Value of hepatic artery resistance index in evaluating progressive liver fibrosis in nonalcoholic fatty liver disease
-
摘要: 目的明确非酒精性脂肪性肝病(NAFLD)患者血流相关指数的变化,探讨肝动脉血流阻力指数在进展期肝纤维化中的应用价值。方法选取公安县人民医院2016年1月-2017年12月确诊为NAFLD的患者148例及健康志愿者60例为研究对象,采集空腹静脉血测定肝功能、血常规,计算NAFLD患者的NAFLD纤维化评分(NFS)。按NFS结果将NAFLD患者分为A组(NFS≤0. 676)、B组(NFS>0. 676),以健康人群作为对照组。所有研究对象应用多普勒超声测量肝门静脉峰值(PPVV)、门静脉平均流速(MPVV)及肝动脉血流阻力指数(HARI)。计量资料3组间比较先进行方差分析,若有差异再采用SNK-q法进行多重比较;计数资料组间比较采用χ2检验。采用Spearman秩相关分析不同评价指标间的相关性。结果 148例患者中A组121例,B组27例,HARI值在A组(0. 64±0. 08)、健康对照组(0. 76±0. 09)、B组(0. 88±0. 05)中依次增高,差异有统计学意义(F=4. 981,P <0. 01),MPVV、PPVV在健康人群[(22. 84±3. 12)...Abstract: Objective To investigate the changes in blood flow indices in patients with nonalcoholic fatty liver disease (NAFLD) and the value of hepatic artery resistance index (HARI) in evaluating progressive liver fibrosis. Methods A total of 148 patients who were diagnosed with NAFLD in The People's Hospital of Gong'an County from January 2016 to December 2017 and 60 healthy volunteers were selected as study subjects. Fasting venous blood samples were collected for liver function evaluation and routine blood test, and then NAFLD fibrosis score (NFS) was calculated for NAFLD patients. According to NFS, the patients with NAFLD were divided into group A (NFS ≤0. 676) and group B (NFS > 0. 676) . The healthy volunteers were enrolled as control group. Color Doppler ultrasound was performed to measure peak portal vein velocity (PPVV) , mean portal vein velocity (MPVV) , and HARI in all subjects. An analysis of variance was used for comparison of continuous data between three groups, and the SNK-q test was used for multiple comparisons; the chi-square test was used for comparison of categorical data between groups. A Spearman' s rank correlation analysis was used to investigate the correlation between assessment indices. Results There were 121 patients in group A and 27 in group B. Group B had the highest HARI (0. 88 ± 0. 05) , followed by the control group (0. 76 ± 0. 09) and group A (0. 64 ± 0. 08) , and there was a significant difference between groups (F =4. 981, P < 0. 01) . The control group had the highest MPVV (22. 84 ± 3. 12 cm/s) and PPVV (19. 02 ± 1. 97 cm/s) , followed by group A (17. 84 ± 2. 87 cm/s and 15. 29 ± 2. 02 cm/s) and group B (15. 31 ± 2. 29 cm/s and 13. 39 ± 1. 92 cm/s) , and there were significant differences between groups (F = 5. 645 and 7. 435, both P < 0. 01) . In the patients with NAFLD, HARI was positively correlated with NFS (r = 0. 763, P < 0. 01) , and MPVV and PPVV were negatively correlated with NFS (r =-0. 463 and-0. 425, both P < 0. 01) . Conclusion There are hemodynamic changes of the liver in NAFLD patients with progressive liver fibrosis. HARI can be used as a noninvasive method to evaluate whether NAFLD patients develop progressive liver fibrosis. The development of progressive liver fibrosis should be considered in case of abnormal increase in HARI.
-
Key words:
- nonalcoholic fatty liver disease /
- liver cirrhosis /
- hepatic artery /
- hemodynamics
-
肝癌是我国常见恶性肿瘤之一,在常见的恶性肿瘤中,肝癌发病率位居全国第五,死亡率居第二,据估测每年新发肝癌病例46万例,5年相对生存率仅为12.1%。肝癌的发病机制复杂,其发生发展与多种危险因素相关,如病毒性肝炎、肝硬化、非酒精性脂肪性肝病、酒精性脂肪性肝病、黄曲霉素等。目前,治疗肝癌的最有效方法为手术切除,早期诊断和治疗是提高手术疗效的关键[1-4]。因此,开发早期检测工具和创新型靶向药物是提升早期诊断准确度、增强肝癌临床治疗效果的有效途径,目前相关研究主要集中在:(1)发现提高早期预测和诊断能力的精准生物标志物;(2)揭示肝癌发生发展的关键基因及信号通路;(3)药物研发的潜在分子机制分析及药品有效性、安全性评估;(4)个体化精准治疗方案的探索。上述研究均需建立在高质量的人体生物样本的采集、保存及管理之上。
生物样本库作为病因学研究的重要资源平台,其在基础医学研究迈向精准医学研究的过程中发挥了重要作用。近年来,随着医学研究对高质量生物样本的迫切需求,不同类型的人类生物样本库建设在世界各大医学院、医疗机构中获得快速发展。早期国际上出现的英国生物样本库、泛欧洲生物样本库与分子生物资源研究中心及美国国家癌症研究所下属的生物样本库和生物样本研究分会等,均为疾病的病因学研究提供了可靠的样本资源。我国生物样本库在国家医学科技发展规划下得到了跨越式发展,涌现了一批以人口为导向和以疾病为导向的不同类型的生物样本库。其中,以疾病为导向的临床生物样本库由于其复杂性,通常起源于医疗机构,建立在医院内部,有自己独立的操作空间和管理制度[5-7]。该类型临床生物样本库目前已有广泛的应用,例如以肿瘤为主的生物样本库、特殊疾病生物样本库等,这些样本库均为相关研究提供了重要样本资源[8-13]。
2012年以前,同济医院肝脏外科肝癌相关研究的临床样本根据课题的不同需求,由各课题组成员分别完成采集、保存和管理工作,操作流程与要求不一致,样本质量参差不齐,临床数据与随访信息也缺少统一标准,利用率较低。2012年,同济医院正式组建了生物样本库与生物资源研究中心,聚焦肝癌样本的采集、保存与管理,为国家重大科技专项“病毒性肝炎相关肝癌样本库的建设维护及基线水平调查”的研究提供了强有力支撑。本文主要总结了2012年—2020年肝脏外科生物样本库样本储存情况,根据采集、保存、出入库及信息管理等流程,制定标准化操作制度和信息化管理措施,并对已入库保存的冷冻样本质量进行评估,拟构建一个合格的生物资源研究平台,为肝癌研究提供高质量的临床样本和临床数据信息。
1. 资料与方法
1.1 研究对象
本研究的所有样本来源于2012年8月—2020年12月就诊于华中科技大学同济医学院附属同济医院肝脏外科的肝癌患者,纳入标准:(1)术前影像学诊断为肝癌;(2)拟进行腹腔镜切除术或开腹手术;(3)术后病理诊断为肝细胞癌。排除标准:(1)术后病理诊断为良性肿瘤或非肝癌的恶性肿瘤;(2)其他肿瘤转移至肝脏的转移性癌。排除后的样本将纳入其他疾病样本库。
1.2 仪器设备
-80 ℃超低温冰箱(DW-86L626,海尔,青岛),双门及多门电冰箱(KK18V011CW,西门子,中国),液氮罐(CY509111CN,Thermo,美国),低温标签打印机(IP300,Brady,美国),冰箱无线温度监控系统(YB-HC004-00,海尔,青岛),二氧化碳后备系统(BZ07A0B01,海尔,青岛),生物样本库管理系统(BIMS,海尔,青岛),生物安全柜(HFsafe-1200A2,力康,上海),低速离心机(L500,湘仪,湖南),高通量组织研磨器(18-G136,新芝,宁波),生物组织包埋机(EG1160,LEICA,德国),石蜡切片机(RM2235,LEICA,德国),脱水机(TP1020,LEICA,德国),微量紫光分光光度计(NanoDrop 2000,Thermo,美国)。
1.3 样本的采集及处理
1.3.1 血液的采集及处理
对符合纳排标准的患者进行术前、术中、术后外周血样本的采集,用促凝管和抗凝管分别采集外周血各5 mL,颠倒混匀,其中促凝管3200 r/min离心10 min,置于超净工作台中分离血清;抗凝管全血直接分装,-80 ℃冻存。
1.3.2 组织的采集及处理
(1) 新鲜组织:对符合纳排标准的患者在不影响病理诊断所需材料的前提下,进行新鲜组织样本的采集,尽量采集未坏死癌组织,癌旁组织选择距离癌灶边缘3 cm处的组织样本,远癌组织选择距癌灶边缘5 cm以上或距离癌灶边缘最远端(或手术切缘处)的组织样本,并对样本进行拍摄及标注位置。组织样本的量一般不少于200 mg,其中一份样本加入RNALater保护液,样本切除后迅速置于液氮中保存,整个取样过程尽量在手术样本离体后30 min内完成。(2)石蜡包埋组织:取材操作规范同新鲜组织,取材部位包括癌灶、癌与癌旁交界处、癌灶周围3 cm处的癌旁组织和5 cm以外的远癌组织。取材以癌灶为中心水平向两侧取材,尽量保证足够大的组织样本。取材以“远癌-癌旁-癌与癌旁交界处-癌灶”的顺序,所有组织块进行拍摄且标明取材部位,最后用中性福尔马林溶液固定。固定后的组织经过“取材-脱水-透明-浸蜡-包埋”过程之后,完成组织样本的石蜡包埋。
1.3.3 粪便的采集及处理
本研究收集患者术前、术后的粪便,用取便器采集患者样本后,将样本置于超净工作台中进行分装,每份1~2 g。其中两份加入1.5 mL 20%无菌甘油,含2颗小钢珠,60 Hz 60 s震荡混匀后,吸至冻存管-80 ℃冻存;另外两份直接-80 ℃冻存。
1.4 样本的保存
血液、新鲜组织及粪便样本完成采集与处理后,分装至若干个Ep管进行低温入库储存。通过生物样本库管理系统(BIMS)注册患者基本信息,并关联对应样本信息,打印标签条贴至各Ep管,放置于-80 ℃冰箱对应位置保存。每台-80 ℃冰箱都配有无线温度监控系统和二氧化碳后备系统,可设置低温预警提示,以保证样本低温环境的稳定性。石蜡包埋组织同样进行标签与分类后,放置于石蜡柜室温保存。
1.5 临床数据采集及随访跟踪
患者临床数据的采集主要通过本院电子病历系统完成,包括患者从门诊到住院的所有信息,数据的内容主要是基本信息(年龄、性别、BMI等)、既往史(饮酒、吸烟、肥胖等)、基础肝病(肝硬化、病毒性肝炎、脂肪肝、血吸虫、门静脉高压等)、肝功能(Alb、ALT、AST、TBil、PTA、胆固醇、胆汁酸等)、影像学诊断(B超、CT、磁共振等)、治疗手段及方法(腹腔镜、开腹、切除范围、阻断方式等)、肿瘤特性(Child分级、BCLC分期、TNM分期、肿瘤标志物等)及术后并发症(腹水、胸水、肝衰竭、腹腔感染等)。定期进行患者的追踪随访工作,主要通过电话随访和门诊随访两种形式。
1.6 样本质量控制与检测
根据样本入库时间,随机抽取不同年份的肝癌及癌旁冷冻组织样本,进行总RNA的提取及检测。按照试剂盒说明书完成RNA的提取,NanoDrop检测其浓度,Agilent 5400检测其完整性和纯度。
1.7 样本的管理及使用
保存好的样本在完成病历录入和跟踪随访后,即可投入使用。样本库有专门的管理小组,负责审批样本使用权限。各研究小组成员如需使用样本库样本,使用者需向样本库管理小组提交申请,管理小组审核批准后,交由工作人员查询所需患者ID,找到对应样本位置信息,完成样本的出库。样本的出入库都在低温环境中进行。样本出库进入研究项目后,若研究结束时样本全部用完,则需告知工作人员对该样本进行注销,若存在剩余样本则需归还再次入库保存。
2. 结果
2.1 样本收集情况
2012年8月—2020年12月样本库共收集4190例肝癌手术患者样本,其中包括41 718份冷冻组织样本、18 950份石蜡包埋组织样本、24 389份全血样本、20 060份血清样本和5392份粪便样本。所收集肝癌患者的年龄范围为13~88岁;男性占比85.1%;66.7%的患者无饮酒史;乙型肝炎和肝硬化的比例较高,分别为83.3%和73.5%;11.5%的患者伴门静脉高压症(表 1)。
表 1 样本库肝癌患者基础信息表Table 1. The general information of liver cancer patients in biobank基本信息 例数 年龄(岁) ≤50 1734 >50 2456 性别 男 3566 女 624 饮酒 是 843 否 2796 不详 551 乙型肝炎 是 3492 否 698 肝硬化 是 3081 否 1109 门静脉高压 是 483 否 3062 不详 645 2.2 标准化操作流程的建立
样本库具有独立的工作空间,共设置6个工作区域:样本处理区、样本出入库管理区、临床数据库及随访区、质检实验区、-80 ℃样本冷冻区和液氮冷冻区。本库配备6名专职人员,冷冻区实现实时监控。根据样本的收集、处理、保存、管理及应用,制定出一份标准的操作流程(standard operating procedure,SOP)(图 1)。
2.3 样本质量检测
从样本库保存的冷冻组织样本中,随机挑选出2012年—2020年的肝癌及癌旁组织样本18份,提取总RNA。检测结果为A的16份样本RNA浓度及完整性均达到高质量等级,能够满足后续PCR、转录组测序等实验需求;2份癌组织样本检测结果为C,主因RNA的完整度不足,说明其质量处于中等级别,可能会影响后续实验的进行(表 2)。总体上,样本库组织样本保存质量较高,少数保存时间较长的癌组织中RNA可能发生降解,从而影响了检测结果。
表 2 肝癌组织样本RNA检测结果Table 2. The RNA detection results on tissue samples of liver cancer编号 年份 组织部位 浓度(ng/μL) 完整性值 检测结论 1 2012 癌 517 4.30 C 2 2012 癌旁 804 5.60 A 3 2013 癌 557 4.10 C 4 2013 癌旁 501 6.60 A 5 2014 癌 369 5.70 A 6 2014 癌旁 754 6.90 A 7 2015 癌 324 5.80 A 8 2015 癌旁 754 6.90 A 9 2016 癌 509 6.40 A 10 2016 癌旁 500 6.00 A 11 2017 癌 467 5.30 A 12 2017 癌旁 933 9.30 A 13 2018 癌 447 8.20 A 14 2018 癌旁 1148 9.20 A 15 2019 癌 1325 8.60 A 16 2019 癌旁 760 9.50 A 17 2020 癌 945 9.90 A 18 2020 癌旁 477 9.40 A 2.4 信息化数据查询及管理
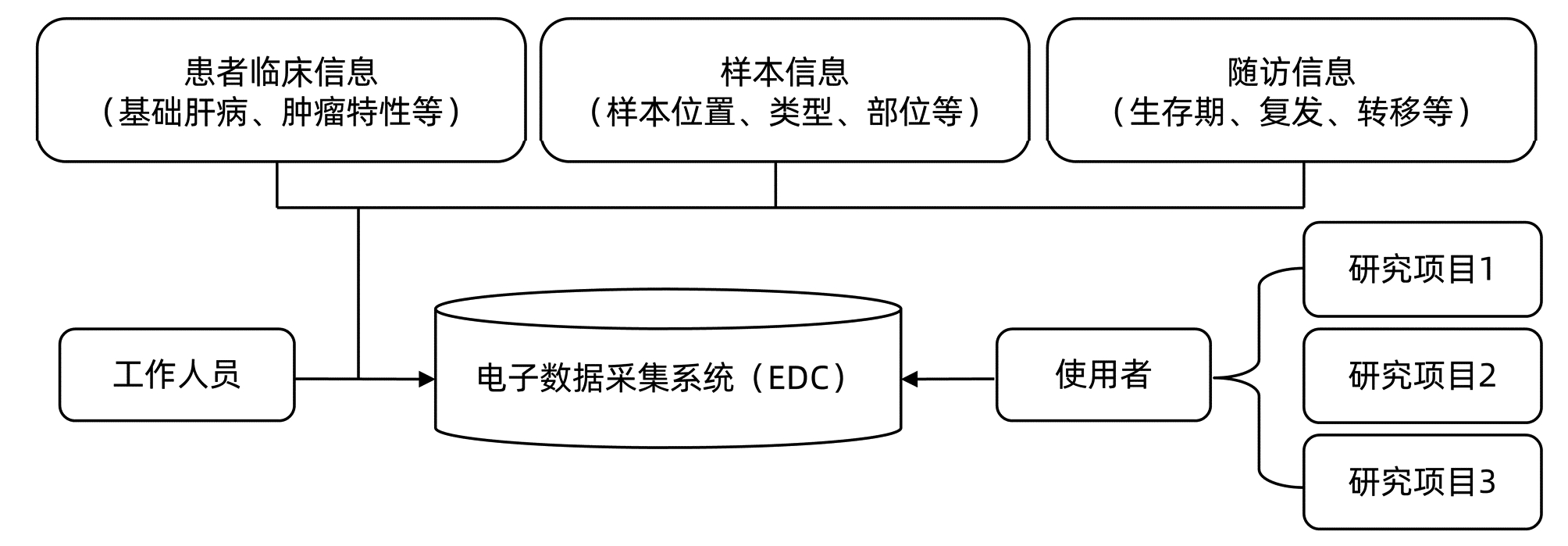
为实现各版块数据的关联,样本库建立了一套电子数据采集系统(electronic data capture system,EDC)(图 2),将从电子病历系统中采集的患者信息、样本出入库系统的样本信息和随访信息进行关联,实现模糊查询关联信息功能,并标注纳入不同研究项目的患者及所用样本,方便使用者查询样本的应用情况。
3. 讨论
本科室肝癌生物样本库的标准化建设与信息化管理为样本质量提供了有力保障,也充分挖掘了样本的科研价值,支撑本科室承担的多个国家级课题顺利推进,在国内外高水平期刊上发表数篇文章[14-17]。其中Song等[14]通过检测样本库的肝癌组织,发现分子伴侣蛋白14-3-3σ在癌组织中表达增高,高表达的14-3-3σ与肝癌侵袭性临床病理特征和预后不良相关。深入研究表明,14-3-3σ通过抑制表皮生长因子受体降解从而激活依赖表皮生长因子受体的ERK1/2信号通路,促进肝癌细胞的逃避失巢凋亡效应和肿瘤转移。Liao等[15]在样本库肝癌组织样本中发现pSMAD3/SMAD3与PTPRε表达呈正相关,且SMAD3或PTPRε高表达与肝癌患者预后不良相关。本文还揭示了TGFβ/SMAD3和PTPRe之间的正反馈调节,为肝癌的侵袭转移提供新的研究思路及治疗靶点。
但本样本库也存在一些问题,有待进一步加强改进和完善。本样本库建设面积200平方米,属于以疾病为导向的小型生物样本库,服务对象主要是本科室医生、科研人员和学生,受利面较窄,尚未实现与其他样本库的样本与信息的共建共享。因本科室近年承担的肝癌与肠道菌群关系研究的课题需要,本库增加了粪便样本的采集与保藏工作,但由于采集启动时间较晚且人员配置不足,样本量不大,今后需进一步增加人员配备,丰富样本库样本的种类与数量,为后续课题研究提供坚实数据基础。
在患者病历信息的采集方面,还存在一些漏项,主要原因是电子病历系统填写不详实,需进一步加强与临床医生间的紧密联系,及时查询入库样本来源患者的电子病历,确保入库样本来源患者相关临床信息的完整准确性,为后续随访信息收集等工作奠定基础。
衡量样本库样本保存质量的核心指标之一是冻存样本的RNA检测,从本次检测结果来看,本样本库冻存7年内(2014年—2020年)的样本质量较高,占本次检测总量的77.8%,可满足肝癌研究的要求;冻存7年以上(2012年—2013年) 的部分组织样本存在RNA降解的问题,占本次检测总量的11.1%,质量较差,无法完全满足肝癌研究的要求。在今后的样本利用中,应进一步加快样本利用效率,在样本采集入库后,尽快应用到各项课题研究中去。
工作人员的专业性是保障样本库持续发展的关键,本样本库专职人员均持有相关合格证书,并不定期参加国内生物样本库相关会议培训,据统计,2012年—2020年参加相关会议培训54人次。随着国内外研究者对生物样本库关注度的不断提升,新一代信息网络技术与生物、医疗技术的迭代升级,生物样本库建设标准与技术正处在不断更新提档的快速发展期,在样本收集、储藏、运输、分配、检索、伦理、信息和安全等方面都产生了一系列规范标准[18-20],客观上要求样本库专职人员必须不断学习,接受专业培训,提升样本库建设与管理标准,努力建设成为服务肝脏基础科研的高效生物资源研究平台。
-
[1] NOUREDDIN M, LAM J, PETERSON MR, et al. Utility of magnetic resonance imaging versus histology for quantifying changes in liver fat in nonalcoholic fatty liver disease trials[J]. Hepatology, 2013, 58 (6) :1930-1940. [2] National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease:A 2018 update[J]. J Clin Hepatol, 2018, 34 (5) :947-957. (in Chinese) 中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会.非酒精性脂肪性肝病防治指南 (2018年更新版) [J].临床肝胆病杂志, 2018, 34 (5) :947-957. [3] FAN RB, FANG XL, MENG ZH, et al. Arelative research of renal interstitial fibrosis using ultrasonography and dynamic computer tomography contrast scan[J]. J Pract Med Tech, 2008, 15 (18) :2313-2315. (in Chinese) 范锐斌, 方先来, 孟志华, 等.超声与动态增强CT扫描诊断肾间质纤维化的对比研究[J].实用医技杂志, 2008, 15 (18) :2313-2315. [4] LI ZX, HE Y, WU J, et al. Study on serum fibrosis markers in hepatic fibrosis and hemodynamics on Doppler ultrasonography in infant hepatitis syndrome[J]. Chin J Ultrasound, 2005, 21 (6) :436-440. (in Chinese) 李智贤, 何云, 吴棘, 等.婴儿肝炎综合征的超声和血清肝纤维化标志物检测研究[J].中国超声医学杂志, 2005, 21 (6) :436-440. [5] GUO ZQ, WANG QY, QI XS, et al. Recommendations for the diagnosis and management of nonalcohilic fatty liver diseases:Practice guidance from the American Association for the Study of Liver Diseases (2017) [J]. J Clin Hepatol, 2017, 33 (12) :2275-2277. (in Chinese) 郭泽淇, 王倩怡, 祁兴顺, 等.《2017年美国肝病学会非酒精性脂肪性肝病诊疗指导》摘译[J].临床肝胆病杂志, 2017, 33 (12) :2275-2277. [6] MUSSO G, GAMBINO R, CASSADER M, et al. Meta-analysis:Natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity[J]. Ann Med, 2011, 43 (8) :617-649. [7] NASR P, IGNATOVA S, KECHAGIAS S, et al. Natural history of nonalcoholic fatty liver disease:A prospective follow-up study with serial biopsies[J]. Hepatol Commun, 2017, 2 (2) :199-210. [8] LI Y, LU LG. Molecular basis of hepatic fibrosis and current status of its diagnosis and treatment[J]. J Clin Hepatol, 2018, 34 (1) :12-15. (in Chinese) 李妍, 陆伦根.肝纤维化的分子基础与临床诊治现状[J].临床肝胆病杂志, 2018, 34 (1) :12-15. [9] HAGSTROM H, ELFWEN O, HULTCRANTZ R, et al. Is not associated with an increased risk for fibrosis progression in nonalcoholic fatty liver disease[J]. Gastroenterol Res Pract, 2018, 2018:1942648. [10] TOPAL NB, ORCAN S, SIGˇIRI D, et al. Effects of fat accumulation in the liver on hemodynamic variables assessed by Doppler ultrasonography[J]. J Clin Ultrasound, 2015, 43 (1) :26-33. [11] BALASUBRAMANIAN P, BOOPATHY V, GOVINDASAMY E, et al.Assessment of portal venous and hepatic artery haemodynamic variation in non-alcoholic fatty liver disease (NAFLD) patients[J]. J Clin Diagn Res, 2016, 10:7-10. [12] SUN YH, HUANG GY, ZHENG S, et al. Value of color Doppler ultrasonography in evaluating the vascular hemodynamic change of liver fibrois in infants with biliary atresia[J/CD]. Chin J Med Ultrasound:Electronic Edition, 2012, 9 (1) :29-35. (in Chinese) 孙颖华, 黄国英, 郑珊, 等.彩色多普勒超声检侧不同程度肝纤维化胆道闭锁婴儿肝内血流动力学变化的价值[J/CD].中华医学超声杂志:电子版, 2012, 9 (1) :29-35. [13] ERGELEN R, YILMAZ Y, ASEDOV R, et al. Comparison of Doppler ultrasound and transient elastography in the diagnosis of significant fibrosis in patients with nonalcoholic steatohepatitis[J]. Abdom Radiol (NY) , 2016, 41 (8) :1505-1510. [14] CAO JY, JIN Z. Advances in Contrast-enhanced Ultrasound Applied Research[J]. Clin J Med Offic, 2017, 45 (5) :441-448. (in Chinese) 曹军英, 金壮.超声造影应用研究进展[J].临床军医杂志, 2017, 45 (5) :441-448. 期刊类型引用(4)
1. 古秋梅,陈正举,陆方. 基于循证医学方法对眼底病专病生物样本库建设的分析与启示. 中华眼底病杂志. 2024(03): 215-221 .  百度学术
百度学术2. 张鑫,肖宇,钱开宇,夏彩霞,朱源. 抗凝血离心沉淀红细胞中残留基因组DNA的质量分析. 转化医学杂志. 2023(02): 80-85 .  百度学术
百度学术3. 王政禄,郑虹. 肝脏移植生物样本采集与保藏技术专家共识. 实用器官移植电子杂志. 2023(05): 385-392+384 .  百度学术
百度学术4. 陈凤秋,史文涛,徐晓菊,李江,仲生生,潘璐璐,张薛杰,蔡晓豪,沈慧青,汪雪玲,许锋. 项目导向的专病生物样本库质量评价体系的构建. 中国医药生物技术. 2022(06): 545-550 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 1614 KB)
PDF下载 ( 1614 KB)

 下载:
下载:


 百度学术
百度学术
 下载:
下载: