肝静脉剥夺术与门静脉栓塞治疗剩余肝体积不足肝癌效果比较的Meta分析
DOI: 10.12449/JCH241217
Clinical efficacy of liver venous deprivation versus portal vein embolization in treatment of liver cancer with insufficient residual liver volume: A Meta-analysis
-
摘要:
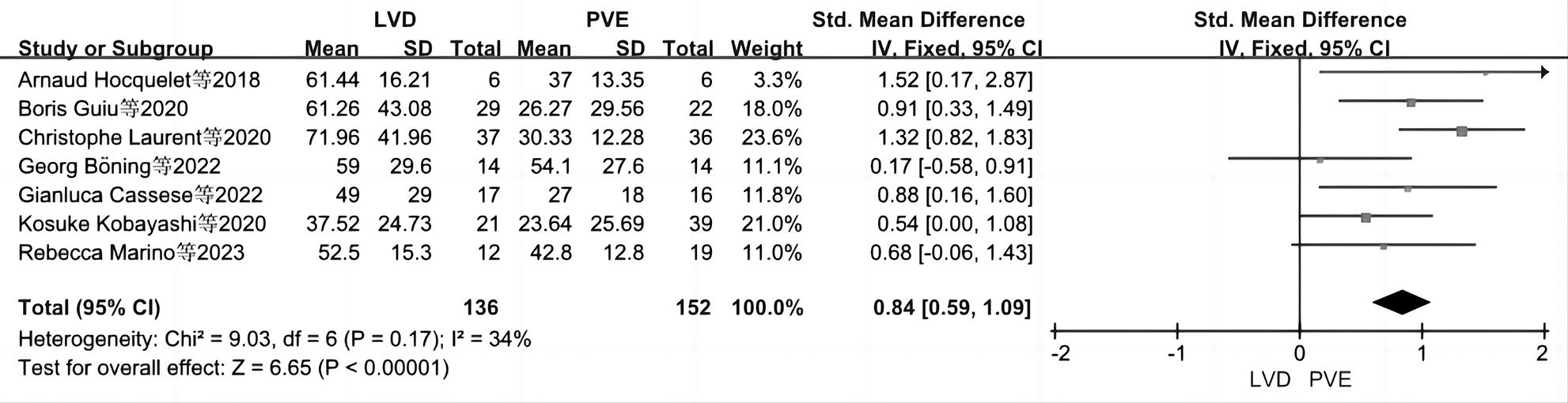
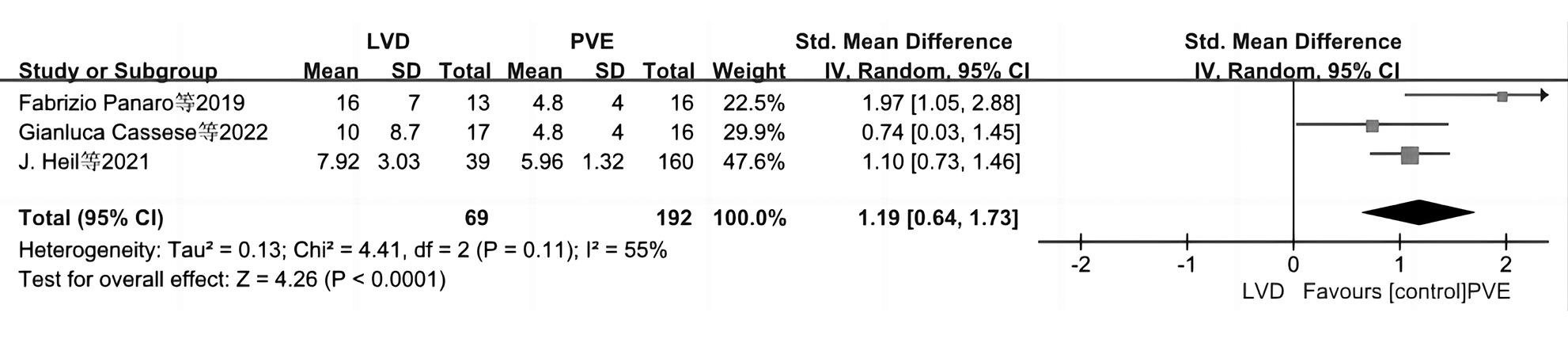
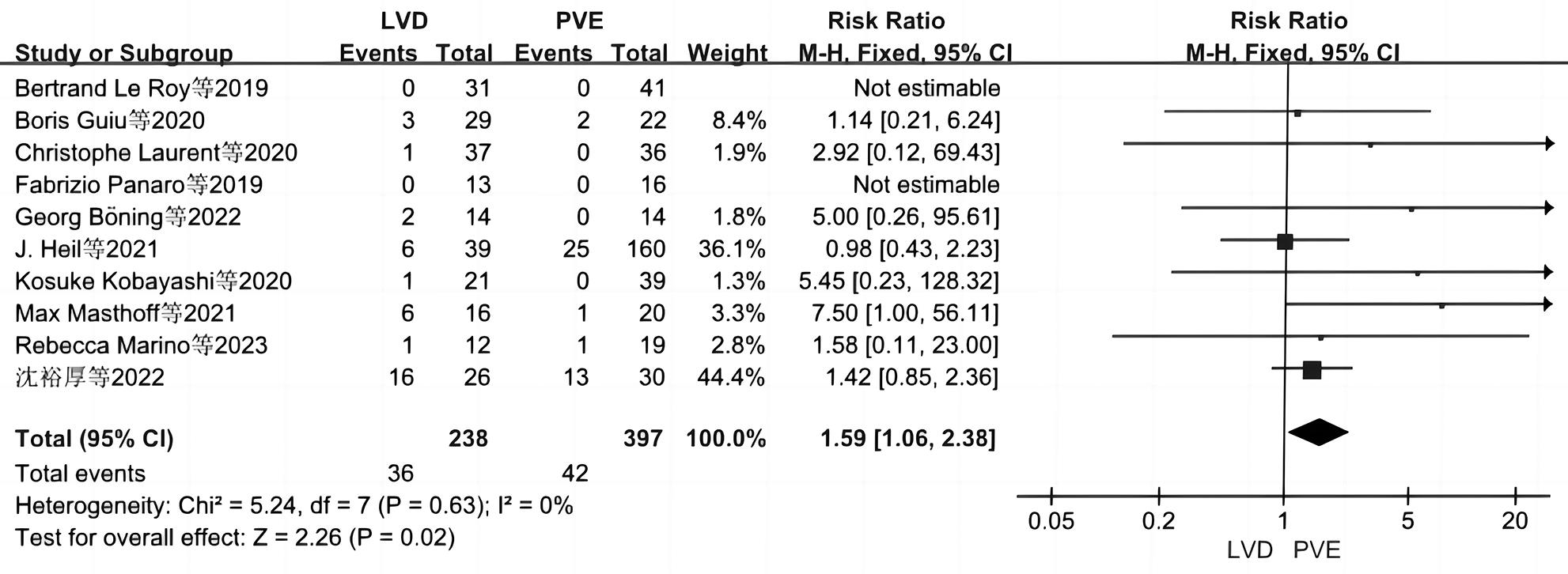
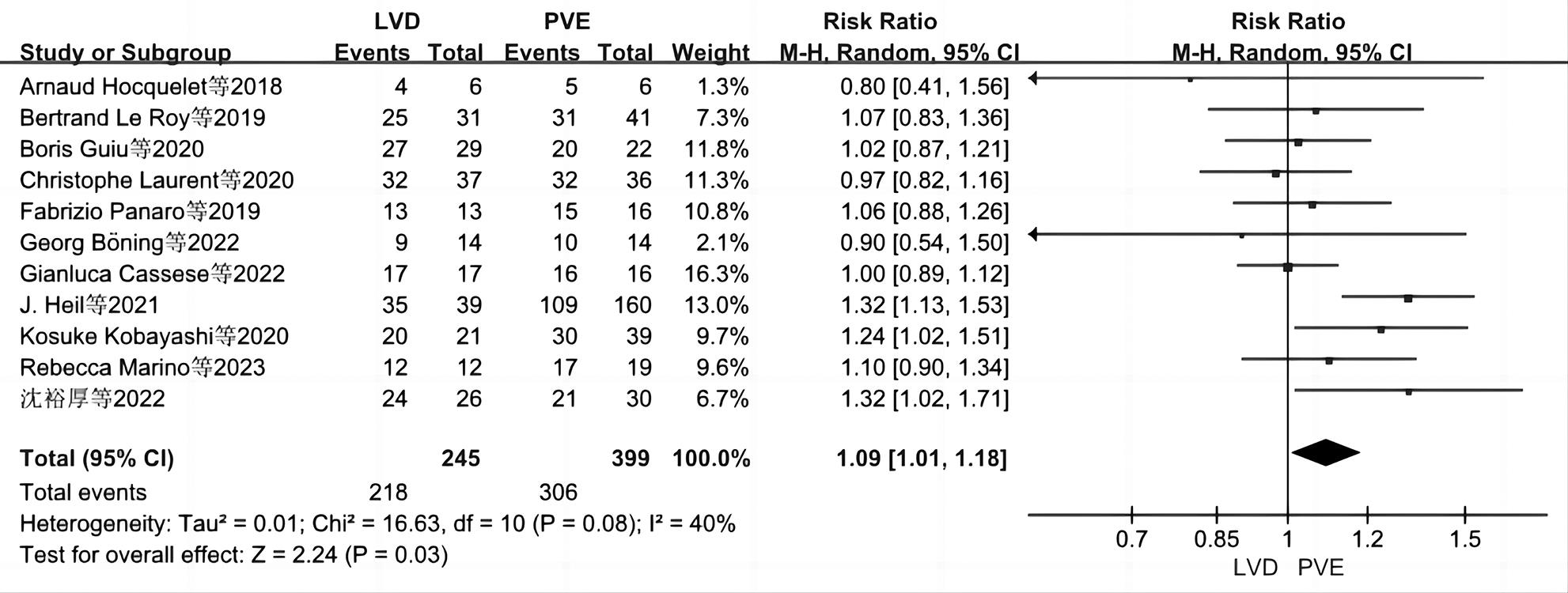
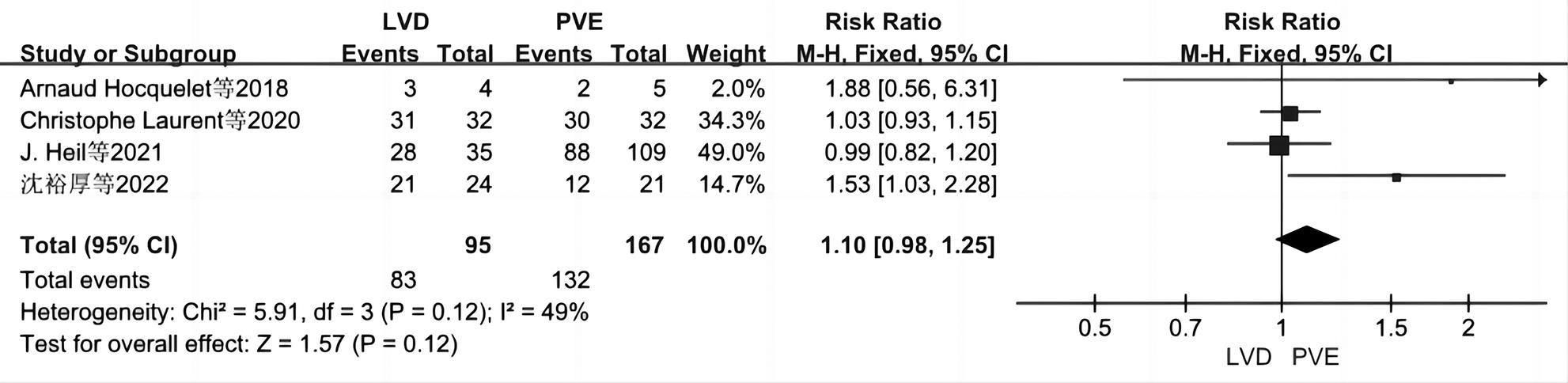
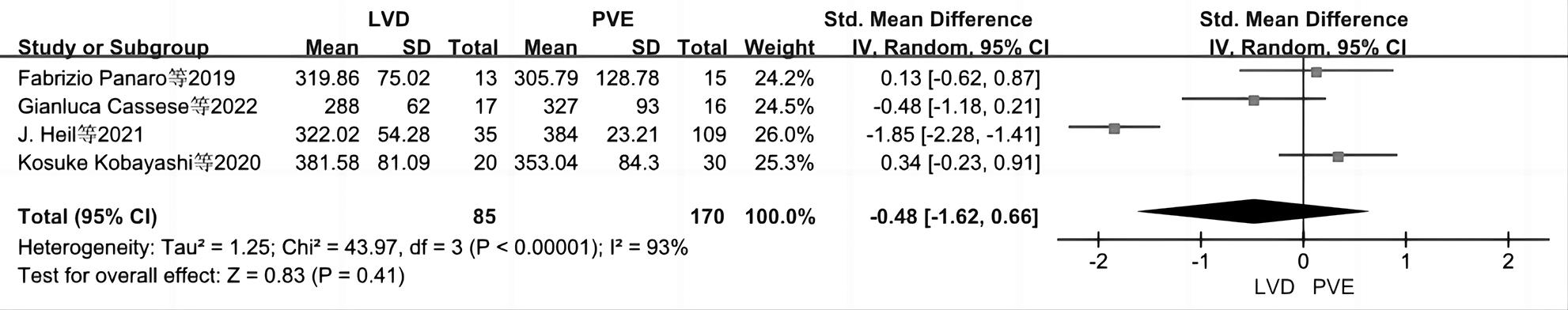
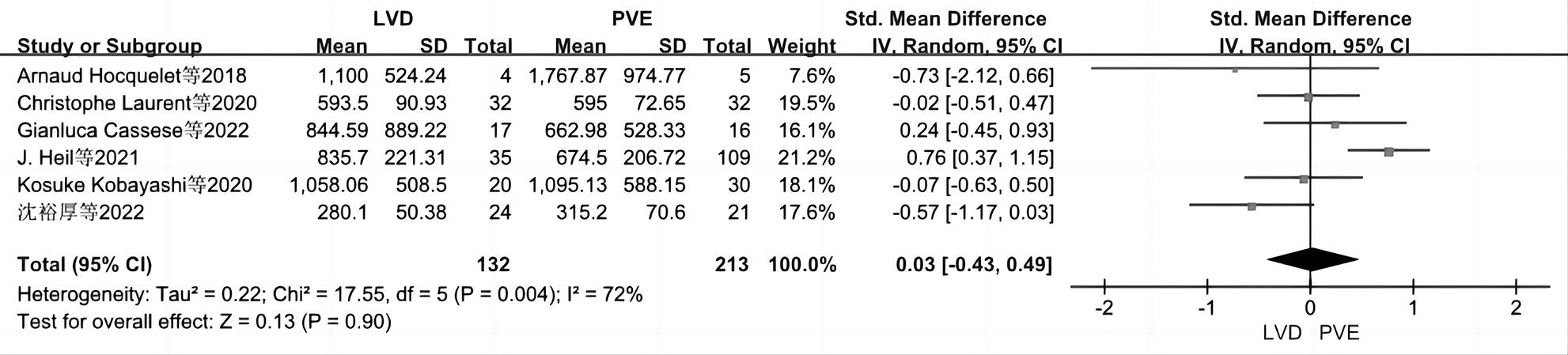
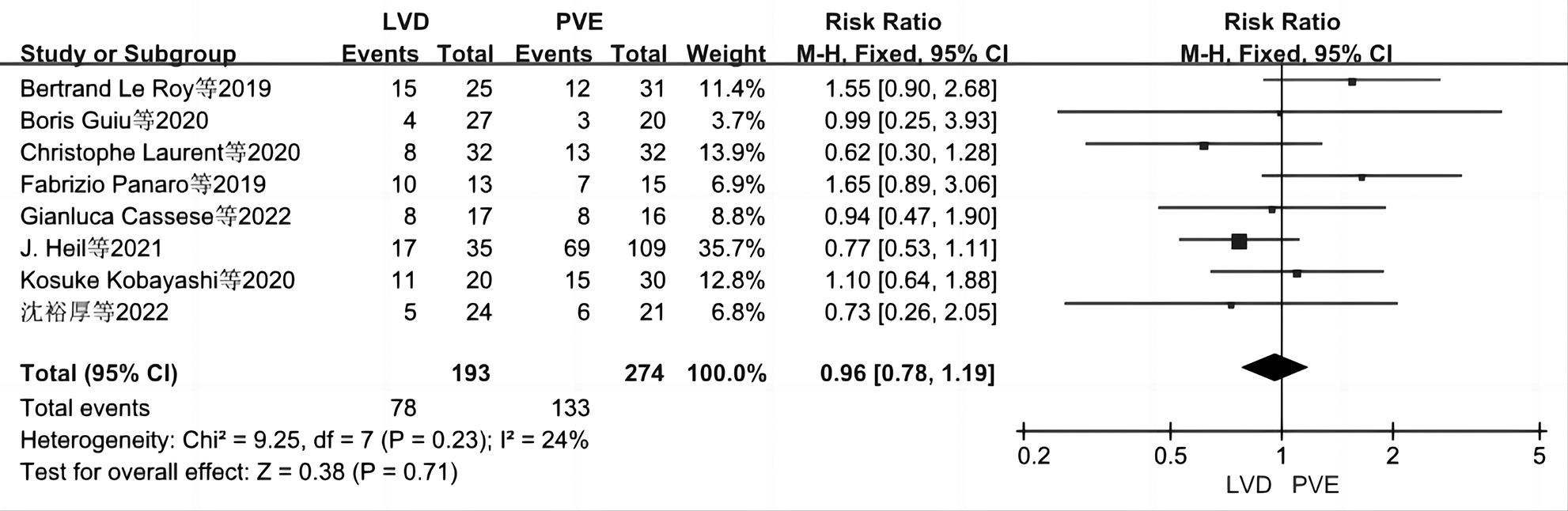
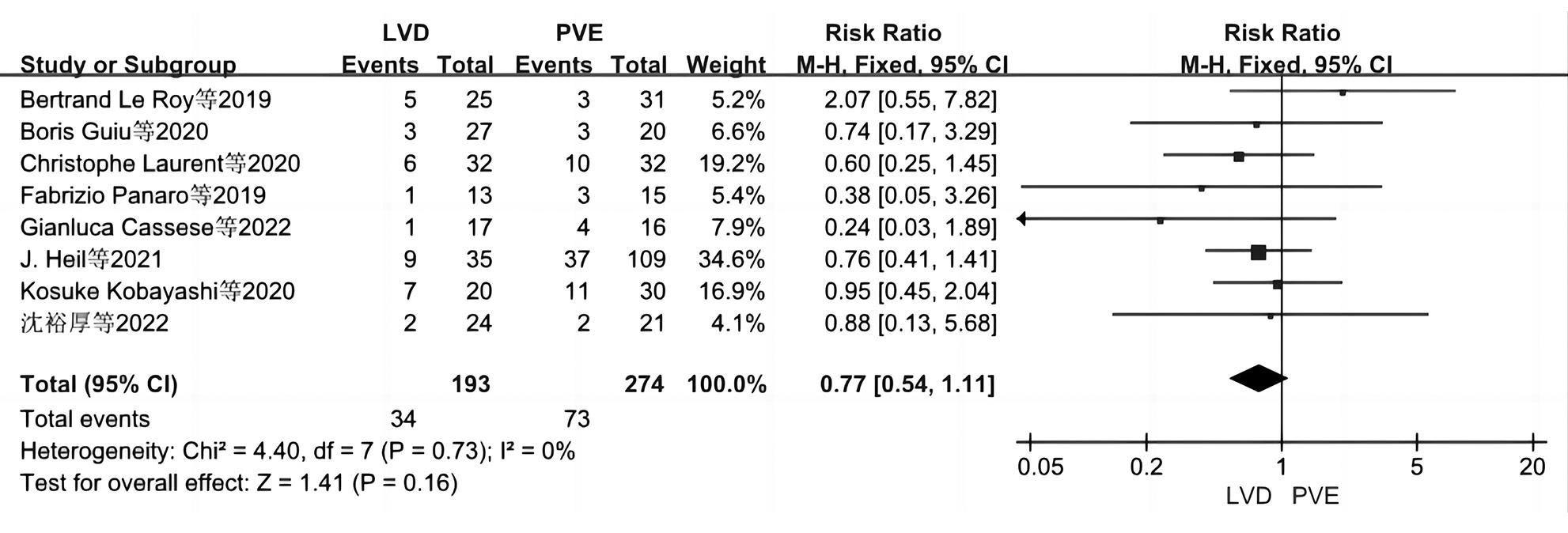
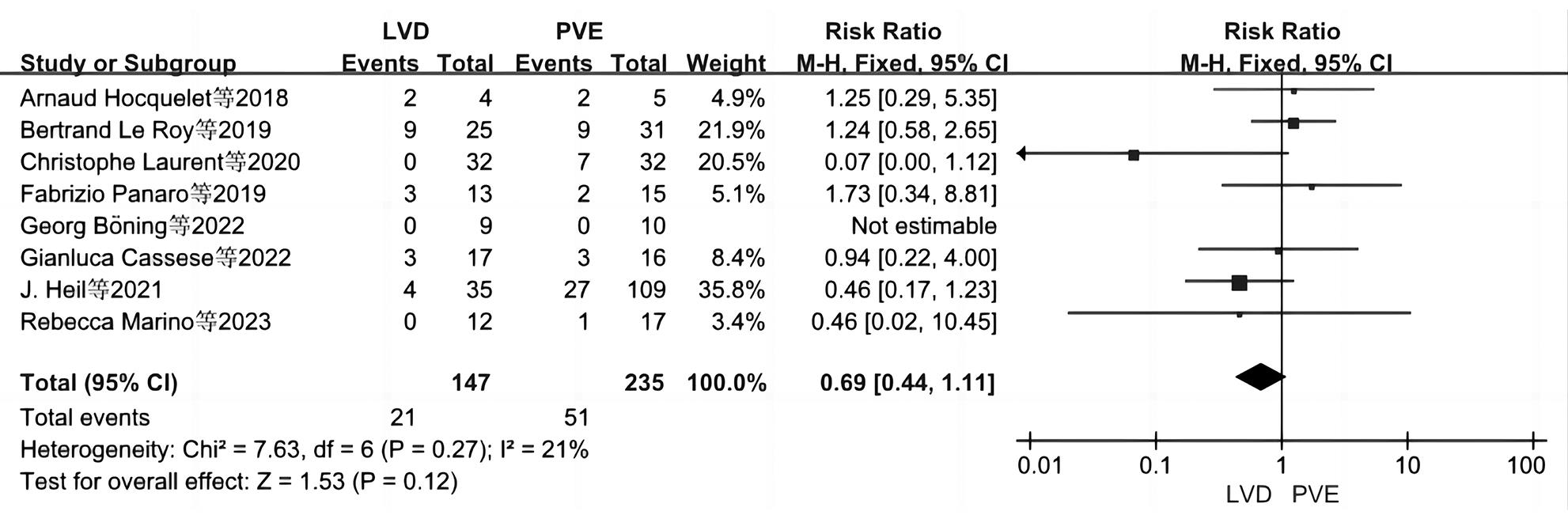
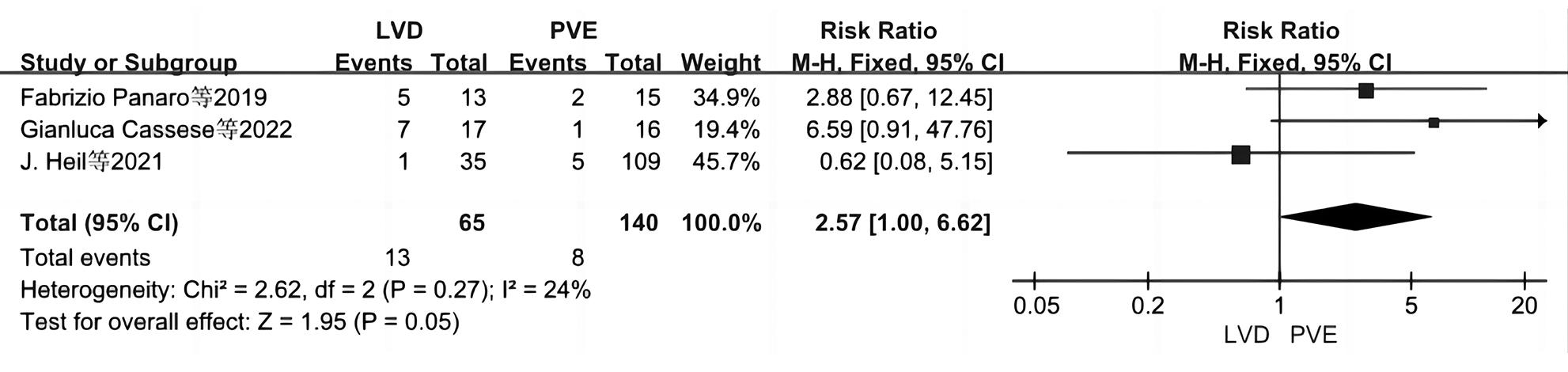
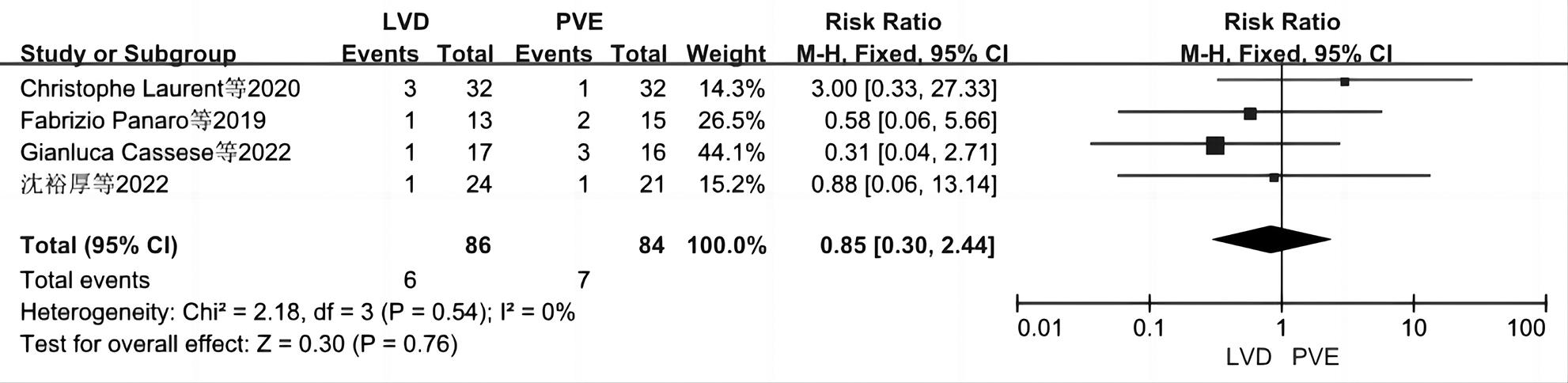
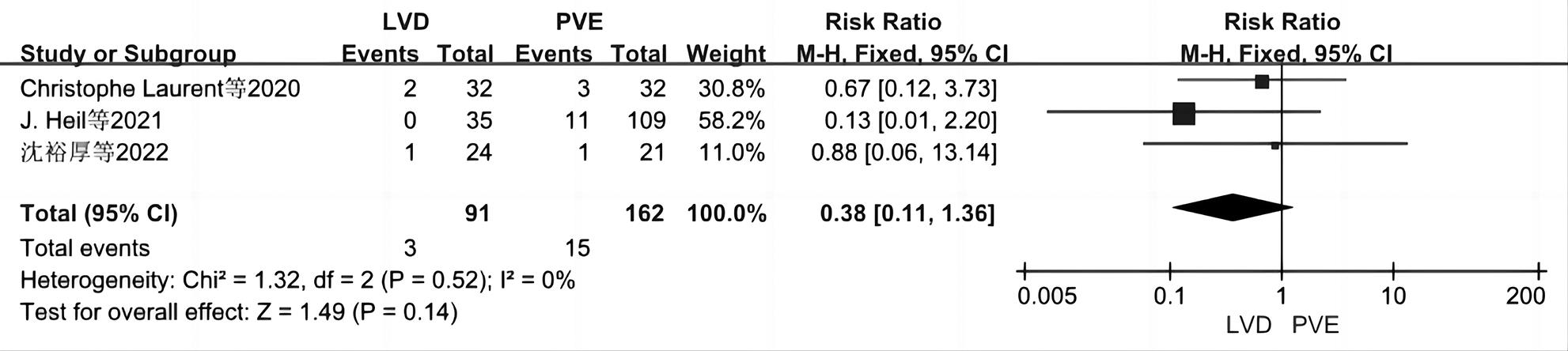
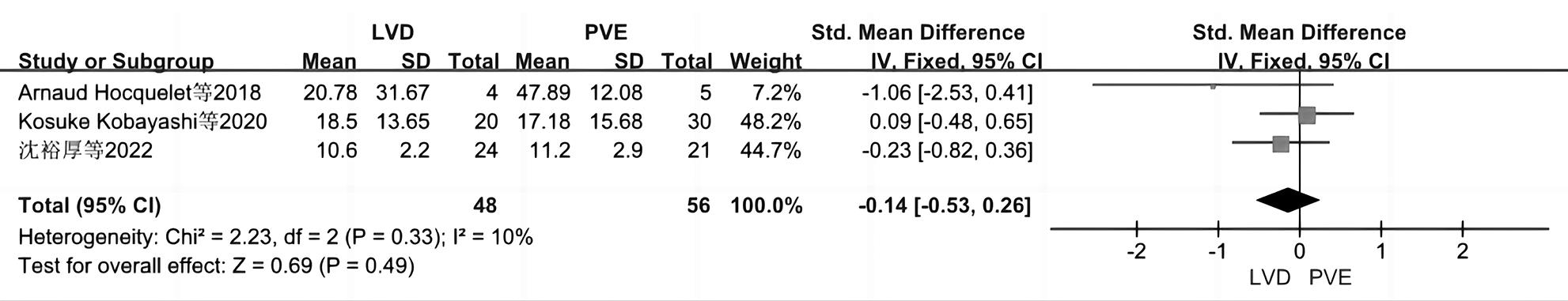
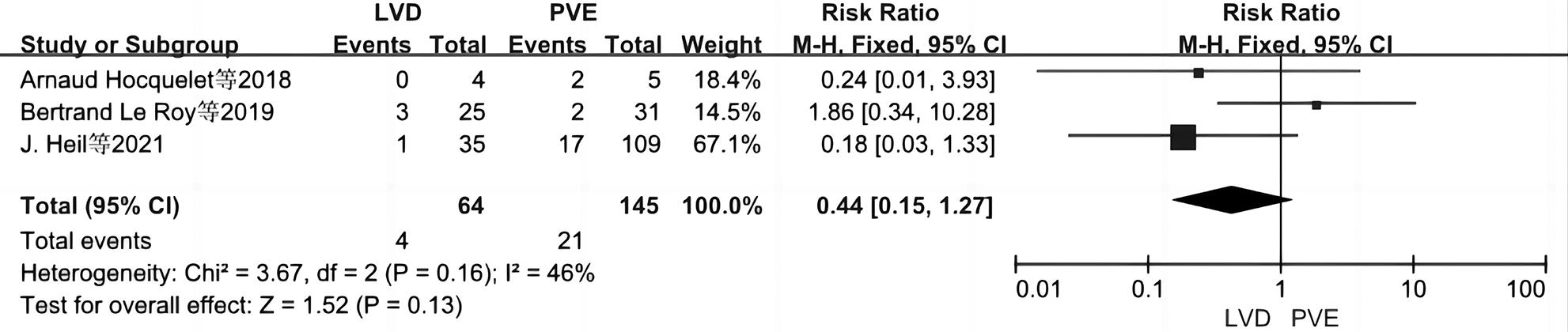
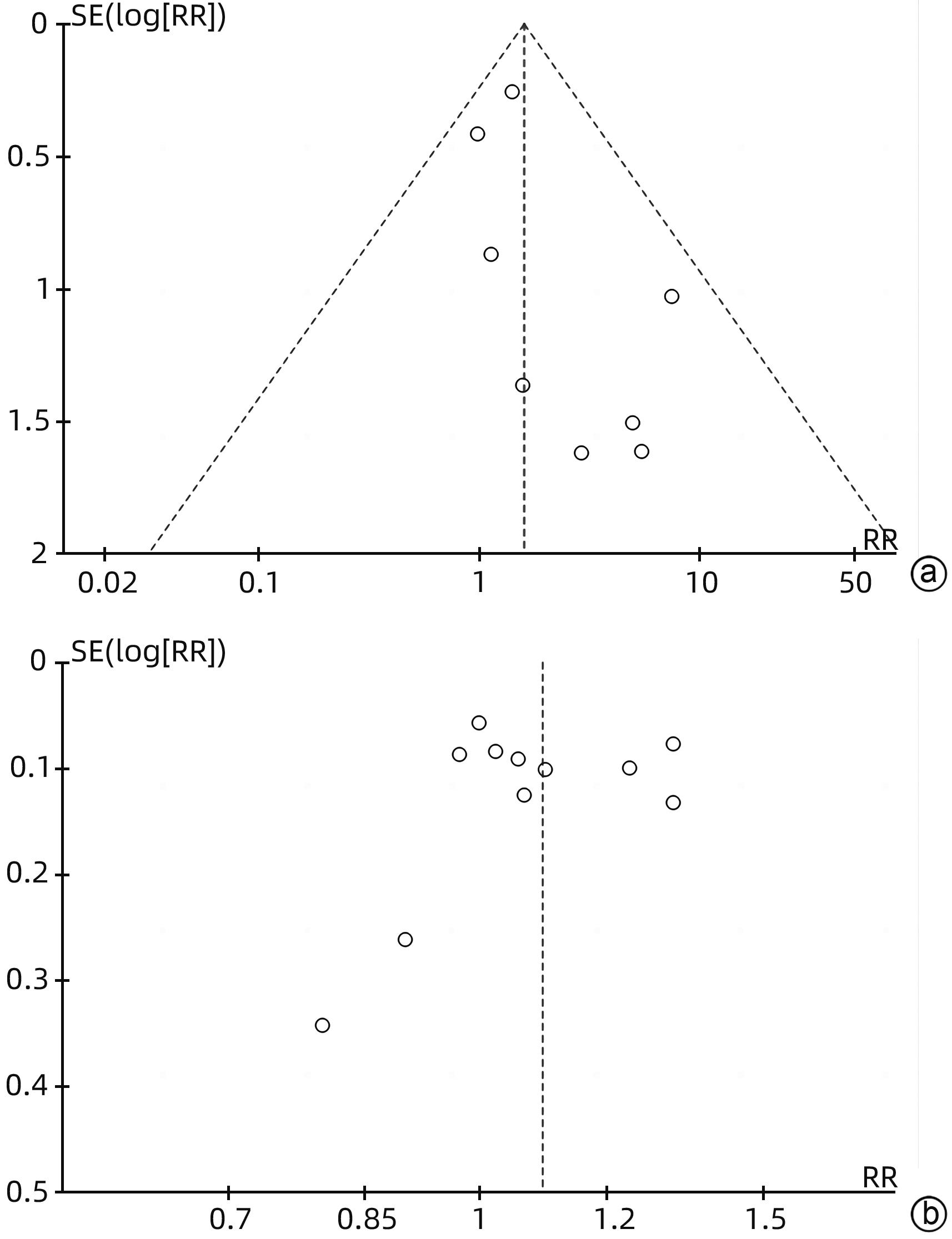
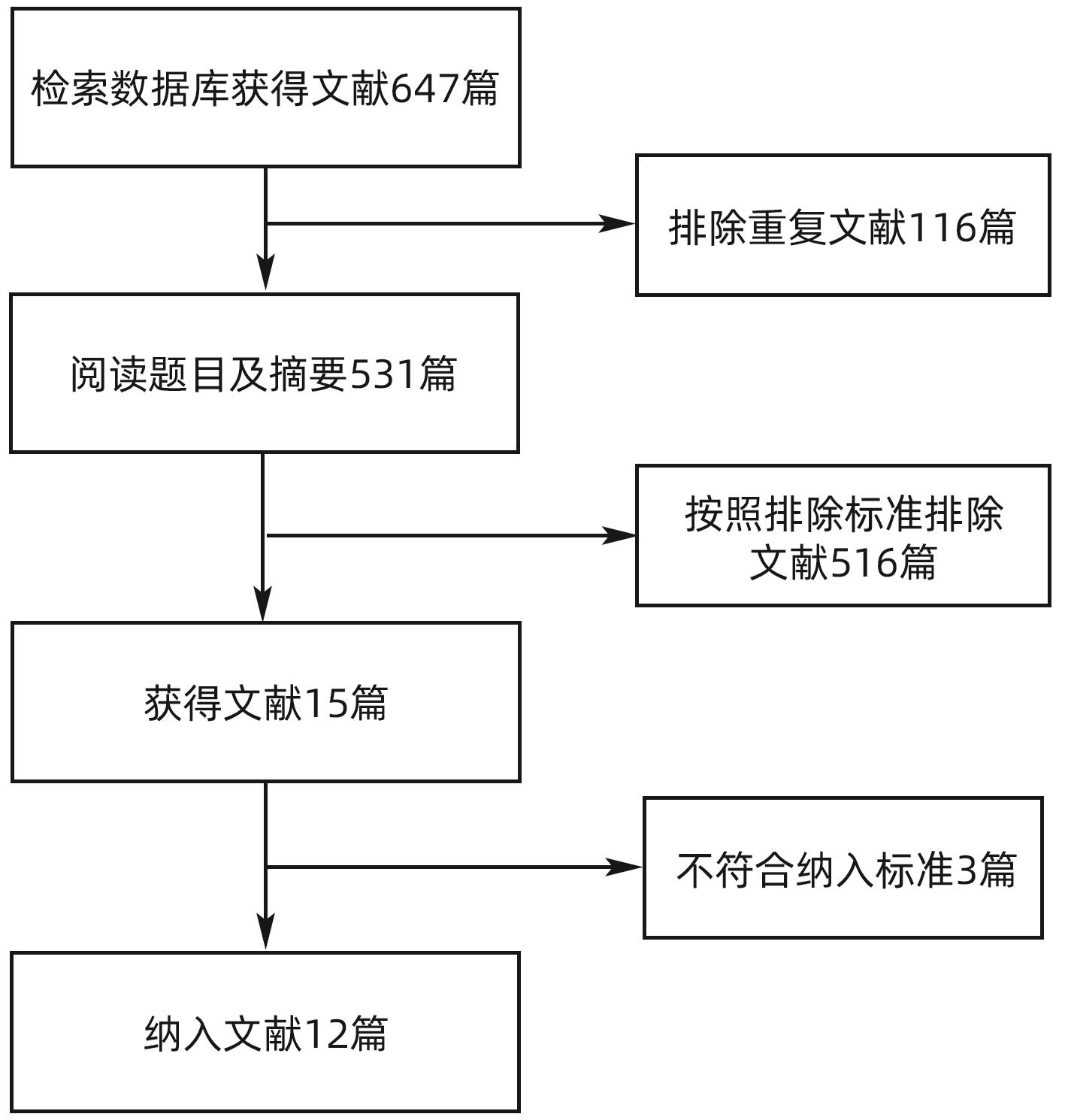
目的 系统性评价肝静脉剥夺术(LVD)与门静脉栓塞(PVE)治疗剩余肝体积(FLR)不足的肝脏恶性肿瘤的效果及预后。 方法 本研究根据PRISMA指南完成,PROSPERO注册号:CRD42024533292。检索PubMed、Embase、Cochrane Library、Web of Science、知网、万方、维普等数据库中关于LVD与PVE效果比较的所有文献。根据制定的纳入和排除文献标准,筛选相关文献,评估文献质量,提取相关LVD与PVE的临床对比资料,整理并分析数据。使用RevMan 5.3软件进行Meta分析。 结果 共纳入12篇文献(均为队列研究),含644例患者(LVD组245例,PVE组399例)。Meta分析结果显示,在栓塞后FLR增长率(SMD=0.84,95%CI:0.59~1.09)、栓塞后FLR每日增长体积(SMD=1.19,95%CI:0.64~1.73)、栓塞后并发症发病率(RR=1.59,95%CI:1.06~2.38)、栓塞与二期手术间隔时间(SMD=-0.81,95%CI:-1.32~-0.29)和二期手术完成率(RR=1.09,95%CI:1.01~1.18)两组间差异均有统计学意义(P值均<0.05)。 结论 LVD相较于PVE能够使患者在相对较短的时间内获得达到手术指征的FLR,从而降低疾病进展的发生率以及解决肥大不足的问题,达到更高的二期手术切除率,从而使更多的肝癌患者受益。并且,LVD在二期手术中具有和PVE相似的安全性。 Abstract:Objective To systematically evaluate the efficacy and prognosis of liver venous deprivation (LVD) versus portal vein embolization (PVE) in the treatment of hepatic malignancies with insufficient residual liver volume. Methods This study was conducted according to PRISMA guidelines, with a PROSPERO registration number of CRD42024533292. Databases including PubMed, Embase, the Cochrane Library, Web of Science, CNKI, Wanfang Data, and VIP were searched for articles on the efficacy of LVD versus PVE. According to the inclusion and exclusion criteria, related articles were screened for quality assessment and extraction of clinical data for LVD and PVE, and related data were summarized and analyzed. RevMan 5.3 was used to perform the Meta-analysis. Results A total of 12 articles (all cohort studies) were included, involving 644 patients (245 in the LVD group and 399 in the PVE group). The Meta-analysis showed that there were significant differences between the two groups in FLR growth rate after embolization (standardized mean difference [SMD]=0.84, 95% confidence interval [CI]: 0.59 — 1.09, P<0.05), daily growth volume of FLR after embolization (SMD=1.19, 95%CI: 0.64 — 1.73, P<0.05), the incidence rate of complications after embolization (risk ratio [RR]=1.59, 95%CI: 1.06 — 2.38, P<0.05), interval between embolization and second-stage surgery (SMD=-0.81, 95%CI: -1.32 to -0.29, P<0.05), and the completion rate of second-stage surgery (RR=1.09, 95%CI: 1.01 — 1.18, P<0.05). Conclusion Compared with PVE, LVD can enable patients to achieve FLR for surgery in a relatively short period of time, thereby reducing the incidence rate of disease progression, solving the problem of hypertrophic deficiency, achieving a higher second-stage surgical resection rate, and bringing more benefits to patients with liver cancer. In addition, LVD has similar safety profiles to PVE during second-stage surgery. -
Key words:
- Liver Neoplasms /
- Liver Vein Deprivation /
- Portal Vein Embolism /
- Meta-Analysis
-
表 1 纳入文献基本特征
Table 1. Basic features of the included literature
作者 研究类型 发表年份 研究起止 国家 研究方式 Masthoff等[11] 回顾性分析 2021 2018—2020 德国 多中心 Laurent等[12] 回顾性分析 2020 2016.1—2018.12 法国 单中心 Heil等[13] 前瞻性非随机试验 2021 2016.1—2019.12 德国/比利时/西班牙/加拿大/荷兰/瑞士 多中心 Panaro等[14] 回顾性分析 2019 2015.4—2017.12 法国 单中心 Böning等[15] 前瞻性非随机试验 2022 2018.6—2019.8 德国 单中心 Hocquelet等[16] 回顾性研究 2018 2014—2018 瑞士/法国 多中心 Cassese等[17] 回顾性研究 2023 2015.5—2019.12 法国 单中心 Kobayashi等[18] 前瞻性非随机试验 2020 2010—2016 瑞士 单中心 Roy等[19] 前瞻性非随机试验 2020 2010.1—2017.12 法国 单中心 Guiu等[20] 回顾性分析 2020 2017.1—2019.3 法国 单中心 Marino等[21] 回顾性分析 2023 2013.1—2022.7 意大利 单中心 沈裕厚等[22] 回顾性分析 2022 2018.1—2019.1 中国 单中心 表 2 人口学资料和观察指标
Table 2. Demographic data and observational indicators
作者 样本量(例) 性别(例) 年龄(岁) 肝脏体积测量时间(天) 观察指标 LVD PVE 男 女 LVD PVE LVD PVE Masthoff等[11] 16 20 21 15 66(38~82) 64(22~74) 20±6.7/79±511) ③ Laurent等[12] 37 36 51 22 64.41(61~71) 60.92(51~72) 30.65±1.64 30.50±1.96 ①③④⑤⑥⑧⑨⑩⑪⑬⑭ Heil等[13] 39 160 120 79 63(52~67) 67(58~73) 17(13~32) 24(19~37) ②③④⑤⑥⑦⑧⑨⑩⑪⑫⑭⑯ Panaro等[14] 13 16 302) ②③⑤⑦⑨⑩⑪⑫⑬ Böning等[15] 14 14 10 18 68.1±10.5 65.1±11.4 30.57±6.86 30.50±7.17 ①③④⑤⑪ Hocquelet等[16] 6 6 60(54~71) 62(54~68) 23.5(15~29)3) ①⑤⑥⑧⑪⑮⑯ Cassese等[17] 17 16 20 13 58.9±9.6 65.2±9.5 ①②④⑤⑦⑧⑨⑩⑪⑫⑬⑰ Kobayashi等[18] 20 30 31 19 65(25~85) 65(41~75) 23.08±10.38 26.35±10.12 ①③④⑤⑦⑧⑨⑩⑮ Roy等[19] 31 41 44 28 66(55~70) 63(60~68) 26 27 ③⑤⑨⑩⑪⑯ Guiu等[20] 29 22 37 14 62(26~79) 66(45~79) 7/14/214) ①③④⑤⑨⑩ Marino等[21] 12 19 17 14 68.61±8.06 66.53±8.22 12.4±4/25.3±45) ①③④⑤⑪ 沈裕厚等[22] 26 30 36 20 52.6±5.7 51.3±4.2 7/14/214) ③④⑤⑥⑧⑨⑩⑬⑭⑮⑰ 注:1)该论文分别对2组患者肝脏体积测量了2次,第1次肝脏体积测量时间为(20±6.7)天,第2次为(79±51)天,未将2组患者肝脏体积测量时间分开描述。2)该论文中2组患者均在操作后1个月时进行肝脏体积测量。3)该论文中未将2组患者肝脏体积测量时间分别进行描述,所有患者肝脏体积测量时间距LVD或PVE间隔为23.5(15~29)天。4)该论文中所有患者在基线(肝脏准备前)以及PVE或LVD后第7、14和21天进行肝脏体积测量。5)该论文中分别对2组患者肝脏体积测量了2次,第1次肝脏体积测量时间为(12.4±4)天,第2次为(25.3±4)天,未将2组患者肝脏体积测量时间分开描述。①栓塞后FLR增长率;②栓塞后FLR每日增长体积;③栓塞后并发症发病率;④栓塞与二期手术间隔时间;⑤二期手术完成率;⑥R0切除率;⑦二期手术时长;⑧二期手术中失血量;⑨术后并发症发生率;⑩术后并发症Clavien-Dindo≥Ⅲ级;⑪术后肝衰竭发生率;⑫术后出血;⑬术后胆漏;⑭术后腹腔感染;⑮术后住院时间;⑯90天死亡率;⑰术后肝癌复发。
表 3 文献质量评价结果
Table 3. Results of literature quality evaluation
文献 选择 可比性 结果 得分 暴露组代表性 非暴露组代表性 暴露因素确定 开始前无要观察结局指标 最重要因素 其他因素 结局指标评价 随访时间(≥1个月) 完整性 Masthoff等[11] √ √ √ √ √ √ √ 7 Laurent等[12] √ √ √ √ √ √ √ √ √ 9 Heil等[13] √ √ √ √ √ √ √ √ √ 9 Panaro等[14] √ √ √ √ √ √ √ 7 Böning等[15] √ √ √ √ √ √ √ √ 8 Hocquelet等[16] √ √ √ √ √ √ √ √ √ 9 Cassese等[17] √ √ √ √ √ √ √ √ √ 9 Kobayashi等[18] √ √ √ √ √ √ √ √ 8 Roy等[19] √ √ √ √ √ √ √ 7 Guiu等[20] √ √ √ √ √ √ √ 7 Marino等[21] √ √ √ √ √ √ √ √ 8 沈裕厚等[22] √ √ √ √ √ √ √ √ √ 9 -
[1] ADAMS RB, ALOIA TA, LOYER E, et al. Selection for hepatic resection of colorectal liver metastases: Expert consensus statement[J]. HPB, 2013, 15( 2): 91- 103. DOI: 10.1111/j.1477-2574.2012.00557.x. [2] KINOSHITA H, SAKAI K, HIROHASHI K, et al. Preoperative portal vein embolization for hepatocellular carcinoma[J]. World J Surg, 1986, 10( 5): 803- 808. DOI: 10.1007/BF01655244. [3] AOKI T, KUBOTA K. Preoperative portal vein embolization for hepatocellular carcinoma: Consensus and controversy[J]. World J Hepatol, 2016, 8( 9): 439- 445. DOI: 10.4254/wjh.v8.i9.439. [4] SHINDOH J, TRUTY MJ, ALOIA TA, et al. Kinetic growth rate after portal vein embolization predicts posthepatectomy outcomes: Toward zero liver-related mortality in patients with colorectal liver metastases and small future liver remnant[J]. J Am Coll Surg, 2013, 216( 2): 201- 209. DOI: 10.1016/j.jamcollsurg.2012.10.018. [5] NARITA M, OUSSOULTZOGLOU E, IKAI I, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings[J]. Ann Surg, 2012, 256( 3): e7- e8; authorreplye16- 7. DOI: 10.1097/SLA.0b013e318265fd51. [6] SCHADDE E, RAPTIS DA, SCHNITZBAUER AA, et al. Prediction of mortality after ALPPS stage-1: An analysis of 320 patients from the international ALPPS registry[J]. Ann Surg, 2015, 262( 5): 780-785; discussion 785-786. DOI: 10.1097/SLA.0000000000001450. [7] GUIU B, CHEVALLIER P, DENYS A, et al. Simultaneous trans-hepatic portal and hepatic vein embolization before major hepatectomy: The liver venous deprivation technique[J]. Eur Radiol, 2016, 26( 12): 4259- 4267. DOI: 10.1007/s00330-016-4291-9. [8] LUO DH, WAN X, LIU JM, et al. How to estimate the sample mean and standard deviation from the sample size, median, extremes or quartiles?[J]. Chin J Evid Based Med, 2017, 17( 11): 1350- 1356. DOI: 10.7507/1672-2531.201706060.罗德惠, 万翔, 刘际明, 等. 如何实现从样本量、中位数、极值或四分位数到均数与标准差的转换[J]. 中国循证医学杂志, 2017, 17( 11): 1350- 1356. DOI: 10.7507/1672-2531.201706060. [9] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25( 9): 603- 605. DOI: 10.1007/s10654-010-9491-z. [10] HIGGINS JPT, ALTMAN DG, GØTZSCHE PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials[J]. BMJ, 2011, 343: d5928. DOI: 10.1136/bmj.d5928. [11] MASTHOFF M, KATOU SD, KÖHLER M, et al. Portal and hepatic vein embolization prior to major hepatectomy[J]. Z Gastroenterol, 2021, 59( 1): 35- 42. DOI: 10.1055/a-1330-9450. [12] LAURENT C, FERNANDEZ B, MARICHEZ A, et al. Radiological simultaneous portohepatic vein embolization(RASPE) before major hepatectomy: A better way to optimize liver hypertrophy compared to portal vein embolization[J]. Ann Surg, 2020, 272( 2): 199- 205. DOI: 10.1097/SLA.0000000000003905. [13] HEIL J, KORENBLIK R, HEID F, et al. Preoperative portal vein or portal and hepatic vein embolization: DRAGON collaborative group analysis[J]. Br J Surg, 2021, 108( 7): 834- 842. DOI: 10.1093/bjs/znaa149. [14] PANARO F, GIANNONE F, RIVIERE B, et al. Perioperative impact of liver venous deprivation compared with portal venous embolization in patients undergoing right hepatectomy: Preliminary results from the pioneer center[J]. Hepatobiliary Surg Nutr, 2019, 8( 4): 329- 337. DOI: 10.21037/hbsn.2019.07.06. [15] BÖNING G, FEHRENBACH U, AUER TA, et al. Liver venous deprivation(LVD) versus portal vein embolization(PVE) alone prior to extended hepatectomy: A matched pair analysis[J]. Cardiovasc Intervent Radiol, 2022, 45( 7): 950- 957. DOI: 10.1007/s00270-022-03107-0. [16] HOCQUELET A, SOTIRIADIS C, DURAN R, et al. Preoperative portal vein embolization alone with biliary drainage compared to a combination of simultaneous portal vein, right hepatic vein embolization and biliary drainage in klatskin tumor[J]. Cardiovasc Intervent Radiol, 2018, 41( 12): 1885- 1891. DOI: 10.1007/s00270-018-2075-0. [17] CASSESE G, TROISI RI, KHAYAT S, et al. Liver venous deprivation versus portal vein embolization before major hepatectomy for colorectal liver metastases: A retrospective comparison of short- and medium-term outcomes[J]. J Gastrointest Surg, 2023, 27( 2): 296- 305. DOI: 10.1007/s11605-022-05551-2. [18] KOBAYASHI K, YAMAGUCHI T, DENYS A, et al. Liver venous deprivation compared to portal vein embolization to induce hypertrophy of the future liver remnant before major hepatectomy: A single center experience[J]. Surgery, 2020, 167( 6): 917- 923. DOI: 10.1016/j.surg.2019.12.006. [19] ROY BL, GALLON A, CAUCHY F, et al. Combined biembolization induces higher hypertrophy than portal vein embolization before major liver resection[J]. HPB, 2020, 22( 2): 298- 305. DOI: 10.1016/j.hpb.2019.08.005. [20] GUIU B, QUENET F, PANARO F, et al. Liver venous deprivation versus portal vein embolization before major hepatectomy: Future liver remnant volumetric and functional changes[J]. Hepatobiliary Surg Nutr, 2020, 9( 5): 564- 576. DOI: 10.21037/hbsn.2020.02.06. [21] MARINO R, RATTI F, DELLA CORTE A, et al. Comparing liver venous deprivation and portal vein embolization for perihilar cholangiocarcinoma: Is it time to shift the focus to hepatic functional reserve rather than hypertrophy?[J]. Cancers, 2023, 15( 17): 4363. DOI: 10.3390/cancers15174363. [22] SHEN YH, YUE AM, JU AD, et al. Application of liver venous deprivation in secondary hepatic resection of primary liver cancer[J]. Chin J Oncol, 2022, 44( 11): 1221- 1228. DOI: 10.3760/cma.j.cn112152-20210801-00563.沈裕厚, 岳爱民, 琚安栋, 等. 肝静脉剥脱术在原发性肝癌二期切除术中的应用价值[J]. 中华肿瘤杂志, 2022, 44( 11): 1221- 1228. DOI: 10.3760/cma.j.cn112152-20210801-00563. [23] CHOI SB, KIM KS, CHOI JY, et al. The prognosis and survival outcome of intrahepatic cholangiocarcinoma following surgical resection: Association of lymph node metastasis and lymph node dissection with survival[J]. Ann Surg Oncol, 2009, 16( 11): 3048- 3056. DOI: 10.1245/s10434-009-0631-1. [24] CAI JQ, ZHAO H, CHEN X. A new pattern of comprehensive treatment for hepatocellular carcinoma[J]. Chin J Dig Surg, 2024, 23( 2): 204- 208. DOI: 10.3760/cma.j.cn115610-20231208-00243.蔡建强, 赵宏, 陈晓. 肝癌综合治疗新格局[J]. 中华消化外科杂志, 2024, 23( 2): 204- 208. DOI: 10.3760/cma.j.cn115610-20231208-00243. [25] LIU QG, SONG T, WANG HH. Re-understanding of surgical resection techniques for liver cancer[J]. Chin J Dig Surg, 2024, 23( 1): 75- 79. DOI: 10.3760/cma.j.cn115610-20231214-00253.刘青光, 宋涛, 王欢欢. 肝癌外科手术切除技术的再认识[J]. 中华消化外科杂志, 2024, 23( 1): 75- 79. DOI: 10.3760/cma.j.cn115610-20231214-00253. [26] CASSESE G, HAN HS, FARAI AA, et al. Future remnant liver optimization: Preoperative assessment, volume augmentation procedures and management of PVE failure[J]. Minerva Surg, 2022, 77( 4): 368- 379. DOI: 10.23736/S2724-5691.22.09541-7. [27] CHEN ZX, CHEN JM, XIE QS, et al. Prevention and treatment of liver failure after hepatectomy and its research progress[J]. J Hepatobiliary Surg, 2020, 28( 3): 237- 240. DOI: 10.3969/j.issn.1006-4761.2020.03.020.陈子祥, 陈江明, 谢青松, 等. 肝切除术后肝功能衰竭的防治及研究进展[J]. 肝胆外科杂志, 2020, 28( 3): 237- 240. DOI: 10.3969/j.issn.1006-4761.2020.03.020. [28] SERENARI M, BONATTI C, ZANONI L, et al. The role of hepatobiliary scintigraphy combined with spect/ct in predicting severity of liver failure before major hepatectomy: A single-center pilot study[J]. Updates Surg, 2021, 73( 1): 197- 208. DOI: 10.1007/s13304-020-00907-2. [29] van LIENDEN KP, van den ESSCHERT JW, GRAAF WD, et al. Portal vein embolization before liver resection: A systematic review[J]. Cardiovasc Intervent Radiol, 2013, 36( 1): 25- 34. DOI: 10.1007/s00270-012-0440-y. [30] ALVAREZ FA, CASTAING D, FIGUEROA R, et al. Natural history of portal vein embolization before liver resection: A 23-year analysis of intention-to-treat results[J]. Surgery, 2018, 163( 6): 1257- 1263. DOI: 10.1016/j.surg.2017.12.027. [31] MADOFF DC, ODISIO BC, SCHADDE E, et al. Improving the safety of major resection for hepatobiliary malignancy: Portal vein embolization and recent innovations in liver regeneration strategies[J]. Curr Oncol Rep, 2020, 22( 6): 59. DOI: 10.1007/s11912-020-00922-x. [32] SCHADDE E, GUIU B, DEAL R, et al. Simultaneous hepatic and portal vein ligation induces rapid liver hypertrophy: A study in pigs[J]. Surgery, 2019, 165( 3): 525- 533. DOI: 10.1016/j.surg.2018.09.001. [33] de GRAAF W, van LIENDEN KP, van den ESSCHERT JW, et al. Increase in future remnant liver function after preoperative portal vein embolization[J]. Br J Surg, 2011, 98( 6): 825- 834. DOI: 10.1002/bjs.7456. [34] GRAAF WD, van LIENDEN KP, DINANT S, et al. Assessment of future remnant liver function using hepatobiliary scintigraphy in patients undergoing major liver resection[J]. J Gastrointest Surg, 2010, 14( 2): 369- 378. DOI: 10.1007/s11605-009-1085-2. -



 PDF下载 ( 1875 KB)
PDF下载 ( 1875 KB)

 下载:
下载: