腹腔镜、胆道镜及十二指肠镜联合免T管引流对胆囊结石合并胆总管结石的治疗效果分析
DOI: 10.3969/j.issn.1001-5256.2021.04.029
Clinical effect of laparoscopy, choledochoscopy, and duodenoscopy combined with T-tube-free drainage in treatment of gallstones with common bile duct stones
-
摘要:
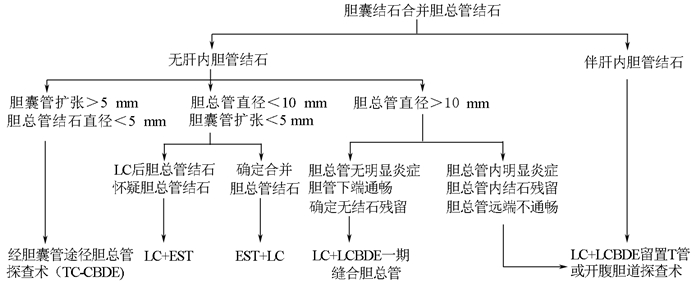
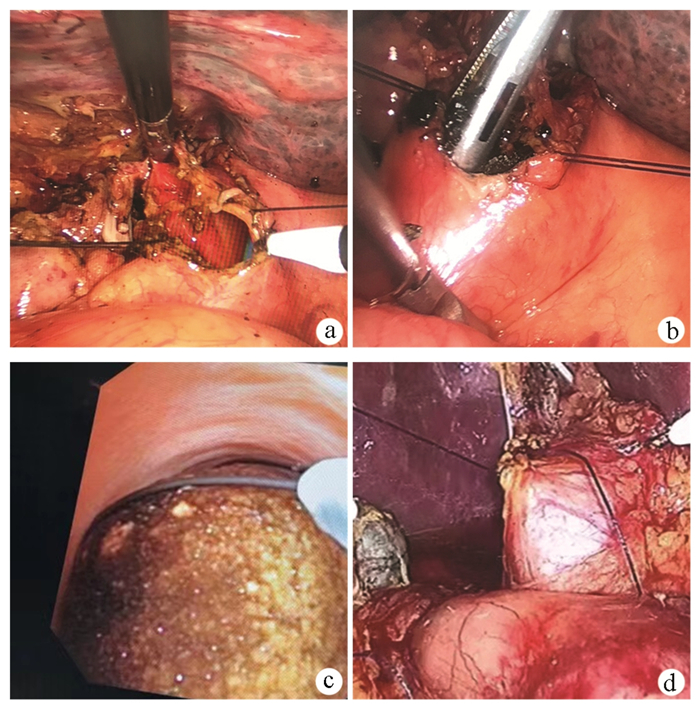
目的 探讨腹腔镜、胆道镜及十二指肠镜联合免T管引流对胆囊结石合并胆总管结石的治疗效果。 方法 选取2017年12月—2019年12月上海市健康医学院附属浦东新区人民医院普外科收治的胆囊结石合并胆管结石患者564例,根据手术方式分为腹腔镜经胆囊管胆道探查术(LTCBDE)组191例;三镜联合腹腔镜胆总管切开取石一期缝合术(LBEPS)组138例;十二指肠镜逆行胰胆管造影术(ERCP)+内镜乳头括约肌切开取石术(EST)/乳头柱状球囊扩张术(EPBD)+腹腔镜胆囊切除术(LC)组235例。统计3组患者性别、年龄、胆管直径、结石大小/数量等一般资料,比较手术及并发症情况。正态分布的计量资料组间比较采用单因素方差分析;非正态数据的计量资料组间比较采用Kruskal-Wallis H检验;计数资料组间比较采用χ2检验。 结果 LTCBDE组、LBEPS组、ERCP+EST/EPBD+LC组3组间住院费用、引流量、排气时间、住院时间、引流管拔除时间,差异均有统计学意义(F值分别为416.40、7.799、33.99、143.70、13.08,P值分别为 < 0.001、0.020、 < 0.001、 < 0.001、 < 0.001),且LTCBDE组较其他2组住院费用更低、排气时间更早、住院时间更短、引流管拔除时间更短(P值均 < 0.05)。3组术后均未见严重并发症,并发症发生率差异无统计学意义(P>0.05)。所有患者术后均顺利出院。 结论 3种微创方式联合免T管引流治疗肝外胆管结石均达到了创伤小、痛苦小、术后恢复快、无严重并发症的目标,其中LTCBDE组治疗费用最低及术后恢复效果最佳。 -
关键词:
- 胆囊结石病 /
- 胆总管结石 /
- 胰胆管造影术, 内窥镜逆行 /
- 胆囊切除术, 腹腔镜 /
- 十二指肠镜检查 /
- 引流术
Abstract:Objective To investigate the clinical effect of laparoscopy, choledochoscopy, and duodenoscopy combined with T-tube-free drainage in the treatment of gallstones with common bile duct stones. Methods A retrospective analysis was performed for the clinical data of 564 patients with gallstones and common bile duct stones who were admitted to Department of General Surgery, Pudong New Area People's Hospital, Shanghai University of Medicine & Health Sciences, from December 2017 to December 2019. According to the surgical procedure, the patients were divided into laparoscopic transcystic common bile duct exploration (LTCBDE) group with 191 patients, three endoscopies+laparoscopic common bile duct exploration and primary suture (LBEPS) group with 138 patients, and endoscopic retrograde cholangiopancreatography (ERCP)+endoscopic sphincterotomy (EST)/endoscopic papillary balloon dilation (EPBD)+laparoscopic cholecystectomy (LC) group with 235 patients. The three groups were analyzed in terms of the general data including sex, age, bile duct diameter, and stone size/number, and surgical condition and complications were compared between groups. A one-way analysis of variance was used for comparison of normally distributed continuous data between groups, and the Kruskal-Wallis H test was used for comparison of non-normally distributed continuous data between groups; the chi-square test was used for comparison of categorical data between groups. Results There were significant differences between the LBEPS group, the ERCP+EST/EPBD+LC group and the LTCBDE group in hospital costs, drainage volume, time to first flatus, length of hospital stay and time to extraction of drainage tube (F=416.40, 7.80, 33.99, 143.70, and 13.08, P < 0.001, P=0.020, P < 0.001, P < 0.001, and P < 0.001). Compared with the LBEPS group and ERCP+EST/EPBD+LC groups, the LTCBDE group had significantly lower hospital costs and a significantly longer time to first flatus, and significantly shorter length of hospital stay and time to extraction of drainage tube(all P < 0.05). No serious complication was observed after surgery, and there was no significant difference in the incidence rate of complications between the three groups (P>0.05). All patients were discharged successfully after surgery. Conclusion The three minimally invasive surgical procedures combined with T-tube-free drainage achieve the goal of little trauma and pain, fast postoperative recovery, and few serious complications, among which LTCBDE has the lowest treatment costs and the best postoperative recovery. -
表 1 3组患者一般资料及手术情况比较
项目 合计(n=564) LTCBDE组(n=191) LBEPS组(n=138) ERCP+EST/EPBD+LC组(n=235) 统计值 P值 年龄(岁) 62.55±12.22 64.30±12.50 65.78±14.03 66.03±13.00 F=1.834 0.180 性别[例(%)] χ2=1.150 0.562 男 266(47.2) 96 (50.3) 62(44.9) 108(46.0) 女 298(52.8) 95 (49.7) 76(55.1) 127(54.0) 手术成功[例(%)] 560(99.2) 175(91.6) 134(97.1) 217(92.3) χ2=0.154 0.931 术前TBil(mmol/L) 19.9±7.8 18.9±3.1 21.2±4.6 20.1±3.7 F=0.896 0.639 病程(月) 21.2±4.3 19.4±5.5 21.5±5.9 22.5±6.2 F=0.920 0.631 胆总管直径(mm) 8.96±3.46 9.03±3.14 8.98±3.09 8.93±3.65 F=3.150 0.207 结石数量(个) 2.2±0.5 2.2±0.5 2.2±0.6 1.8±0.5 F=2.161 0.339 结石大小(mm) 8.38±2.89 7.18±1.60 8.76±3.34 8.42±3.19 F=3.015 0.221 手术情况 手术时间(min) 92.2±15.7 92.4±14.7 90.2±15.1 93.2±16.6 F=2.052 0.358 住院费用(万元) 3.0±0.4 2.1±0.6 3.1±0.7 3.6±0.5 F=416.400 < 0.001 24 h引流量(ml) 37±13 39±13 37±16 36±12 F=7.799 0.020 排气时间(d) 2.1±0.6 1.9±0.5 2.1±0.7 2.2±0.5 F=33.990 < 0.001 拔引流管时间(d) 2.3±0.5 2.1±0.5 2.3±0.5 2.4±0.5 F=13.080 0.001 住院时间(d) 2.8±0.7 2.3±0.4 2.7±0.6 3.2±0.7 F=143.700 < 0.001 并发症[例(%)] 胆漏 3(0.5) 1(0.5) 2 (1.4) 0 χ2=3.067 0.115 胰腺炎 4(0.7) 0 0 4(1.7) χ2=3.891 0.090 结石残留 1(0.2) 1(0.5) 0 0 χ2=1.853 0.584 切口感染 3(0.5) 1(0.5) 1(0.7) 1(0.4) χ2=0.639 >0.05 出血 6(1.1) 3(1.5) 3(2.2) 0 χ2=5.000 0.056 胆管炎 2(0.4) 0 0 2(0.9) χ2=1.800 0.512 穿孔 0 0 0 0 死亡 0 0 0 0 -
[1] LIU XJ, HE XZ. Clinical analysis of residual choledocholithiasis after laparoscopic cholecystectomy[J]. J Hepatopancreatobiliary Surg, 2019, 31(9): 566-568. DOI: 10.11952/j.issn.1007-1954.2019.09.013.刘小健, 何信众. 腹腔镜胆囊切除术后胆总管残留结石的临床分析[J]. 肝胆胰外科杂志, 2019, 31(9): 566-568. DOI: 10.11952/j.issn.1007-1954.2019.09.013. [2] PAN L, CHEN M, JI L, et al. The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: An up-to-date Meta-analysis[J]. Ann Surg, 2018, 268(2): 247-253. DOI: 10.1097/SLA.0000000000002731. [3] AHN DW, LEE SH, PAIK WH, et al. Effects of saline irrigation of the bile duct to reduce the rate of residual common bile duct stones: A multicenter, prospective, randomized study[J]. Am J Gastroenterol, 2018, 113(4): 548-555. DOI: 10.1038/ajg.2018.21. [4] SUN XD, QIU W, LYU GY, et al. Clinical efficacy of combined three-endoscopic minimally invasive surgical treatment of extrahepatic cholangiolithiasis in 2364 patient[J]. Chin J Dig Surg, 2016, 15(4): 357-362. DOI: 10.3760/cma.j.issn.1673-9752.2016.04.010.孙晓东, 邱伟, 吕国悦, 等. 2364例肝外胆管结石三镜联合微创外科治疗的临床疗效[J]. 中华消化外科杂志, 2016, 15(4): 357-362. DOI: 10.3760/cma.j.issn.1673-9752.2016.04.010. [5] ZHANG LH, TAO LD, ZENG J, et al. Combined treatment of choledocholithiasis with cholecystolithiasis Oddi sphincter function[J]. Chin J Gen Surg, 2019, 34(11): 994-995. DOI: 10.3670.cma.j.issn.1007-631X.2019.11.025.张立洪, 陶立德, 曾佳, 等. 保护Oddi括约肌功能的三镜联合治疗胆总管结石合并胆囊结石[J]. 中华普通外科杂志, 2019, 34(11): 994-995. DOI: 10.3670.cma.j.issn.1007-631X.2019.11.025. [6] WANG AQ, YI SN, LIU JH. Application of three-mirror combined with transabdominal drainage of nasal bile duct in elderly patients with extrahepatic cholelithiasis[J]. J Hepatopancreatobiliary Surg, 2018, 30(6): 485-488. DOI: 10.11952/j.issn.1007-1954.2018.06.010.王安琪, 尹思能, 刘进衡. 三镜联合经腹置入鼻胆管引流在老年肝外胆管结石中的应用[J]. 肝胆胰外科杂志, 2018, 30(6): 485-488. DOI: 10.11952/j.issn.1007-1954.2018.06.010. [7] WANG YF, WANG AL, LI Z, et al. Laparoscopic transcystic common bile duct exploration and laparoscopic transductal common bile duct exploration in elderly patients with cholecystolithiasis combined with choledocholithiasis[J]. Chin Med J (Engl), 2019, 132(14): 1745-1746. DOI: 10.1097/CM9.0000000000000323. [8] CZERWONKO ME, PEKOLJ J, UAD P, et al. Laparoscopic transcystic common bile duct exploration in the emergency is as effective and safe as in elective setting[J]. J Gastrointest Surg, 2019, 23(9): 1848-1855. DOI: 10.1007/s11605-018-4029-x. [9] ZHU JG, WU S, FENG Q, et al. Protocol for the CREST Choles (Chinese REgistry Study on Treatment of Cholecysto-Choledocholithiasis) study: An ambispective, multicenter, observational, open-cohort study[J]. BMJ Open, 2019, 9(11): e030293. DOI: 10.1136/bmjopen-2019-030293. [10] FU Y, KONG J, WANG D, et al. Cholelithiasis and choledocholithiasis in a 78-day-old infant suffering from jaundice, and treated through laparoscopic transcystic common bile duct exploration (LTCBDE)[J]. Asian J Surg, 2019, 42(10): 930-931. DOI: 10.1016/j.asjsur.2019.05.013. [11] PANG L, ZHANG Y, WANG Y, et al. Transcystic versus traditional laparoscopic common bile duct exploration: Its advantages and a meta-analysis[J]. Surg Endosc, 2018, 32(11): 4363-4376. DOI: 10.1007/s00464-018-6286-x. [12] WENG HQ, JIANG JL, SUN HW, et al. Feasibility study of laparoscopic choledocholithotomy for primary suture[J]. Chin J Gen Surg, 2015, 30(10): 819-820. DOI: 10.3760/cma.j.issn.1007-631X.2015.10.022.翁汉钦, 蒋基令, 孙宏武, 等. 腹腔镜下胆管测压胆总管一期缝合的可行性研究[J]. 中国普通外科杂志, 2015, 30(10): 819-820. DOI: 10.3760/cma.j.issn.1007-631X.2015.10.022. [13] LEONG HY, CHANG YK, OOI CW, et al. Liquid biphasic electric partitioning system as a novel integration process for betacyanins extraction from red-purple pitaya and antioxidant properties assessment[J]. Front Chem, 2019, 7: 201. DOI: 10.3389/fchem.2019.00201. [14] COHEN J, PLESKOW D. The long road to stone management in the bile duct - what else to wish?[J]. Endoscopy, 2019, 51(10): 907-908. DOI: 10.1055/a-0982-3278. [15] WEN ZQ, SONG Y, ZHANG YM, et al. Clinical application of laparoscopy combined with choledochoscopy and duodenoscopy in treatment of gallstones complicated by intra-and extrahepatic bile duct stones[J]. J Clin Hepatol, 2016, 32(6): 1145-1148. DOI: 10.3969/j.issn.1001-5256.2016.06.025.温治强, 宋越, 张耀明, 等. 腹腔镜联合胆道镜、十二指肠镜治疗胆囊结石合并肝内外胆管结石的效果观察[J]. 临床肝胆病杂志, 2016, 32(6): 1145-1148. DOI: 10.3969/j.issn.1001-5256.2016.06.025. [16] WANG J, CHEN W. Treatment strategies of complicated extrahepatic bileduct stones[J]. Chin J Dig Surg, 2019, 18(12): 1113-1117. DOI: 10.3760/cma.j.issn.1673-9752.2019.12.005.王坚, 陈炜. 复杂肝外胆管结石的治疗策略[J]. 中华消化外科杂志, 2019, 18(12): 1113-1117. DOI: 10.3760/cma.j.issn.1673-9752.2019.12.005. -



 PDF下载 ( 2486 KB)
PDF下载 ( 2486 KB)

 下载:
下载: