慢性乙型肝炎患者发生肝癌的危险因素分析及列线图预测模型构建
DOI: 10.12449/JCH241214
Risk factors for liver cancer in chronic hepatitis B patients and construction of a nomogram prediction model
-
摘要:
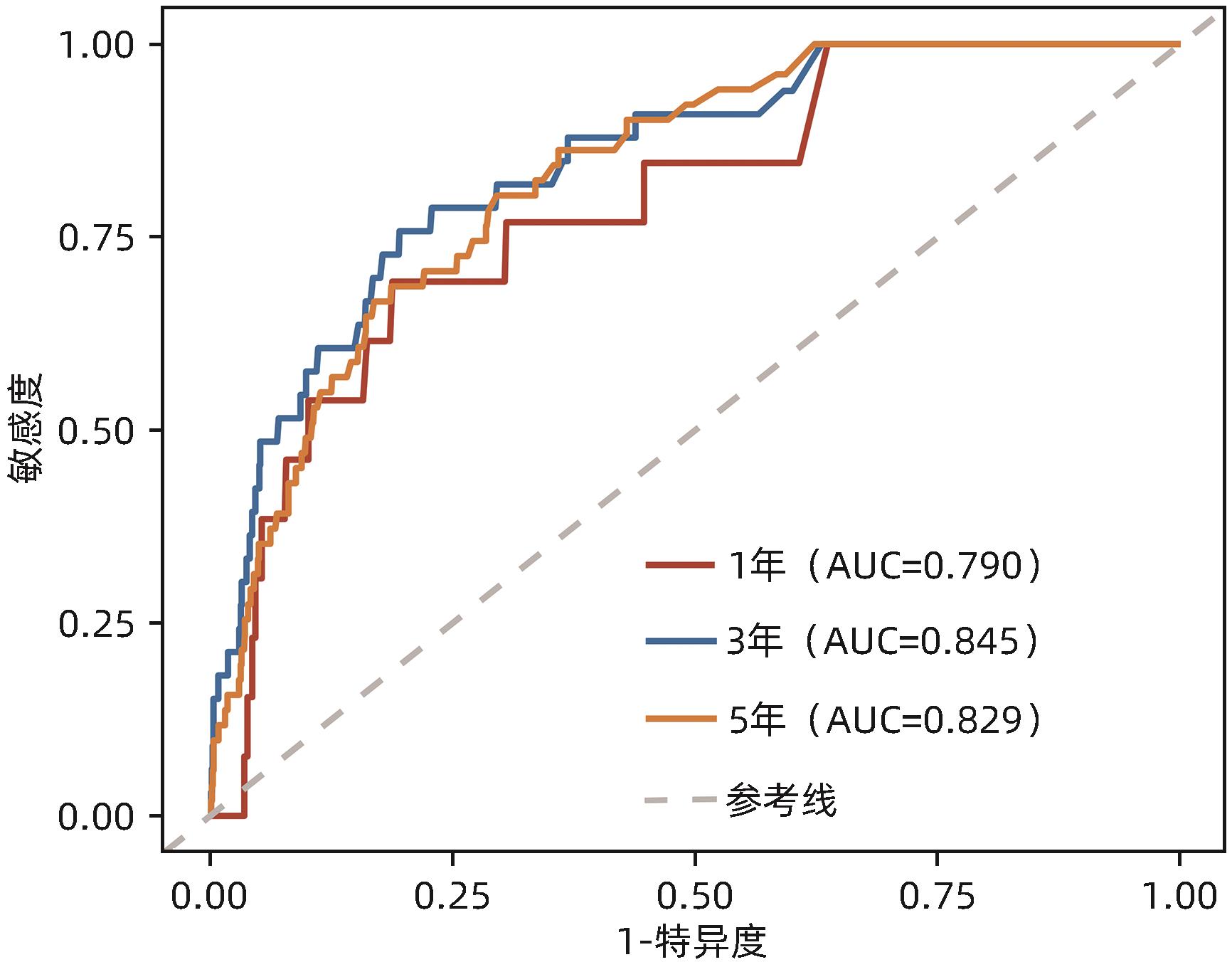
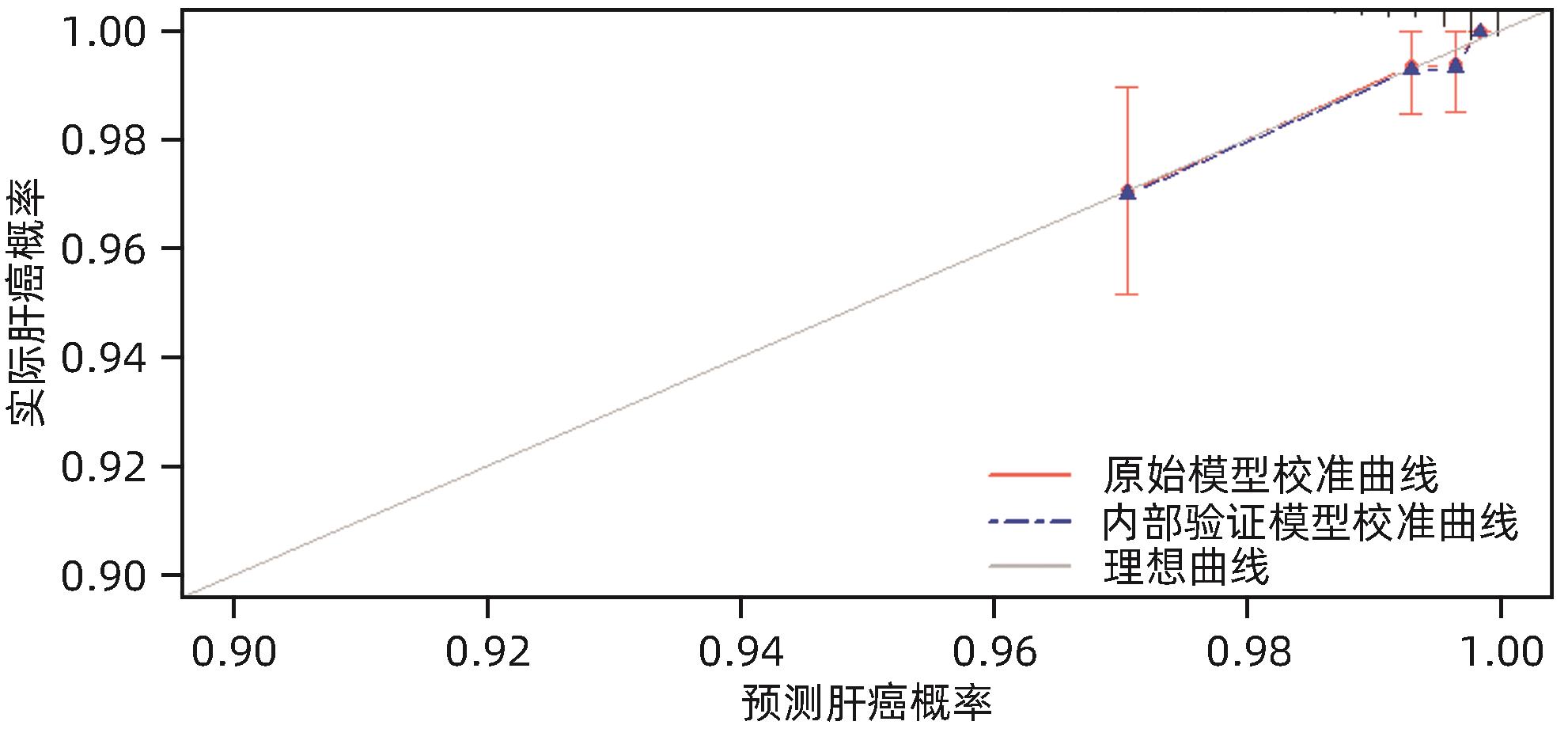
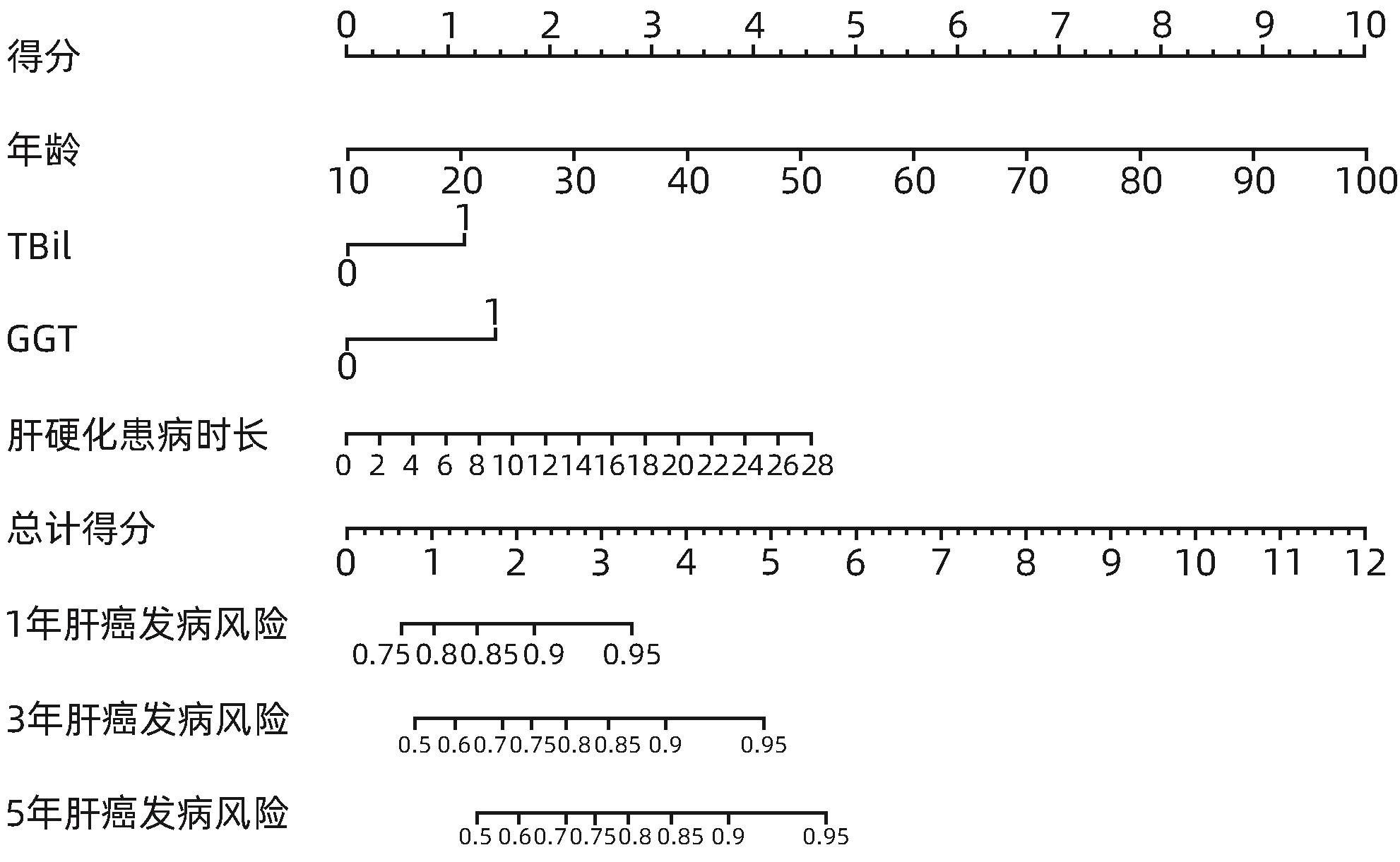
目的 通过分析启东市慢性乙型肝炎(CHB)临床队列患者肝癌发病的危险因素,构建预测CHB患者肝癌发病风险的列线图模型。 方法 选取2016年1月1日—12月31日于启东市第三人民医院肝病门诊就诊的年龄≥18周岁的CHB患者,均采用结构式问卷进行问卷调查。将肝癌发病作为主要研究结局,通过启东市癌症登记处获取队列研究结局。比较肝癌发病组与未发病组的基线临床特征。计量资料两组间比较采用成组t检验或Mann-Whitney U检验。计数资料组间比较采用χ 2检验或Fisher精确概率法。采用单因素Cox回归模型探索CHB患者肝癌发病风险的影响因素,计算风险比(HR)和95%可信区间(95%CI),将单因素Cox回归模型中有意义的变量纳入LASSO回归进行筛选,所得特征变量纳入多因素Cox回归以建立预测模型。采用列线图使复杂模型可视化,通过受试者工作特征曲线(ROC曲线)、一致性指数(C-index)和校准曲线评估列线图的预测效能,应用决策曲线评估列线图的临床实用性。 结果 共选取CHB患者1 479例,排除已确诊为肝癌者58例,检验指标缺失者15例及基线问卷重要信息缺失者164例,最终纳入研究对象1 242例。截至2023年12月31日,中位随访时间7.71年,共67例肝癌新发病例,肝癌发病密度为729.78/10万人年。肝癌组与非肝癌组患者比较,年龄、性别、受教育程度、肝硬化情况、肝硬化患病时间、糖尿病史、白蛋白、TBil、DBil、AST、ALT、GGT、ALP差异均有统计学意义(P值均<0.05)。多因素Cox回归分析显示,年龄增长(HR=1.07,95%CI:1.05~1.10,P<0.001)、较高的TBil水平(HR=1.98,95%CI:1.15~3.42,P=0.014)、较高的GGT水平(HR=2.41,95%CI:1.43~4.08,P=0.001)及较长的肝硬化患病时间(HR=1.09,95%CI:1.02~1.15,P=0.009)是CHB患者肝癌发病的独立危险因素,基于上述4项指标构建列线图,预测CHB患者在1、3、5年时肝癌发病风险的ROC曲线下面积分别为0.790、0.845和0.829,并经bootstrap重抽样法进行内部验证(C-index=0.778),校准曲线提示预测模型具有良好稳定性;决策曲线分析提示预测模型具有临床实用性。 结论 年龄增长、较高的TBil和GGT水平及较长的肝硬化患病时间是CHB患者肝癌发病的独立危险因素,据此建立的列线图模型具有较好的预测价值,该模型可用于临床实践,以帮助制订肝癌的长期监测策略。 Abstract:Objective To investigate the risk factors for liver cancer in patients with chronic hepatitis B (CHB) in the Qidong Chronic Hepatitis B cohort, and to construct a nomogram model for predicting the risk of liver cancer in CHB patients. Methods A structured questionnaire survey was conducted among the CHB patients, aged ≥18 years, who attended the outpatient service of Qidong Third People’s Hospital from January 1 to December 31, 2016. The onset of liver cancer was defined as the primary outcome, and the outcomes of the cohort were obtained from Qidong Cancer Registry. Baseline clinical features were compared;between the liver cancer group and the non-liver cancer group. The independent-samples t test or the Mann-Whitney U test was used for comparison of continuous data between two groups, and the chi-square test or the Fisher’s exact test was used for comparison of categorical data between groups. The Cox regression model was used to analyze the risk factors for liver cancer in CHB patients and calculate their hazard ratio (HR) and 95% confidence interval (CI); the variables with statistical significance in the univariate Cox regression analysis were included in the LASSO regression analysis, and then the variables obtained were included in the multivariate Cox regression analysis to establish a predictive model. The nomogram was used to visualize the complex model. The receiver operating characteristic (ROC) curve, index of concordance (C-index), and the calibration curve were used to assess the predictive efficacy of the model, and the decision curve was used to evaluate the clinical practicability of the nomogram. Results A total of 1 479 CHB patients were selected, among whom 58 patients with a confirmed diagnosis of liver cancer, 15 with missing data on testing indicators, and 164 with missing data on important information in the questionnaire were excluded, and finally 1 242 subjects were included in the study. Up to December 31, 2023, there were 67 new cases of liver cancer after a median follow-up time of 7.71 years, and the incidence density of liver cancer was 729.78/100,000 person-years. There were significant differences between the liver cancer group and the non-liver cancer group in age, sex, educational level, liver cirrhosis, duration of liver cirrhosis, history of diabetes mellitus, albumin, total bilirubin (TBil), direct bilirubin, aspartate aminotransferase, aspartate aminotransferase, gamma-glutamyl transpeptidase (GGT), and alkaline phosphatase (all P<0.05). The multivariate Cox regression analysis showed that the increase in age (HR=1.07, 95%CI: 1.05 — 1.10, P<0.001), a relatively high level of TBil (HR=1.98, 95%CI: 1.15 — 3.42, P=0.014), a relatively high level of GGT (HR=2.41, 95%CI: 1.43 — 4.08, P=0.001), and a long duration of liver cirrhosis (HR=1.09, 95%CI: 1.02 — 1.15, P=0.009) were independent risk factors for liver cancer in CHB patients. A nomogram prediction model was constructed based on the above four indicators, with an area under the ROC curve of 0.790, 0.845, and 0.829, respectively, in predicting the risk of liver cancer in CHB patients at 1, 3, and 5 years, and the bootstrap resampling method was used for internal validation and showed a C-index of 0. 778. The calibration curve showed that the prediction model had good stability, and the decision curve showed that it had certain clinical practicability. Conclusion The increase in age, relatively high levels of TBil and GGT, and a long duration of liver cirrhosis are independent risk factors for liver cancer in CHB patients, and the nomogram model constructed based on these factors has a good predictive value and can be used in clinical practice to help develop strategies for the long-term monitoring of liver cancer. -
Key words:
- Hepatitis B, Chronic /
- Liver Neoplasms /
- Risk Factors /
- Nomograms
-
表 1 研究对象基线特征
Table 1. Baseline characteristics of the study population
变量 总计(n=1 242) 非肝癌组(n=1 175) 肝癌组(n=67) 统计值 P值 年龄(岁) 52.00(45.00~59.00) 52.00(44.00~58.00) 59.00(54.00~71.00) Z=-8.244 <0.001 年龄段[例(%)] χ 2=23.745 <0.001 <60岁 1 018(82.0) 978(83.2) 40(59.7) ≥60岁 224(18.0) 197(16.8) 27(40.3) 性别[例(%)] χ 2=5.341 0.021 男 741(59.7) 692(58.9) 49(73.1) 女 501(40.3) 483(41.1) 18(26.9) 婚姻情况[例(%)] 0.644 离异 1(0.1) 1(0.1) 0(0.0) 未婚 21(1.7) 21(1.8) 0(0.0) 已婚 1 220(98.2) 1 153(98.1) 67(100.0) 受教育程度[例(%)] χ 2=9.708 0.021 小学 165(13.3) 148(12.6) 17(25.4) 初中 687(55.3) 658(56.0) 29(43.3) 高中 231(18.6) 218(18.6) 13(19.4) 大专及以上 159(12.8) 151(12.9) 8(11.9) 吸烟[例(%)] χ 2=1.960 0.185 否 1 024(82.4) 973(82.8) 51(76.1) 是 218(17.6) 202(17.2) 16(23.9) 饮酒[例(%)] 0.263 否 1 173(94.4) 1 112(94.6) 61(91.0) 是 69(5.6) 63(5.4) 6(9.0) 饮茶[例(%)] 0.621 否 1 222(98.4) 1 155(98.3) 67(100.0) 是 20(1.6) 20(1.7) 0(0.0) 体育锻炼[例(%)] >0.05 否 1 219(98.1) 1 153(98.1) 66(98.5) 是 23(1.9) 22(1.9) 1(1.5) 肝硬化[例(%)] χ 2=45.677 <0.001 否 957(77.1) 928(79.0) 29(43.3) 是 285(22.9) 247(21.0) 38(56.7) 肝硬化患病时间(年) 0.00(0.00~0.00) 0.00(0.00~0.00) 3.00(0.00~9.00) W=24 578 <0.001 糖尿病史[例(%)] 0.030 否 1 197(96.4) 1 136(96.7) 61(91.0) 是 45(3.6) 39(3.3) 6(9.0) 家族史[例(%)] χ 2=1.279 0.494 无 607(48.9) 574(48.9) 33(49.3) 乙型肝炎 447(36.0) 426(36.3) 21(31.3) HBV相关肝癌 188(15.1) 175(14.9) 13(19.4) HBV DNA[例(%)] 0.332 低于检测下限 1 021(82.2) 967(82.3) 54(80.6) >500~104拷贝/mL 73(5.9) 70(6.0) 3(4.5) >104~106拷贝/mL 69(5.6) 62(5.3) 7(10.4) >106拷贝/mL 79(6.4) 76(6.5) 3(4.5) 总蛋白[例(%)] 0.894 <60 g/L 1(0.1) 1(0.1) 0(0.0) 60~80 g/L 906(72.9) 856(72.9) 50(74.6) >80 g/L 335(27.0) 318(27.1) 17(25.4) 变量 总计(n=1 242) 非肝癌组(n=1 175) 肝癌组(n=67) 统计值 P值 白蛋白[例(%)] 0.026 <35 g/L 5(0.4) 3(0.3) 2(3.0) ≥35 g/L 1 237(99.6) 1 172(99.7) 65(97.0) TBil[例(%)] χ 2=15.429 <0.001 <21.80 μmol/L 1 071(86.2) 1 024(87.1) 47(70.1) ≥21.80 μmol/L 171(13.8) 151(12.9) 20(29.9) DBil[例(%)] χ 2=14.176 <0.001 <6.84 μmol/L 971(78.2) 931(79.2) 40(59.7) ≥6.84 μmol/L 271(21.8) 244(20.8) 27(40.3) GGT χ 2=20.306 <0.001 <50 U/L 1 054(84.9) 1 010(86.0) 44(65.7) ≥50 U/L 188(15.1) 165(14.0) 23(34.3) ALP 0.002 <135 U/L 1 176(94.7) 1 119(95.2) 57(85.1) ≥135 U/L 66(5.3) 56(4.8) 10(14.9) ALT[例(%)] χ 2=6.198 0.022 <40 U/L 968(77.9) 924(78.6) 44(65.7) ≥40 U/L 274(22.1) 251(21.4) 23(34.3) AST[例(%)] 0.003 <50 U/L 1 150(92.6) 1 095(93.2) 55(82.1) ≥50 U/L 92(7.4) 80(6.8) 12(17.9) HBsAg水平[例(%)] χ 2=0.641 0.712 <1 000 IU/L 206(16.6) 194(16.5) 12(17.9) 1 000~10 000 IU/L 465(37.4) 443(37.7) 22(32.8) >10 000 IU/L 571(46.0) 538(45.8) 33(49.3) HBeAg[例(%)] χ 2=0.007 0.933 阴性 96(7.7) 91(7.7) 5(7.5) 阳性 1 146(92.3) 1 084(92.3) 62(92.5) 表 2 Cox回归分析结果
Table 2. Results of Cox regression analysis
变量 单因素Cox回归 多因素Cox回归 HR(95%CI) P值 HR(95%CI) P值 年龄 1.09(1.07~1.11) <0.001 1.07(1.05~1.10) <0.001 年龄段 <60岁 Ref ≥60岁 3.22(1.97~5.24) <0.001 性别 女 Ref 男 1.88(1.09~3.22) 0.022 受教育程度 小学 Ref 初中 0.40(0.22~0.73) 0.003 高中 0.53(0.26~1.09) 0.086 大专及以上 0.47(0.20~1.10) 0.081 吸烟 否 Ref 是 1.50(0.85~2.62) 0.159 饮酒 否 Ref 是 1.73(0.75~3.99) 0.202 体育锻炼 否 Ref 是 0.79(0.11~5.71) 0.818 肝硬化 否 Ref Ref 是 4.63(2.86~7.51) <0.001 1.41(0.67~3.03) 0.362 肝硬化患病时间 1.14(1.10~1.18) <0.001 1.09(1.02~1.15) 0.009 糖尿病史 否 Ref 是 2.76(1.19~6.38) 0.018 家族史 无 Ref 乙型肝炎 0.86(0.50~1.49) 0.593 HBV相关肝癌 1.37(0.75~2.52) 0.434 HBV DNA 低于检测下限 Ref >500~104拷贝/mL 0.79(0.25~2.52) 0.688 >104~106拷贝/mL 2.01(0.91~4.41) 0.083 >106拷贝/mL 0.72(0.22~2.30) 0.577 白蛋白 <35 g/L Ref ≥35 g/L 0.11(0.03~0.44) 0.002 TBil <21.80 μmol/L Ref Ref ≥21.80 μmol/L 2.85(1.69~4.80) <0.001 1.98(1.15~3.42) 0.014 DBil <6.84 μmol/L Ref ≥6.84 μmol/L 2.54(1.56~4.13) <0.001 变量 单因素Cox回归 多因素Cox回归 HR(95%CI) P值 HR(95%CI) P值 GGT <50 U/L Ref Ref ≥50 U/L 3.19(1.89~5.21) <0.001 2.41(1.43~4.08) 0.001 ALP <135 U/L Ref ≥135 U/L 3.43(1.75~6.72) <0.001 ALT <40 U/L Ref ≥40 U/L 1.90(1.15~3.14) 0.013 AST <50 U/L Ref ≥50 2.93(1.57~5.48) 0.001 HBsAg <1 000 IU/L Ref 1 000~10 000 IU/L 0.80(0.40~1.62) 0.541 >10 000 IU/L 0.98(0.51~1.91) 0.967 HBeAg 阴性 Ref 阳性 1.00(0.41~2.51) 0.986 -
[1] TRÉPO C, CHAN HL, LOK A. Hepatitis B virus infection[J]. Lancet, 2014, 384( 9959): 2053- 2063. DOI: 10.1016/s0140-6736(14)60220-8. [2] Global Burden of Disease Liver Cancer Collaboration; AKINYEMIJU T, ABERA S, et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: Results from the global burden of disease study 2015[J]. JAMA Oncol, 2017, 3( 12): 1683- 1691. DOI: 10.1001/jamaoncol.2017.3055. [3] CHEN BY, XU HT, DING XY, et al. Serum B7-H2 and interleukin-6 levels in patients with hepatitis B virus-related primary liver cancer and their correlation with prognosis[J]. Trauma Crit Care Med, 2022, 10( 4): 292- 295, 299. DOI: 10.16048/j.issn.2095-5561.2022.04.13.陈冰燕, 徐绘婷, 丁翔宇, 等. 乙型肝炎病毒相关原发性肝癌患者血清B7-H2、白细胞介素6水平及其与预后相关性研究[J]. 创伤与急危重病医学, 2022, 10( 4): 292- 295, 299. DOI: 10.16048/j.issn.2095-5561.2022.04.13. [4] ASRANI SK, DEVARBHAVI H, EATON J, et al. Burden of liver diseases in the world[J]. J Hepatol, 2019, 70( 1): 151- 171. DOI: 10.1016/j.jhep.2018.09.014. [5] SCHWEITZER A, HORN J, MIKOLAJCZYK RT, et al. Estimations of worldwide prevalence of chronic hepatitis B virus infection: A systematic review of data published between 1965 and 2013[J]. Lancet, 2015, 386( 10003): 1546- 1555. DOI: 10.1016/S0140-6736(15)61412-X. [6] LIU ZQ, MAO XH, JIANG YF, et al. Changing trends in the disease burden of primary liver cancer caused by specific etiologies in China[J]. Cancer Med, 2019, 8( 12): 5787- 5799. DOI: 10.1002/cam4.2477. [7] YUEN MF, TANAKA Y, FONG DY, et al. Independent risk factors and predictive score for the development of hepatocellular carcinoma in chronic hepatitis B[J]. J Hepatol, 2009, 50( 1): 80- 88. DOI: 10.1016/j.jhep.2008.07.023. [8] SHERMAN M. Hepatocellular carcinoma: Epidemiology, risk factors, and screening[J]. Semin Liver Dis, 2005, 25( 2): 143- 154. DOI: 10.1055/s-2005-871194. [9] CHEN CJ, YANG HI, SU J, et al. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level[J]. JAMA, 2006, 295( 1): 65- 73. DOI: 10.1001/jama.295.1.65. [10] HE J, CHEN WQ, SHEN HB, et al. China guideline for liver cancer screening(2022, Beijing)[J]. J Clin Hepatol, 2022, 38( 8): 1739- 1758. DOI: 10.3969/j.issn.1001-5256.2022.08.007.赫捷, 陈万青, 沈洪兵, 等. 中国人群肝癌筛查指南(2022, 北京)[J]. 临床肝胆病杂志, 2022, 38( 8): 1739- 1758. DOI: 10.3969/j.issn.1001-5256.2022.08.007. [11] LIANG F, SHA CX, FAN CS, et al. Qidong Chronic Hepatitis B Cohort: Participants enrollment and comparison of baseline characteristics by gender stratification[J]. Chin J Epidemiol, 2017, 38( 11): 1569- 1573. DOI: 10.3760/cma.j.issn.0254-6450.2017.11.026.梁枫, 沙春霞, 樊春笋, 等. 启东慢性乙型肝炎临床队列: 建立及基线特征[J]. 中华流行病学杂志, 2017, 38( 11): 1569- 1573. DOI: 10.3760/cma.j.issn.0254-6450.2017.11.026. [12] KIM BK, AHN SH. Prediction model of hepatitis B virus-related hepatocellular carcinoma in patients receiving antiviral therapy[J]. J Formos Med Assoc, 2023, 122( 12): 1238- 1246. DOI: 10.1016/j.jfma.2023.05.029. [13] LEE HW, AHN SH. Prediction models of hepatocellular carcinoma development in chronic hepatitis B patients[J]. World J Gastroenterol, 2016, 22( 37): 8314- 8321. DOI: 10.3748/wjg.v22.i37.8314. [14] RAFFETTI E, FATTOVICH G, DONATO F. Incidence of hepatocellular carcinoma in untreated subjects with chronic hepatitis B: A systematic review and meta-analysis[J]. Liver Int, 2016, 36( 9): 1239- 1251. DOI: 10.1111/liv.13142. [15] WANG Y, WANG M, LI H, et al. A male-ABCD algorithm for hepatocellular carcinoma risk prediction in HBsAg carriers[J]. Chin J Cancer Res, 2021, 33( 3): 352- 363. DOI: 10.21147/j.issn.1000-9604.2021.03.07. [16] YANG HI, YUEN MF, CHAN HL, et al. Risk estimation for hepatocellular carcinoma in chronic hepatitis B(REACH-B): Development and validation of a predictive score[J]. Lancet Oncol, 2011, 12( 6): 568- 574. DOI: 10.1016/S1470-2045(11)70077-8. [17] FAN R, PAPATHEODORIDIS G, SUN J, et al. aMAP risk score predicts hepatocellular carcinoma development in patients with chronic hepatitis[J]. J Hepatol, 2020, 73( 6): 1368- 1378. DOI: 10.1016/j.jhep.2020.07.025. [18] YU JH, SUH YJ, JIN YJ, et al. Prediction model for hepatocellular carcinoma risk in treatment-naive chronic hepatitis B patients receiving entecavir/tenofovir[J]. Eur J Gastroenterol Hepatol, 2019, 31( 7): 865- 872. DOI: 10.1097/MEG.0000000000001357. [19] KIM JH, KIM YD, LEE M, et al. Modified PAGE-B score predicts the risk of hepatocellular carcinoma in Asians with chronic hepatitis B on antiviral therapy[J]. J Hepatol, 2018, 69( 5): 1066- 1073. DOI: 10.1016/j.jhep.2018.07.018. [20] YANG HI, SHERMAN M, SU J, et al. Nomograms for risk of hepatocellular carcinoma in patients with chronic hepatitis B virus infection[J]. J Clin Oncol, 2010, 28( 14): 2437- 2444. DOI: 10.1200/JCO.2009.27.4456. [21] WONG VW, CHAN SL, MO F, et al. Clinical scoring system to predict hepatocellular carcinoma in chronic hepatitis B carriers[J]. J Clin Oncol, 2010, 28( 10): 1660- 1665. DOI: 10.1200/JCO.2009.26.2675. [22] LIAW YF, SUNG JJY, CHOW WC, et al. Lamivudine for patients with chronic hepatitis B and advanced liver disease[J]. N Engl J Med, 2004, 351( 15): 1521- 1531. DOI: 10.1056/NEJMoa033364. [23] LIM YS, HAN S, HEO NY, et al. Mortality, liver transplantation, and hepatocellular carcinoma among patients with chronic hepatitis B treated with entecavir vs lamivudine[J]. Gastroenterology, 2014, 147( 1): 152- 161. DOI: 10.1053/j.gastro.2014.02.033. -



 PDF下载 ( 1065 KB)
PDF下载 ( 1065 KB)

 下载:
下载: