半肝阻断法和全肝阻断法在原发性肝癌肝切除术中应用效果比较的Meta分析
DOI: 10.3969/j.issn.1001-5256.2021.01.015
利益冲突声明:本研究不存在研究者以及与公开研究成果有关的利益冲突,特此声明。
作者贡献声明:刘莹、高本见负责课题设计,收集数据,资料分析,撰写论文;杨小李、方程、苏松参与修改论文;李波负责指导撰写文章并最后定稿。
Effect of hemihepatic vascular exclusion versus total hepatic vascular exclusion in hepatectomy for primary liver cancer: A Meta-analysis
-
摘要:
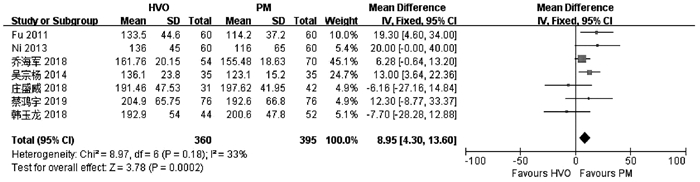
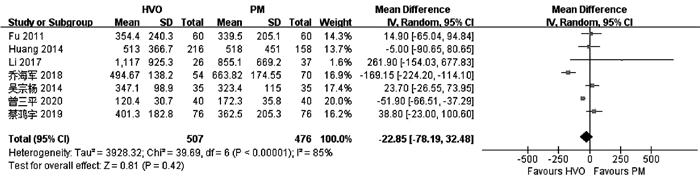
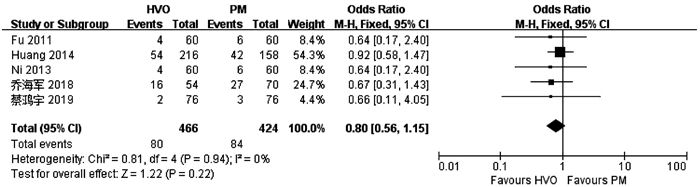
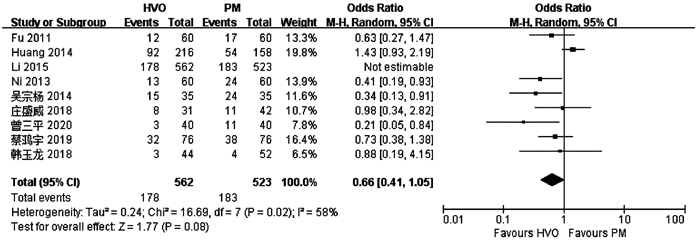
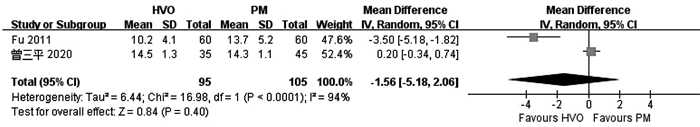
目的 比较普林格尔法(Pringle’s measure, PM)和半肝血管流入阻断法(HVO)在原发性肝癌肝切除术中的应用效果。 方法 计算机检索中、英文数据库中关于HVO和PM治疗原发性肝癌的对照研究,查找时间为数据库建立至2020年6月。对纳入的研究进行质量评价和数据提取后,采用RevMan5.3软件进行Meta分析。 结果 共纳入10项研究,合计1272例患者。HVO组术后第1、3天ALT水平低于PM组[均数差(MD)=-172.71,95%CI:-289.26~-56.16,P=0.004;MD=-130.35,95%CI:-221.25~-39.45,P=0.005],术后第3天AST水平低于PM组(MD=-84.56,95%CI:-166.47~-2.65,P=0.04),术后第1、3天Alb水平高于PM组(MD=1.31,95%CI:0.06~2.56,P=0.04;MD=1.81,95%CI:0.27~3.35,P=0.02),手术时间较PM组长(MD=8.95,95%CI:4.30~13.60;P<0.01)。 结论 HVO是一种安全有效的血流阻断方法,与PM相比能有效减轻肝损伤。但外科医生还应根据个人经验、患者病情以及术中具体情况选择适合患者的阻断方法。 -
关键词:
- 肝肿瘤 /
- 阻断治疗 /
- 肝切除术 /
- Meta分析(主题)
Abstract:Objective To systematically evaluate the effect of Pringle's measure (PM) versus hemihepatic vascular occlusion (HVO) in hepatectomy for primary liver cancer. Methods Related Chinese and English databases were searched for control studies on HVI versus PM in the treatment of primary liver cancer published up to June 2020. After quality evaluation and data extraction of the included studies, RevMan5.3 software was used for the meta-analysis. Results A total of 10 studies were included in the Meta-analysis, with 1272 patients in total. On days 1 and 3 after surgery, the HVO group had a significantly lower level of alanine aminotransferase than the PM group (day 1: mean difference [MD]=-172.71, 95% confidence interval [CI]: -289.26 to -56.16, P=0.004; day 3: MD=-130.35, 95%CI: -221.25 to -39.45, P=0.005). On day 3 after surgery, the HVO group had a significantly lower level of aspartate aminotransferase than the PM group (MD=-84.56, 95%CI: -166.47 to -2.65, P=0.04), and on days 1 and 3 after surgery, the HVO group had a significantly higher level of albumin than the PM group (day 1: MD=1.31, 95%CI: 0.06-2.56, P=0.04; day 3: MD=1.81, 95%CI: 0.27-3.35, P=0.02). The HVO group had a significantly longer time of operation than the PM group (MD=8.95, 95%CI: 4.30-13.60, P < 0.01). Conclusion HVO is a safe and effective method for vascular occlusion, and compared with PM, it can effectively alleviate liver injury. However, surgeons should select a suitable method for occlusion based on their own personal experience, patients' conditions, and specific situation during surgery. -
Key words:
- Liver Neoplasms /
- Therapeutic Occlusion /
- Hepatectomy /
- Meta-Analysis as Topic
-
表 1 纳入文献基本特征及质量评价
作者 年份 国家 研究类型 手术分组 样本量(例) 年龄(岁) 男/女(例) 肿瘤大小(cm) 质量评分(NOS/Jadad量表) Huang等[13] 2014 中国 RCS HVO 126 49.3±12.8 97/29 - 8 PM 158 48.5±12.0 129/29 - Li等[14] 2017 中国 RCS HVO 26 53(34~72)1) 20/6 - 8 PM 37 47.5(25~70)1) 33/4 - Ni等[15] 2013 中国 RCT HVO 60 56.1±9.3 47/13 4.7±2.2 3 PM 60 55.2±8.7 45/15 5.4±3.1 Fu等[16] 2011 中国 RCT HVO 60 49.3±9.2 41/19 6±2.8 3 PM 60 48.6±8.7 46/14 6.8±2.8 蔡鸿宇等[17] 2019 中国 RCT HVO 76 54.11±7.75 59/17 5.03±2.86 3 PM 76 53.24±7.83 56/20 5.77±3.74 曾三平[18] 2020 中国 RCT HVO 40 48.6±3.1 22/18 - 3 PM 40 48.8±3.0 23/17 - 韩玉龙等[19] 2018 中国 RCS HVO 44 - - 10.1±3.1 7 PM 52 - - 9.6±3.0 乔海军等[20] 2018 中国 RCS HVO 54 57.35±9.06 35/19 6.47±1.42 8 PM 70 56.94±8.72 46/24 6.51±1.38 吴宗杨等[21] 2014 中国 RCT HVO 35 - - - 3 PM 35 - - - 庄盛威等[22] 2018 中国 RCS HVO 31 49.62±4.91 24/7 9.07±0.99 8 PM 42 49.09±4.51 32/10 9.31±0.75 注:1)M(P最小值~P最大值);“-”表示未提及。 -
[1] BRUIX J, REIG M, SHERMAN M. Evidence-based diagnosis, staging, and treatment of patients with hepatocellular carcinoma[J]. Gastroenterology, 2016, 150(4): 835-853. DOI: 10.1053/j.gastro.2015.12.041 [2] TAN YH, SHANG YY, ZHANG T, et al. Current status and perspectives of multimodality therapy for hepatocellular carcinoma[J]. J Clin Hepatol, 2019, 35(8): 1858-1860. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2019.08.047谭运华, 商阳阳, 张涛, 等. 肝细胞癌综合治疗的现状和前景[J]. 临床肝胆病杂志, 2019, 35(8): 1858-1860. DOI: 10.3969/j.issn.1001-5256.2019.08.047 [3] KOOBY DA, STOCKMAN J, BEN-PORAT L, et al. Influence of transfusions on perioperative and long-term outcome in patients following hepatic resection for colorectal metastases[J]. Ann Surg, 2003, 237(6): 860-869; discussion 869-870. [4] TORZILLI G, MAKUUCHI M, INOUE K, et al. No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: Is there a way? A prospective analysis of our approach[J]. Arch Surg, 1999, 134(9): 984-992. DOI: 10.1001/archsurg.134.9.984 [5] PRINGLE JH. V. Notes on the arrest of hepatic hemorrhage due to trauma[J]. Ann Surg, 1908, 48(4): 541-549. DOI: 10.1097/00000658-190810000-00005 [6] TORZILLI G, PROCOPIO F, DONADON M, et al. Safety of intermittent Pringle maneuver cumulative time exceeding 120 minutes in liver resection: A further step in favor of the "radical but conservative" policy[J]. Ann Surg, 2012, 255(2): 270-280. DOI: 10.1097/SLA.0b013e318232b375 [7] GLANEMANN M, VOLLMAR B, NUSSLER AK, et al. Ischemic preconditioning protects from hepatic ischemia/reperfusion-injury by preservation of microcirculation and mitochondrial redox-state[J]. J Hepatol, 2003, 38(1): 59-66. DOI: 10.1016/S0168-8278(02)00327-6 [8] KUPIEC-WEGLINSKI JW, BUSUTTIL RW. Ischemia and reperfusion injury in liver transplantation[J]. Transpl Proc, 2005, 37(4): 1653-1656. DOI: 10.1016/j.transproceed.2005.03.134 [9] MAN K, FAN ST, NG IO, et al. Tolerance of the liver to intermittent pringle maneuver in hepatectomy for liver tumors[J]. Arch Surg, 1999, 134(5): 533-539. DOI: 10.1001/archsurg.134.5.533 [10] WU CC, HWANG CR, LIU TJ, et al. Effects and limitations of prolonged intermittent ischaemia for hepatic resection of the cirrhotic liver[J]. Br J Surg, 1996, 83(1): 121-124. DOI: 10.1002/bjs.1800830139 [11] BISMUTH H. Surgical anatomy and anatomical surgery of the liver[J]. World J Surg, 1982, 6(1): 3-9. DOI: 10.1007/BF01656368 [12] CLAUDIO L, BRENDON S, MARCO S, et al. Assessing the quality of studies in meta-analyses: Advantage and limitations of the Newcastie Ottawa Scale[J]. WJMA, 2017, 5(4): 80. DOI: 10.13105/wjma.v5.i4.80 [13] HUANG Z, ZHANG P, WANG H, et al. Comparing outcomes of two vascular inflow occlusion techniques and treatment without vascular occlusion during major hepatectomy in patients with hepatitis B-related hepatocellular carcinoma[J]. PLoS One, 2014, 9(9): e107303. DOI: 10.1371/journal.pone.0107303 [14] LI M, ZHANG T, WANG L, et al. Selective hemihepatic vascular occlusion versus pringle maneuver in hepatectomy for primary liver cancer[J]. Med Sci Monit, 2017, 23: 2203-2210. DOI: 10.12659/MSM.900859 [15] NI JS, LAU WY, YANG Y, et al. A prospective randomized controlled trial to compare pringle manoeuvre with hemi-hepatic vascular inflow occlusion in liver resection for hepatocellular carcinoma with cirrhosis[J]. J Gastrointest Surg, 2013, 17(8): 1414-1421. DOI: 10.1007/s11605-013-2236-z [16] FU SY, LAU WY, LI GG, et al. A prospective randomized controlled trial to compare Pringle maneuver, hemihepatic vascular inflow occlusion, and main portal vein inflow occlusion in partial hepatectomy[J]. Am J Surg, 2011, 201(1): 62-69. DOI: 10.1016/j.amjsurg.2009.09.029 [17] CAI HY, SHAO BF, ZHOU Y. Comparative observation of selective hemihepatic blood flow occlusion and Pringle blood flow occlusion in the surgical treatment of HBV-related liver cancer[J]. Shandong Med J, 2019, 59(6): 53-55. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY201906014.htm蔡鸿宇, 邵冰峰, 周元, 等. HBV相关性肝癌手术治疗中选择性半肝血流阻断与Pringle法血流阻断的应用对比观察[J]. 山东医药, 2019, 59(6): 53-55. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY201906014.htm [18] ZENG SP. Application effect comparison the first hepatic portal blood flow occlusion method and hemi-hepatic blood flow occlusion method in the treatment of primary hepatocellular carcinoma patients with hemi-hepatectomy[J]. Chin Mod Med, 2020, 27(3): 122-128. (in Chinese) DOI: 10.3969/j.issn.1674-4721.2020.03.036曾三平. 第一肝门血流阻断法与半肝血流阻断法在行半肝切除术治疗原发性肝癌患者中的应用效果比较[J]. 中国当代医药, 2020, 27(3): 122-128. DOI: 10.3969/j.issn.1674-4721.2020.03.036 [19] HAN YL, MIAO J, YIN JJ. Comparison of different hepatic inflow occlusion in hepatectomy in treatm ent of patients with primary large liver cancer[J]. J Prac Hepatol, 2018, 21(1): 104-107. (in Chinese) DOI: 10.3969/j.issn.1672-5069.2018.01.025韩玉龙, 苗健, 尹家俊. 不同肝血流阻断方案对手术切除原发性大肝癌患者治疗效果比较[J]. 实用肝脏病杂志, 2018, 21(1): 104-107. DOI: 10.3969/j.issn.1672-5069.2018.01.025 [20] QIAO HJ, SONG YC, ZHAO XY. Application of different blood flow occlusion methods of hepatectomy in the treatment of primary liver cancer[J]. J Hepatobiliary Surg, 2018, 26(4): 277-280. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-GDWZ201804012.htm乔海军, 宋玉成, 赵小勇. 肝癌切除术中不同血流阻断方式在原发性肝癌治疗中的应用[J]. 肝胆外科杂志, 2018, 26(4): 277-280. https://www.cnki.com.cn/Article/CJFDTOTAL-GDWZ201804012.htm [21] WU ZY, FENG JY, WANG JB, et al. Clinical study of Glisson pedicle transverse hepatectomy in the treatment of liver cancer[J]. J Hepatopancreatobiliary Surg, 2014, 26(4): 342-344. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-GDYW201404026.htm吴宗杨, 冯济业, 王金波, 等. Glisson蒂横断式肝切除术治疗肝癌的临床研究[J]. 肝胆胰外科杂志, 2014, 26(4): 342-344. https://www.cnki.com.cn/Article/CJFDTOTAL-GDYW201404026.htm [22] ZHUANG SW, LIN YY. Influence of different hepatic blood flow blocking methods on the curative effect of surgical resection of patients with primary massive liver cancer[J]. Chin Mod Doc, 2018, 56(29): 38-40. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS201829011.htm庄盛威, 林燕燕. 不同肝血流阻断方法对外科手术切除原发性大肝癌患者疗效的影响[J]. 中国现代医生, 2018, 56(29): 38-40. https://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS201829011.htm [23] ZHANG NP, ZHANG XJ. Evaluation of different hepatic blood flow blocking methods in laparoscopic hepatectomy of patients with liver cancer[J/CD]. Chin J Liver Dis (Electronic Version), 2019, 11(3): 58-63. (in Chinese)张能平, 张雄杰. 不同肝血流阻断方式在肝癌患者腹腔镜肝切除术中的应用[J/CD]. 中国肝脏病杂志(电子版), 2019, 11(3): 58-63. [24] ZHU P, LAU WY, CHEN YF, et al. Randomized clinical trial comparing infrahepatic inferior vena cava clamping with low central venous pressure in complex liver resections involving the Pringle manoeuvre[J]. Br J Surg, 2012, 99(6): 781-788. DOI: 10.1002/bjs.8714 [25] SELZNER N, RUDIGER H, GRAF R, et al. Protective strategies against ischemic injury of the liver[J]. Gastroenterology, 2003, 125(3): 917-936. DOI: 10.1016/S0016-5085(03)01048-5 [26] GRACE PA. Ischaemia-reperfusion injury[J]. Br J Surg, 1994, 81(5): 637-647. DOI: 10.1002/bjs.1800810504 [27] XIAOBIN F, ZIPEI L, SHUGUO Z, et al. The Pringle manoeuvre should be avoided in hepatectomy for cancer patients due to its side effects on tumor recurrence and worse prognosis[J]. Med Hypotheses, 2009, 72(4): 398-401. [28] BELGHITI J, NOUN R, MALAFOSSE R, et al. Continuous versus intermittent portal triad clamping for liver resection: A controlled study[J]. Ann Surg, 1999, 229(3): 369-375. [29] GUO T, XIAO Y, LIU Z, et al. The impact of intraoperative vascular occlusion during liver surgery on postoperative peak ALT levels: A systematic review and meta-analysis[J]. Int J Surg, 2016, 27: 99-104. [30] WANG HQ, YANG JY, YAN LN. Hemihepatic versus total hepatic inflow occlusion during hepatectomy: A systematic review and meta-analysis[J]. World J Gastroenterol, 2011, 17(26): 3158-3164. [31] DING HY, TAI QW, ZHOU CM, et al. Hemihepatic inflow occlusion versus total hepatic inflow occlusion in liver resection: A meta-analysis[J]. Chin J Evid-based Med, 2014, 14(4): 469-477. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZZXZ201404019.htm丁贺义, 邰沁文, 周成明, 等. 肝切除术应用半肝与全肝入肝血流阻断法效果的Meta分析[J]. 中国循证医学杂志, 2014, 14(4): 469-477 https://www.cnki.com.cn/Article/CJFDTOTAL-ZZXZ201404019.htm [32] RAHBARI NN, KOCH M, MEHRABI A, et al. Portal triad clamping versus vascular exclusion for vascular control during hepatic resection: A systematic review and meta-analysis[J]. J Gastrointest Surg, 2009, 13(3): 558-568. -



 PDF下载 ( 3827 KB)
PDF下载 ( 3827 KB)


 下载:
下载: