血清甘油三酯累积暴露水平对急性胰腺炎发病风险的影响
DOI: 10.12449/JCH241220
Influence of serum cumulative triglyceride exposure on the risk of acute pancreatitis
-
摘要:
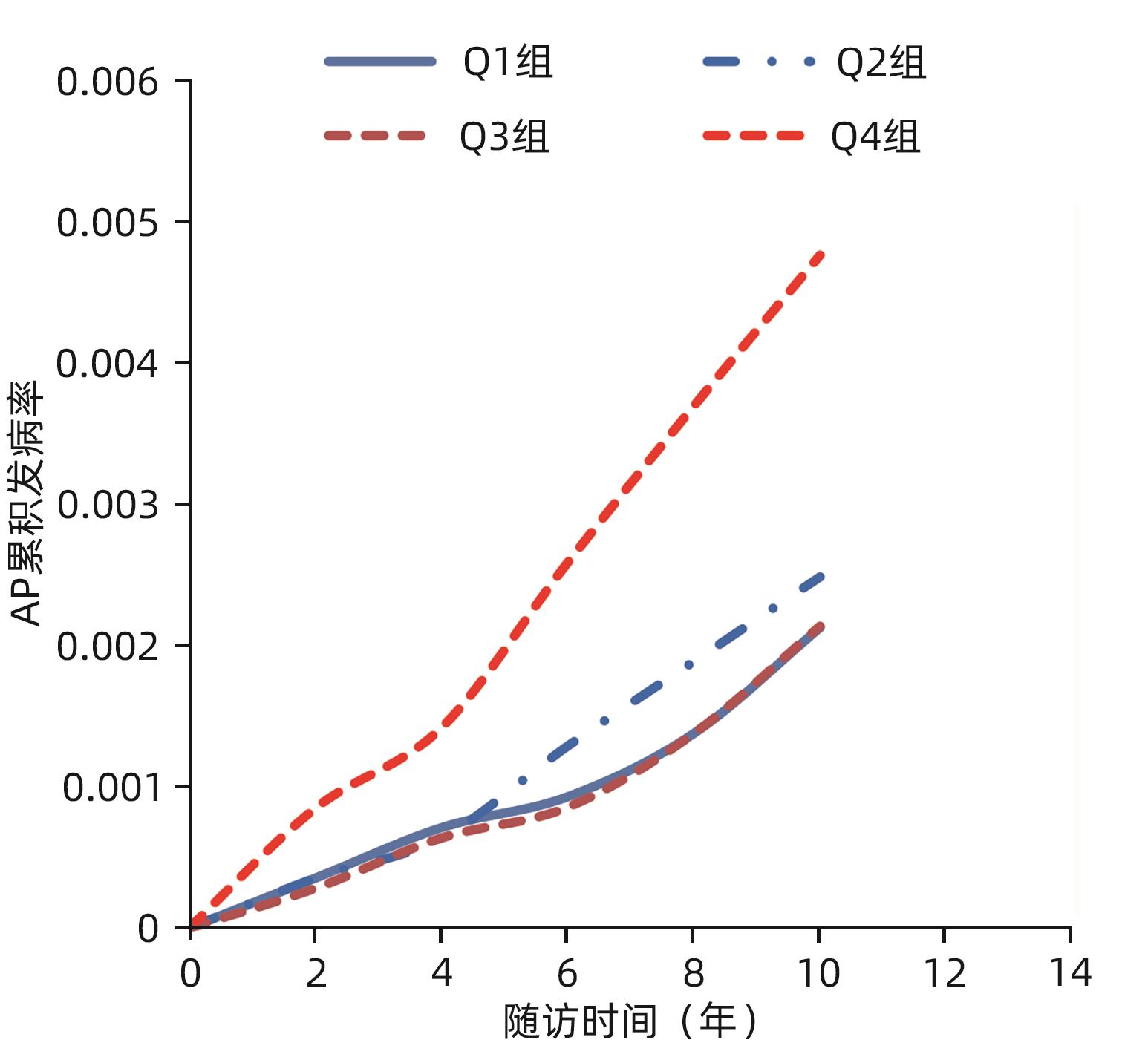
目的 探讨甘油三酯累积暴露(cumTG)与急性胰腺炎(AP)发病风险的关联。 方法 采用前瞻性队列研究方法,以连续参加2006—2010年度(2006、2008、2010年度)三次健康体检、既往无AP病史且TG资料完整的开滦职工56 883例为观察队列。根据计算的cumTG值按四分位数分为4组(Q1、Q2、Q3、Q4组),对组间一般资料进行比较。正态分布的计量资料多组间比较采用单因素方差分析;偏态分布计量资料多组间比较采用Kruskal-Wallis H检验。计数资料组间比较采用χ2检验。经Kaplan-Meier法绘制生存曲线并计算AP的累积发病率,用Log-rank法进行检验,采用Cox回归模型分析不同cumTG分组对新发AP事件的影响。 结果 随访(10.51±1.76)年,共发生AP事件158例,总发病密度为2.64/万人年;Q1、Q2、Q3、Q4组的发病例数及发病密度分别为29例(1.93/万人年)、34例(2.27/万人年)、30例(2.01/万人年)、65例(4.37/万人年)。Log-rank检验结果显示,各分组之间累积发病率差异有统计学意义(χ2=22.41,P<0.001)。多因素Cox回归模型显示:与Q1组比较,Q4组发生AP的HR=1.94,95%CI:1.20~3.13(P=0.01)。与TG累积暴露0年相比,累积暴露4、6年发生AP的HR分别是2.04(95%CI:1.26~3.30,P<0.01)、3.20(95%CI:1.98~5.17,P<0.01)。排除随访2年内发生的AP病例,重复多因素Cox回归分析,结果发现Q4组发生AP的HR=1.96,95%CI:1.23~3.12(P<0.01)。排除随访期间死亡人群后重复多因素Cox回归分析,结果发现Q4组发生AP的HR=1.85,95%CI:1.10~3.14(P<0.05)。 结论 随着cumTG的暴露增加,AP的发病率和发病风险均呈上升趋势。 Abstract:Objective To investigate the association between cumulative triglyceride (cumTG) exposure and the risk of acute pancreatitis (AP). Methods A prospective study was conducted for a cohort of 56 883 workers from Kailuan Group who participated in annual physical examination for three consecutive times in 2006-2010 (2006, 2008, and 2010) and had complete TG data without the medical history of AP. According to the quartiles of cumTG calculated, the subjects were divided into four groups (Q1, Q2, Q3, and Q4 groups), and general information was compared between the two groups. A one-way analysis of variance was used for comparison of normally distributed continuous data between multiple groups, and the Kruskal-Wallis H test was used for comparison of continuous data with skewed distribution between multiple groups; the chi-square test was used for comparison of categorical data between groups. The Kaplan-Meier method was used to plot the survival curve and calculate the cumulative incidence rate of AP, and the Log-rank test was used for comparison between groups; the Cox regression model was used to analyze the effect of different cumTG levels on new-onset AP events. Results After follow-up for 10.51±1.76 years, there were 158 AP events in total, with a total incidence density of 2.64 per 10 000 person-years, and the number of cases and incidence density in the Q1, Q2, Q3, and Q4 groups were 29 cases (1.93 per 10 000 person-years), 34 cases (2.27 per 10 000 person-years), 30 cases (2.01 per 10 000 person-years), and 65 cases (4.37 per 10 000 person-years). The Log-rank test showed that there was a significant difference in cumulative incidence rate between groups (χ2=22.41, P<0.001). The multivariate Cox regression analysis showed that compared with the Q1 group, the Q4 group had a significantly higher risk of AP (hazard ratio [HR]=1.94, 95% confidence interval [CI]: 1.20 — 3.13, P=0.01). Compared with cumulative triglyceride exposure for 0 year, cumulative triglyceride exposure for 4 and 6 years significantly increased the risk of AP, with an HR value of 2.04 (95%CI: 1.26 — 3.30, P<0.01) and 3.20 (95%CI: 1.98 — 5.17, P<0.01), respectively. After exclusion of the AP cases that occurred during the 2-year follow-up, the repeated multivariate Cox regression analysis showed that the Q4 group had an HR value of 1.96 (95%CI: 1.23 — 3.12, P<0.01) for the onset of AP, and after exclusion of the death cases during follow-up, the repeated multivariate Cox regression analysis showed that the Q4 group had an HR value of 1.85 (95%CI: 1.10 — 3.14, P<0.05) for the onset of AP. Conclusion The incidence rate and risk of AP tend to increase with the increase in cumTG exposure. -
Key words:
- Triglycerides /
- Acute Pancreatitis /
- Risk Factors
-
表 1 观察对象的一般资料
Table 1. Basic conditions of study objects
组别 例数 男/女(例) 年龄(岁) BMI(kg/m2) 收缩压(mmHg) 舒张压(mmHg) Q1组 14 203 9 965/4 238 52.54±12.46 23.68±3.15 126.3±19.28 81.27±10.62 Q2组 14 234 10 849/3 385 53.74±12.42 24.71±3.24 130.1±19.08 83.73±10.54 Q3组 14 233 1 1057/3 176 54.67±11.96 25.71±3.26 133.0±19.28 85.23±10.70 Q4组 14 213 11 651/2 562 53.38±11.31 26.39±3.21 135.0±18.97 87.03±10.85 统计值 χ2=566.30 F=77.04 F=1 920.31 F=558.22 F=737.97 P值 <0.001 <0.001 <0.001 <0.001 <0.001 组别 eGFR(mL/min) TC(mmol/L) TG(mmol/L) HDL-C(mmol/L) LDL-C(mmol/L) FPG(mmol/L) 降脂药[例(%)] Q1组 92.64±19.11 4.65±0.88 0.79(0.61~0.96) 1.71±0.53 2.34±0.76 5.32±1.13 54(0.38) Q2组 89.01±19.62 4.88±0.91 1.14(0.93~1.41) 1.58±0.46 2.60±0.75 5.53±1.38 110(0.78) Q3组 88.84±20.00 5.11±0.97 1.52(1.20~1.94) 1.51±0.44 2.72±0.82 5.74±1.59 161(1.14) Q4组 89.73±21.42 5.34±1.15 2.43(1.71~3.54) 1.43±0.47 2.72±0.90 6.01±1.86 319(2.26) 统计值 F=110.49 F=1 311.70 H=30 649.83 F=908.34 F=695.32 F=536.57 χ2=243.55 P值 <0.001 <0.001 <0.001 <0.001 <0.001 0.040 <0.001 组别 饮酒[例(%)] 吸烟[例(%)] 教育年限≥9年[例(%)] 体育锻炼≥3次/周[例(%)] 高血压病史[例(%)] 糖尿病病史[例(%)] 胆石症[例(%)] Q1组 628(4.44) 5 522(39.05) 3 864(27.32) 2 474(17.49) 6 949(49.14) 1 101(7.79) 556(3.93) Q2组 684(4.83) 6 024(42.50) 3 885(27.41) 2 631(18.56) 8 696(61.36) 1 736(12.25) 583(4.11) Q3组 828(5.84) 6 502(45.88) 3 803(26.84) 2 705(19.09) 9 830(69.37) 2 473(17.45) 640(4.52) Q4组 1 239(8.77) 7 361(52.11) 3 941(27.90) 2 481(17.56) 10 658(75.44) 3 339(23.64) 603(4.27) 统计值 χ2=286.89 χ2=528.81 χ2=4.03 χ2=17.95 χ2=2 379.85 χ2=1 532.68 χ2=6.75 P值 <0.001 <0.001 0.260 <0.001 <0.001 <0.001 0.080 注:饮酒、吸烟、教育年限、体育锻炼、降脂药、高血压病史、糖尿病病史、胆石症病史指标在统计时数据有缺失,Q1~Q4组分别缺失61例、61例、62例、86例。
表 2 不同cumTG水平分组影响AP事件的Cox比例风险回归模型分析
Table 2. Cox proportional hazards models for AP by cumTG level
自变量 β值 SE χ²值 P值 HR 95%CI 模型1 Q1组 1.00 Q2组 0.16 0.25 0.40 0.52 1.17 0.72~1.93 Q3组 0.04 0.26 0.02 0.89 1.04 0.62~1.73 Q4组 0.81 0.22 13.16 <0.01 2.25 1.45~3.48 1SD 0.15 0.02 63.24 <0.01 1.16 1.12~1.20 模型2 Q1组 1.00 Q2组 0.13 0.25 0.26 0.61 1.14 0.69~1.87 Q3组 -0.01 0.26 0.00 0.96 0.99 0.59~1.65 Q4组 0.76 0.22 11.46 <0.01 2.13 1.38~3.31 1SD 0.14 0.02 57.68 <0.01 1.15 1.11~1.20 模型3 Q1组 1.00 Q2组 0.18 0.26 0.46 0.50 1.19 0.72~1.99 Q3组 0.01 0.27 0.00 0.98 1.01 0.59~1.71 Q4组 0.66 0.25 7.25 0.01 1.94 1.20~3.13 1SD 0.13 0.02 30.10 <0.01 1.14 1.09~1.20 注:SD,标准差。模型1未校正混杂因素,模型2校正性别、年龄,模型3在模型2基础上进一步校正了TC、2010年TG、eGFR、体育锻炼、受教育年限、吸烟、 饮酒、高血压病史、糖尿病病史、胆石症病史、降脂药。
表 3 高TG累积暴露时间对AP事件影响的多因素Cox比例风险回归模型分析
Table 3. Multivariate Cox regression analysis of the effect of cumulative exposure years of hypertriglycerides on AP
模型 累积暴露时间(年) β值 SE χ²值 P值 HR 95%CI 模型1 0 1.00 2 0.26 0.22 1.37 0.24 1.30 0.84~2.01 4 0.81 0.24 11.76 <0.01 2.25 1.42~3.57 6 1.33 0.22 35.85 <0.01 3.78 2.45~5.85 模型2 0 1.00 2 0.23 0.23 1.05 0.31 1.26 0.81~1.94 4 0.77 0.24 10.53 <0.01 2.16 1.36~3.43 6 1.28 0.23 33.20 <0.01 3.61 2.33~5.59 模型3 0 1.00 2 0.21 0.23 0.81 0.37 1.23 0.79~1.92 4 0.71 0.25 8.34 <0.01 2.04 1.26~3.30 6 1.16 0.25 22.52 <0.01 3.20 1.98~5.17 注:模型1未校正混杂因素,模型2校正性别、年龄,模型3在模型2基础上进一步校正了TC、2010年TG、eGFR、体育锻炼、受教育年限、吸烟、 饮酒、高血压病史、糖尿病病史、胆石症病史、降脂药。
表 4 不同cumTG水平分组对随访2年后发生AP事件影响的Cox比例风险回归模型
Table 4. Cox proportional hazards models for AP by cumTG level after 2 year follow-up
自变量 β值 SE χ²值 P值 HR 95%CI Q1组 1.00 Q2组 0.18 0.26 0.49 0.49 1.20 0.72~2.00 Q3组 0.02 0.28 0.00 0.96 1.02 0.59~1.74 Q4组 0.67 0.24 7.98 <0.01 1.96 1.23~3.12 注:校正了TC、2010年TG、eGFR、性别、年龄、体育锻炼、受教育年限、吸烟、饮酒、高血压病史、糖尿病病史、胆石症病史、降脂药。
表 5 排除随访期间死亡人群后不同cumTG水平分组对AP事件影响的Cox比例风险回归模型
Table 5. Cox proportional hazards models for AP by different cumTG level after excluded death during follow-up
自变量 β值 SE χ²值 P值 HR 95%CI Q1组 1.00 Q2组 0.17 0.28 0.35 0.55 1.18 0.68~2.05 Q3组 0.01 0.29 0.00 0.97 1.01 0.57~1.79 Q4组 0.62 0.27 5.31 0.02 1.85 1.10~3.14 注:校正了TC、2010年TG、eGFR、性别、年龄、体育锻炼、受教育年限、吸烟、 饮酒、高血压病史、糖尿病病史、胆石症病史、降脂药。
-
[1] ROBERTS SE, MORRISON-REES S, JOHN A, et al. The incidence and aetiology of acute pancreatitis across Europe[J]. Pancreatology, 2017, 17( 2): 155- 165. DOI: 10.1016/j.pan.2017.01.005. [2] LIN HH, CHANG HY, CHIANG YT, et al. Smoking, drinking, and pancreatitis: A population-based cohort study in Taiwan[J]. Pancreas, 2014, 43( 7): 1117- 1122. DOI: 10.1097/MPA.0000000000000209. [3] GRAJALES-FIGUEROA G, DÍAZ HERNÁNDEZ HA, CHACÓN PORTILLO MA, et al. Increased mortality from extrapancreatic infections in hospitalized patients with acute pancreatitis[J]. Gastroenterol Res Pract, 2019, 2019: 2789764. DOI: 10.1155/2019/2789764. [4] JIN JL, SUN D, CAO YX, et al. Intensive genetic analysis for Chinese patients with very high triglyceride levels: Relations of mutations to triglyceride levels and acute pancreatitis[J]. EBioMedicine, 2018, 38: 171- 177. DOI: 10.1016/j.ebiom.2018.11.001. [5] REID GP, WILLIAMS EW, FRANCIS DK, et al. Acute pancreatitis: A 7 year retrospective cohort study of the epidemiology, aetiology and outcome from a tertiary hospital in Jamaica[J]. Ann Med Surg(Lond), 2017, 20: 103- 108. DOI: 10.1016/j.amsu.2017.07.014. [6] HONG WD, ZIMMER V, BASHARAT Z, et al. Association of total cholesterol with severe acute pancreatitis: A U-shaped relationship[J]. Clin Nutr, 2020, 39( 1): 250- 257. DOI: 10.1016/j.clnu.2019.01.022. [7] Expert group of emergency expert consensus on diagnosis and treatment of hypertriglyceridemic acute pancreatitis. Emergency expert consensus on diagnosis and treatment of hypertriglyceridemic acute pancreatitis[J]. Chin Gen Pract, 2021, 24( 30): 3781- 3793. DOI: 10.12114/j.issn.1007-9572.2021.02.028.《高甘油三酯血症性急性胰腺炎诊治急诊专家共识》专家组. 高甘油三酯血症性急性胰腺炎诊治急诊专家共识[J]. 中国全科医学, 2021, 24( 30): 3781- 3793. DOI: 10.12114/j.issn.1007-9572.2021.02.028. [8] TENNER S, BAILLIE J, DEWITT J, et al. American college of gastroenterology guideline: Management of acute pancreatitis[J]. Am J Gastroenterol, 2013, 108( 9): 1400- 1415. DOI: 10.1038/ajg.2013.218. [9] BERGLUND L, BRUNZELL JD, GOLDBERG AC, et al. Evaluation and treatment of hypertriglyceridemia: An endocrine society clinical practice guideline[J]. J Clin Endocrinol Metab, 2012, 97( 9): 2969- 2989. DOI: 10.1210/jc.2011-3213. [10] JI RG, ZHU GL, ZHANG B, et al. Association between dyslipidemia and acute pancreatitis: A prospective cohort study[J]. J Clin Hepatol, 2019, 35( 7): 1536- 1540. DOI: 10.3969/j.issn.1001-5256.2019.07.023.吉瑞更, 朱国玲, 张冰, 等. 血脂异常对急性胰腺炎发病影响的前瞻性队列研究[J]. 临床肝胆病杂志, 2019, 35( 7): 1536- 1540. DOI: 10.3969/j.issn.1001-5256.2019.07.023. [11] WANG GD, SONG L, ZHAO HL, et al. Predictive value of cumulative blood pressure exposure to stroke events[J]. Chin J Hypertens, 2017, 25( 8): 773- 778. DOI: 10.16439/j.cnki.1673-7245.2017.08.026.汪国栋, 宋路, 赵华灵, 等. 累积血压暴露值对脑卒中事件的预测价值[J]. 中华高血压杂志, 2017, 25( 8): 773- 778. DOI: 10.16439/j.cnki.1673-7245.2017.08.026. [12] WANG JR, HU YQ, SHI HJ, et al. Study on the assiociation between cumulative uric acid and brachial-ankle pulse velocity[J]. Chin J Rheumatol, 2019, 4( 23): 220- 227. DOI: 10.3760/cma.j.issn.1007-7480.2019.04.002.王洁蕊, 胡玉琴, 石慧婧, 等. 累积尿酸暴露与臂踝动脉脉搏波传导速度的关系[J]. 中华风湿病学杂志, 2019, 4( 23): 220- 227. DOI: 10.3760/cma.j.issn.1007-7480.2019.04.002. [13] WU SL, HUANG ZR, YANG XC, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city[J]. Circ Cardiovasc Qual Outcomes, 2012, 5( 4): 487- 493. DOI: 10.1161/CIRCOUTCOMES.111.963694. [14] ZHU GL, CHEN SH, FAN XD, et al. A prospective cohort study on BMI levels and risk of acute pancreatitis[J]. Chin J Epidemiol, 2021, 42( 12): 2131- 2137. DOI: 10.3760/cma.j.cn112338-20201027-01286.朱国玲, 陈朔华, 樊学东, 等. 基线BMI水平对急性胰腺炎发病风险影响的前瞻性队列研究[J]. 中华流行病学杂志, 2021, 42( 12): 2131- 2137. DOI: 10.3760/cma.j.cn112338-20201027-01286. [15] ZHANG B, ZHU GL, SUN Q, et al. Baseline fasting glucose and risk of acute pancreatitis: A prospective cohort study[J]. Chin Gen Pract, 2021, 24( 1): 60- 64. DOI: 10.12114/j.issn.1007-9572.2020.00.602.张冰, 朱国玲, 孙秋, 等. 基线空腹血糖水平与急性胰腺炎发病风险的前瞻性队列研究[J]. 中国全科医学, 2021, 24( 1): 60- 64. DOI: 10.12114/j.issn.1007-9572.2020.00.602. [16] Writing Group of 2018 Chinese Guidelines for the Management of Hypertension, Chinese Hypertension League, Chinese Society of Cardiology, et al. Chinese guidelines for the management of hypertension(2018 revised edition)[J]. Chin J Cardiovasc Med, 2019, 24( 1): 24- 56. DOI: 10.3969/j.issn.1007-5410.2019.01.002.中国高血压防治指南修订委员会, 高血压联盟(中国), 中华医学会心血管病学分会, 等. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志, 2019, 24( 1): 24- 56. DOI: 10.3969/j.issn.1007-5410.2019.01.002. [17] Chinese Diabetes Society. Guidelines for the prevention and control of type 2 diabetes in China(2017 Edition)[J]. Chin J Pract Intern Med, 2018, 38( 4): 292- 344. DOI: 10.19538/j.nk2018040108.中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2017年版)[J]. 中国实用内科杂志, 2018, 38( 4): 292- 344. DOI: 10.19538/j.nk2018040108. [18] Pancreas Study Group, Chinese Society of Gastroenterology, Chinese Medical Association; Editorial Board of Chinese Journal of Pancreatology; Editorial Board of Chinese Journal of Digestion. Chinese guidelines for the management of acute pancreatitis(Shenyang, 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2706- 2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013.中华医学会消化病学分会胰腺疾病学组,《中华胰腺病杂志》编委会,《中华消化杂志》编委会. 中国急性胰腺炎诊治指南(2019年, 沈阳)[J]. 临床肝胆病杂志, 2019, 35( 12): 2706- 2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013. [19] SU W, GUO F. Triglyceride-controlling during acute phase of hypertriglyceridemia induced pancreatitis[J]. Chin J Dig Surg, 2023, 22( 1): 89- 93. DOI: 10.3760/cma.j.cn115610-20221220-00755.苏伟, 郭丰. 高甘油三酯血症性胰腺炎急性期的血脂控制[J]. 中华消化外科杂志, 2023, 22( 1): 89- 93. DOI: 10.3760/cma.j.cn115610-20221220-00755. [20] WU YQ, ZHAO JC. Predictive value of Ranson score in the classification of moderate to severe hyperlipidemia acute pancreatitis[J]. J Clin Exp Med, 2022, 21( 2): 222- 225. DOI: 10.3969/j.issn.1671-4695.2022.02.029.吴永强, 赵景成. Ranson评分在高脂血症性急性胰腺炎病情严重程度评估中的应用价值[J]. 临床和实验医学杂志, 2022, 21( 2): 222- 225. DOI: 10.3969/j.issn.1671-4695.2022.02.029. [21] Joint committee for guideline revision. 2016 Chinese guidelines for the management of dyslipidemia in adults[J]. J Geriatr Cardiol, 2018, 15( 1): 1- 29. DOI: 10.11909/j.issn.1671-5411.2018.01.011. [22] ZHU GL, ZHANG B, JI RG, et al. A prospective cohort study on triglycerides levels and risk of acute pancreatitis[J]. Chin J Dig, 2018, 38( 12): 829- 834. DOI: 10.3760/cma.j.issn.0254-1432.2018.12.008.朱国玲, 张冰, 吉瑞更, 等. 基线三酰甘油水平与急性胰腺炎发病风险的前瞻性队列研究[J]. 中华消化杂志, 2018, 38( 12): 829- 834. DOI: 10.3760/cma.j.issn.0254-1432.2018.12.008. [23] LINDKVIST B, APPELROS S, REGNÉR S, et al. A prospective cohort study on risk of acute pancreatitis related to serum triglycerides, cholesterol and fasting glucose[J]. Pancreatology, 2012, 12( 4): 317- 324. DOI: 10.1016/j.pan.2012.05.002. [24] PEDERSEN SB, LANGSTED A, NORDESTGAARD BG. Nonfasting mild-to-moderate hypertriglyceridemia and risk of acute pancreatitis[J]. JAMA Intern Med, 2016, 176( 12): 1834- 1842. DOI: 10.1001/jamainternmed.2016.6875. [25] EWALD N, HARDT PD, KLOER HU. Severe hypertriglyceridemia and pancreatitis: Presentation and management[J]. Curr Opin Lipidol, 2009, 20( 6): 497- 504. DOI: 10.1097/MOL.0b013e3283319a1d. [26] GERASIMENKO JV, GERASIMENKO OV, PETERSEN OH. The role of Ca2+ in the pathophysiology of pancreatitis[J]. J Physiol, 2014, 592( 2): 269- 280. DOI: 10.1113/jphysiol.2013.261784. [27] ZHANG XL, LI F, CUI YQ, et al. The role of oxide stress during the pathogenesis of chronic pancreatic injuries induced by chronic high-fat diets in rat[J]. Chin J Surg, 2012, 50( 7): 646- 649. DOI: 10.3760/cma.j.issn.0529-5815.2012.07.019.张小丽, 李非, 崔叶青, 等. 氧应激在慢性胰腺损伤发生中的表达变化[J]. 中华外科杂志, 2012, 50( 7): 646- 649. DOI: 10.3760/cma.j.issn.0529-5815.2012.07.019. [28] VALDIVIELSO P, RAMIREZ-BUENO A, EWALD N. Current knowledge of hypertriglyceridemic pancreatitis[J]. Eur J Intern Med, 2014, 25( 8): 689- 694. DOI: 10.1016/j.ejim.2014.08.008. [29] RAWLA P, SUNKARA T, THANDRA KC, et al. Hypertriglyceridemia-induced pancreatitis: updated review of current treatment and preventive strategies[J]. Clin J Gastroenterol, 2018, 11( 6): 441- 448. DOI: 10.1007/s12328-018-0881-1. [30] Joint Committee on the Chinese Guidelines for Lipid Management. Chinese guidelines for lipid management(2023)[J]. Chin J Cardiol, 2023, 51( 3): 221- 255. DOI: 10.3760/cma.j.cn112148-20230119-00038.中国血脂管理指南修订联合专家委员会. 中国血脂管理指南(2023年)[J]. 中华心血管病杂志, 2023, 51( 3): 221- 255. DOI: 10.3760/cma.j.cn112148-20230119-00038. -



 PDF下载 ( 770 KB)
PDF下载 ( 770 KB)

 下载:
下载:


