) Z=-3.624 <0.001 TBil(μmol/L) 18.0(13.4~27.0) 18.7(13.6~25.3) Z=-0.023 0.981 ALP(U/L) 83.0(63.0~117.0) 79.0(61.0~108.0) Z=-1.250 0.211 GGT(U/L) 36.00(21.75~78.25) 34.00(20.00~62.00) Z=-1.923 0.054 GLU(mmol/L) 5.88(4.84~7.50) 5.19(4.68~6.46) Z=-3.670 <0.001 表 2 再出血的影响因素分析
Table 2. Analysis of influencing factors of rebleeding
项目 单因素分析 多因素分析 HR(95%CI) P值 HR(95%CI) P值 性别 男 1.000 女 0.819(0.641~1.047) 0.112 年龄 0.992(0.981~1.002) 0.130 吸烟史 无 1.000 1.000 有 1.452(1.141~1.848) 0.002 1.321(0.968~1.801) 0.079 饮酒史 无 1.000 1.000 有 1.294(1.012~1.654) 0.040 0.816(0.523~1.273) 0.370 肝硬化病因 HBV 1.000 1.000 酒精 1.612(1.182~2.198) 0.003 1.324(0.823~2.131) 0.248 HCV 1.686(0.932~3.049) 0.084 1.546(0.842~2.837) 0.160 自身免疫性 0.489(0.121~1.976) 0.315 0.418(0.102~1.722) 0.227 HBV+酒精 2.192(1.114~4.313) 0.023 2.112(0.981~4.548) 0.056 病因不明 1.098(0.829~1.455) 0.513 0.997(0.736~1.350) 0.985 合并糖尿病 1.223(0.929~1.610) 0.152 合并高血压 1.073(0.768~1.499) 0.680 合并冠心病 1.343(0.833~2.164) 0.226 断流术 否 1.000 是 0.627(0.359~1.094) 0.100 分流术 否 1.000 是 1.463(0.364~5.879) 0.592 TIPS 否 1.000 是 0.049(0.000~21.833) 0.333 术前服用NSBB 否 1.000 是 1.327(1.045~1.686) 0.020 1.240(0.962~1.597) 0.096 术后应用PPI 否 1.000 是 1.364(0.508~3.662) 0.538 术后应用抗生素 否 1.000 是 0.953(0.732~1.243) 0.724 住院时间 1.002(0.983~1.021) 0.857 治疗次数 1.012(0.991~1.035) 0.266 脾切除术 否 1.000 是 0.807(0.611~1.066) 0.131 脾栓塞术 否 1.000 是 0.739(0.483~1.132) 0.165 Hb 0.988(0.984~0.993) <0.001 0.989(0.983~0.994) <0.001 WBC 1.033(0.991~1.078) 0.124 PLT 0.998(0.997~1.000) 0.033 0.999(0.997~1.000) 0.106 PT 1.072(1.037~1.108) <0.001 0.908(0.750~1.100) 0.326 PTA 0.989(0.980~0.997) 0.011 1.004(0.993~1.016) 0.468 项目 单因素分析 多因素分析 HR(95%CI) P值 HR(95%CI) P值 INR 2.341(1.626~3.370) <0.001 5.661(0.636~50.404) 0.120 ALT 0.999(0.996~1.003) 0.789 AST 1.000(0.999~1.001) 0.901 Alb 0.957(0.937~0.978) <0.001 0.868(0.758~0.994) 0.041 TBil 1.011(1.004~1.018) 0.002 1.020(1.006~1.034) 0.005 ALP 1.002(1.001~1.004) 0.001 1.003(1.001~1.004) 0.002 GGT 1.001(1.001~1.002) <0.001 1.001(1.000~1.001) 0.104 GLU 1.050(1.016~1.086) 0.004 1.019(0.980~1.060) 0.347 CRE 1.000(0.097~1.003) 0.918 BUN 1.059(1.024~1.096) 0.001 1.020(0.980~1.063) 0.331 血清钾 1.210(0.909~1.612) 0.192 血清钠 0.971(0.938~1.004) 0.088 腹水量 无 1.000 少量 0.970(0.741~1.271) 0.827 中量 1.529(0.902~2.592) 0.115 大量 1.487(0.945~2.339) 0.086 肝性脑病分级 无 1.000 1~2级 0.932(0.232~3.743) 0.920 3~4级 2.212(0.550~8.892) 0.263 门静脉血栓形成 1.038(0.796~1.354) 0.784 脾功能亢进 1.165(0.923~1.471) 0.199 治疗方式 0.001 EVL 1.000 1.000 EIS 1.893(1.189~3.015) 0.007 2.158(1.342~3.470) 0.002 ECI 4.391(2.262~8.523) <0.001 2.709(1.343~5.462) 0.005 EVL+EIS 3.334(1.607~6.917) 0.001 3.181(1.522~6.645) 0.002 EVL+ECI 1.628(0.998~2.656) 0.051 1.284(0.775~2.126) 0.331 EIS+ECI 1.633(0.978~2.727) 0.061 1.851(1.100~3.113) 0.020 EVL+EIS+ECI 2.008(0.889~4.536) 0.094 1.504(0.648~3.492) 0.342 静脉曲张类型 0.066 单纯食管静脉曲张 1.000 食管静脉曲张合并胃静脉曲张 1.360(0.970~1.900) 0.074 单纯胃静脉曲张 2.560(1.010~6.480) 0.048 最大静脉曲张直径 1.310(1.110~1.560) 0.002 1.346(1.119~1.618) 0.002 红色征 0.573 阴性 1.000 阳性 1.070(0.850~1.360) 0.573 GOV程度 0.081 轻度 1.000 中度 1.430(1.040~1.960) 0.029 重度 1.200(0.870~1.650) 0.275 Child-Pugh分级 A级 1.000 1.000 B级 1.338(1.049~1.707) 0.019 0.979(0.712~1.347) 0.897 C级 2.222(1.174~4.206) 0.014 0.837(0.365~1.920) 0.675 APRI评分 1.003(0.985~1.021) 0.768 FIB-4评分 1.007(0.997~1.017) 0.161 ALBI评分 1.617(1.279~2.045) <0.001 0.209(0.043~1.010) 0.052 MELD评分 1.007(0.980~1.035) 0.605 表 3 不同治疗次数患者出血率与出血平均间隔时间的比较
Table 3. Comparison of bleeding rate and mean interval of bleeding by number of treatments
治疗次数 例数 出血率(%) 出血平均间隔时间(d) 1次 125 20.8 101(30~344) 2次 171 17.5 105(29~5 412) 3次 304 10.21)2) 201(85~753)1) 3次以上 1 117 17.83) 150(55~448) 统计值 χ2=11.860 H=5.996 P值 0.008 0.112 注:与治疗1次比较,1)P<0.05;与治疗2次比较,2)P<0.05;与治疗3次比较,3)P<0.05。
表 4 不同治疗次数患者不同时间的出血率比较
Table 4. Comparison of bleeding rates by number of treatments by duration
时间 1次 2次 3次 3次以上 χ2值 P值 <5 d 1.6%(2/125) 2.3%(4/171) 0.3%(1/304) 0.3%(3/1 117) 13.587 0.004 5~42 d 4.0%(5/125) 4.7%(8/171) 1.3%(4/304) 2.8%(31/1 117) 5.349 0.148 43~180 d 8.0%(10/125) 2.9%(5/171) 3.0%(9/304) 6.6%(74/1 117) 9.692 0.019 >180 d 7.2%(9/125) 7.6%(13/171) 5.6%(17/304) 8.1%(91/1 117) 2.255 0.521 -
[1] IWAKIRI Y, TREBICKA J. Portal hypertension in cirrhosis: Pathophysiological mechanisms and therapy[J]. JHEP Rep, 2021, 3( 4): 100316. DOI: 10.1016/j.jhepr.2021.100316. [2] LUNOVA M, FRANKOVA S, GOTTFRIEDOVA H, et al. Portal hypertension is the main driver of liver stiffness in advanced liver cirrhosis[J]. Physiol Res, 2021, 70( 4): 563- 577. DOI: 10.33549/physiolres.934626. [3] KIM KR, JUN CH, CHO KM, et al. Can proton pump inhibitors reduce rebleeding following Histoacryl sclerotherapy for gastric variceal hemorrhage?[J]. Korean J Intern Med, 2015, 30( 5): 593- 601. DOI: 10.3904/kjim.2015.30.5.593. [4] ZHAO Y. Application value of endoscopic ultrasonography in precise devascularization of esophageal and gastric varices caused by portal hypertension[D]. Kaifeng: Henan University, 2020.赵一. 超声内镜在门脉高压所致食管胃静脉曲张精准断流术中的应用价值[D]. 开封: 河南大学, 2020. [5] MA L, TSENG Y, LUO T, et al. Risk stratification for secondary prophylaxis of gastric varices due to portal hypertension[J]. Dig Liver Dis, 2019, 51( 12): 1678- 1684. DOI: 10.1016/j.dld.2019.05.020. [6] LIU LM, ZHANG CQ. Advances in high risk factors of rebleeding after endoscopic treatment of esophagogastric variceal bleeding[J/CD]. Chin J Dig Med Imageology Electron Ed, 2022, 12( 4): 236- 240. DOI: 10.3877/cma.j.issn.2095-2015.2022.04.010.刘黎明, 张春清. 食管-胃底静脉曲张破裂出血内镜治疗后再出血高危因素研究进展[J/CD]. 中华消化病与影像杂志(电子版), 2022, 12( 4): 236- 240. DOI: 10.3877/cma.j.issn.2095-2015.2022.04.010. [7] GUO YL, XU BH, LIU X, et al. Risk factors analysis of early rebleeding after endoscopic treatment of esophageal varices[J]. Chin J Dig Endosc, 2018, 35( 2): 89- 93. DOI: 10.3760/cma.j.issn.1007-5232.2018.02.003.郭雅丽, 徐宝宏, 刘贤, 等. 食管静脉曲张内镜治疗术后早期再出血的危险因素分析[J]. 中华消化内镜杂志, 2018, 35( 2): 89- 93. DOI: 10.3760/cma.j.issn.1007-5232.2018.02.003. [8] GIRI S, SUNDARAM S, JEARTH V, et al. Predictors of early bleeding after endoscopic variceal ligation for esophageal varices: A systematic review and meta-analysis[J]. Clin Exp Hepatol, 2022, 8( 4): 267- 277. DOI: 10.5114/ceh.2022.123096. [9] ZHANG N, PENG CY, ZHANG F, et al. Clinical value of regular endoscopic treatment for esophageal and gastric variceal bleeding in patients with liver cirrhosis[J]. Chin J Dig Endosc, 2022, 39( 5): 384- 387. DOI: 10.3760/cma.j.cn321463-20210113-00760.张娜, 彭春艳, 张峰, 等. 肝硬化食管胃静脉曲张破裂出血行规律内镜下治疗的临床价值[J]. 中华消化内镜杂志, 2022, 39( 5): 384- 387. DOI: 10.3760/cma.j.cn321463-20210113-00760. [10] Chinese Society of Hepatology, Chinese Society of Gastroenterology, Chinese Society of Digestive Endoscopology of Chinese Medical Association. Guidelines on the management of esophagogastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2023, 39( 3): 527- 538.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会消化内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2023, 39( 3): 527- 538. [11] Esophagageal and Gastric Varices Group of Digestive Endoscopy Branch of Chinese Medical Association. Tentative guidelines for endoscopic diagnosis and treatment of varicosity and variceal bleeding in digestive tract(2009)[J]. Chin J Dig Endosc, 2010, 27( 1): 1- 4. DOI: 10.3760/cma.j.issn.1007-5232.2010.01.001.中华医学会消化内镜学分会食管胃静脉曲张学组. 消化道静脉曲张及出血的内镜诊断和治疗规范试行方案(2009年)[J]. 中华消化内镜杂志, 2010, 27( 1): 1- 4. DOI: 10.3760/cma.j.issn.1007-5232.2010.01.001. [12] MOSTAFA EF, MOHAMMAD AN. Incidence and predictors of rebleeding after band ligation of oesophageal varices[J]. Arab J Gastroenterol, 2014, 15( 3-4): 135- 141. DOI: 10.1016/j.ajg.2014.10.002. [13] HUANG C, SU N, WU SL, et al. Risk factors of early rebleeding after endoscopic variceal ligation[J]. J Clin Intern Med, 2019, 36( 4): 264- 266. DOI: 10.3969/j.issn.1001-9057.2019.04.014.黄超, 苏宁, 吴胜兰, 等. 内镜下食管静脉曲张套扎术后早期再出血的危险因素分析[J]. 临床内科杂志, 2019, 36( 4): 264- 266. DOI: 10.3969/j.issn.1001-9057.2019.04.014. [14] ZHANG Y. Meta-analysis of risk factors of early rebleeding after endoscopic variceal ligation[D]. Changchun: Jilin University, 2023.张赟. 食管静脉曲张内镜下套扎术后早期再出血危险因素的Meta分析[D]. 长春: 吉林大学, 2023. [15] DROLZ A, SCHRAMM C, SEIZ O, et al. Risk factors associated with bleeding after prophylactic endoscopic variceal ligation in cirrhosis[J]. Endoscopy, 2021, 53( 3): 226- 234. DOI: 10.1055/a-1214-5355. [16] JIMÉNEZ ROSALES R, MARTÍNEZ-CARA JG, VADILLO-CALLES F, et al. Analysis of rebleeding in cases of an upper gastrointestinal bleed in a single center series[J]. Rev Esp Enferm Dig, 2019, 111( 3): 189- 192. DOI: 10.17235/reed.2018.5702/2018. [17] ZHONG BH, WANG JP, LIN JH, et al. Risk assessment and prevention of gastroesophageal varices and variceal hemorrhage in cirrhosis[J]. Chin J Pract Intern Med, 2013, 33( 9): 690- 693.钟碧慧, 王锦萍, 林菁华, 等. 肝硬化食管胃底静脉曲张破裂出血风险评估及预防策略[J]. 中国实用内科杂志, 2013, 33( 9): 690- 693. [18] ZHAO MY, WU XR, LI HX, et al. Study on correlation between serum 25-hydroxyvitamin D3 level and esophageal variceal bleeding in cirrhotic patients[J]. Chin J Hepatol, 2019, 27( 5): 358- 362. DOI: 10.3760/cma.j.issn.1007-3418.2019.05.007.赵明远, 武希润, 李红霞, 等. 血清25羟维生素D3的水平与肝硬化食管静脉曲张破裂出血的相关性[J]. 中华肝脏病杂志, 2019, 27( 5): 358- 362. DOI: 10.3760/cma.j.issn.1007-3418.2019.05.007. [19] ZHANG Q, SHI K, WANG XB. Developing the prediction model of esophagogastric variceal rebleeding in patients with liver cirrhosis based on artificial neural network[J]. J Clin Hepatol, 2022, 38( 11): 2493- 2498. DOI: 10.3969/j.issn.1001-5256.2022.11.011.张群, 时克, 王宪波. 肝硬化食管胃底静脉曲张破裂出血患者再出血预测模型的建立[J]. 临床肝胆病杂志, 2022, 38( 11): 2493- 2498. DOI: 10.3969/j.issn.1001-5256.2022.11.011. [20] YUAN XY, HUANG YQ, JIANG M. Influence of hyponatremia on the condition and prognosis of patients with liver cirrhosis[J]. J China Med Univ, 2019, 48( 11): 1003- 1006. DOI: 10.12007/j.issn.0258-4646.2019.11.010.袁晓艳, 黄颖秋, 姜敏. 低钠血症对肝硬化患者病情和预后的影响[J]. 中国医科大学学报, 2019, 48( 11): 1003- 1006. DOI: 10.12007/j.issn.0258-4646.2019.11.010. [21] ZHANG XB, LI HP, LU CL, et al. Relationship between serum sodium level and liver function and complications in patients with decompensated cirrhosis[J]. Anhui Med J, 2019, 40( 6): 673- 676. DOI: 10.3969/j.issn.1000-0399.2019.06.022.张小宝, 李华平, 陆春雷, 等. 失代偿期肝硬化患者血清钠水平与肝功能及并发症的关系[J]. 安徽医学, 2019, 40( 6): 673- 676. DOI: 10.3969/j.issn.1000-0399.2019.06.022. [22] GUO H, ZHANG M, ZHANG N, et al. Number of endoscopic sessions to eradicate varices identifies high risk of rebleeding in cirrhotic patients[J]. BMC Gastroenterol, 2022, 22( 1): 213. DOI: 10.1186/s12876-022-02283-0. [23] RÍOS E, SIERRALTA A, ABARZÚA M, et al. Comparison of band ligation with sclerotherapy for the treatment of bleeding esophageal varices[J]. Rev Med Chil, 2012, 140( 6): 713- 718. DOI: 10.4067/s0034-98872012000600003. [24] YANG YJ. Comparative analysis of ligation, sclerosing agent and drug therapy in patients with esophageal varices bleeding[J]. Guide China Med, 2011, 9( 19): 288- 289.杨悦军. 食管静脉曲张破裂出血患者套扎术、硬化剂、药物治疗方法比较分析[J]. 中国医药指南, 2011, 9( 19): 288- 289. [25] XIANG Y, WANG X, MEI XC, et al. Comparative analysis of endoscopic ligation and tissue adhesive injection for tortuous gastric varices[J]. Chin J Dig Endosc, 2021, 38( 11): 901- 906. DOI: 10.3760/cma.j.cn321463-20210223-00123.项艺, 王曦, 梅雪灿, 等. 蔓状隆起型胃底静脉曲张内镜下套扎与组织胶注射治疗的对比分析[J]. 中华消化内镜杂志, 2021, 38( 11): 901- 906. DOI: 10.3760/cma.j.cn321463-20210223-00123. [26] HUANG XQ, WU L, JIANG SY, et al. Clinical evaluation of different modalities in emergency endoscopic treatment of esophageal variceal bleeding[J]. J Chin Physician, 2022, 24( 5): 653- 657. DOI: 10.3760/cma.j.cn431274-20220419-00361.黄晓铨, 吴玲, 姜思雨, 等. 食管静脉曲张出血的急诊内镜治疗选择与疗效评价[J]. 中国医师杂志, 2022, 24( 5): 653- 657. DOI: 10.3760/cma.j.cn431274-20220419-00361. [27] SONG ZM, CHEN YM, YANG M. Comparison of clinical evaluation of endoscopic therapy for esophageal variceal bleeding[J]. Chin J Curr Adv Gen Surg, 2010, 13( 3): 199- 201. DOI: 10.3969/j.issn.1009-9905.2010.03.009.宋振梅, 陈艳明, 杨猛. 内镜下硬化与套扎治疗食管静脉曲张破裂出血疗效比较[J]. 中国现代普通外科进展, 2010, 13( 3): 199- 201. DOI: 10.3969/j.issn.1009-9905.2010.03.009. -



 PDF下载 ( 1261 KB)
PDF下载 ( 1261 KB)

 下载:
下载: