基于升阶梯治疗原则分析重症急性胰腺炎患者行开腹坏死物清除术的危险因素
DOI: 10.3969/j.issn.1001-5256.2021.04.033
Risk factors for open pancreatic necrosectomy in patients with severe acute pancreatitis: An analysis based on the surgical step-up approach
-
摘要:
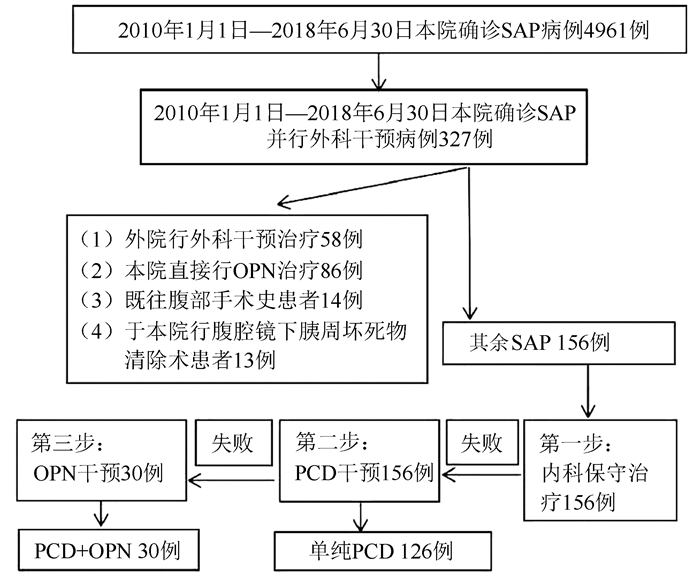
目的 开腹坏死物清除术(OPN)是单纯经皮穿刺置管引流(PCD)失败后治疗重症急性胰腺炎(SAP)的有效方式,探讨导致患者需要继续行OPN的危险因素。 方法 选取2010年1月1日—2018年6月30日于遵义医科大学附属医院行基于“step-up”原则外科干预方式的SAP患者156例,根据后期是否行OPN分为PCD组(n=126)和PCD+OPN组(n=30)。收集患者年龄、性别、病因、入院血钙、入院白细胞、CTSI评分>7分、APACHE-Ⅱ评分、Ronson评分、是否合并胰周液体积聚、是否合并感染、是否合并多器官功能衰竭(MOF)、PCD干预时间是否超过入院后1周等临床资料。计量资料两组间比较采用t检验;计数资料两组间比较采用χ2检验。采用多因素logistic回归分析确定后期行OPN的独立预测因子。 结果 SAP患者后期需要行OPN的概率为19.2%。PCD组与PCD+OPN组相比,入院时合并MOF所占比例更少[34(27.0%) vs 21(70.0%),χ2=19.642, P < 0.01];PCD干预时间 < 1周所占比例更高[78(61.9%) vs 6(20.0%),χ2=17.121, P < 0.01]。入院时合并MOF、入院后首次PCD干预时间>1周、入院时合并感染[OR(95%CI)分别为5.343(1.832~15.583)、5.518(1.742~17.477)、5.016(1.322~19.378),P值均 < 0.05]是SAP患者后期需要行OPN的独立危险因素。 结论 SAP入院时合并MOF、入院后初次PCD干预时间>1周和入院时合并感染是基于“step-up”原则下的SAP患者早期行PCD治疗后需要继续行OPN的独立危险因素,在临床实践中及时识别相关危险因素有利于把握OPN的时机以改善SAP患者的临床预后。 Abstract:Objective To investigate the risk factors for open pancreatic necrosectomy (OPN), an effective treatment method for severe acute pancreatitis (SAP) after the failure of percutaneous catheter drainage (PCD), in patients with SAP. Methods A retrospective analysis was performed for 156 patients with SAP who underwent surgical intervention based on the step-up approach in The Affiliated Hospital of Zunyi Medical University from January 1, 2010 to June 30, 2018, and according to whether OPN was performed, the patients were divided into PCD group with 126 patients and PCD+OPN group with 30 patients. Related clinical data were collected, including age, sex, etiology, blood calcium on admission, white blood cell count on admission, whether CTSI score was >7, APACHE-Ⅱ score, Ranson score, presence or absence of peripancreatic fluid accumulation, presence or absence of infection, presence or absence of multiple organ failure (MOF), and whether PCD was performed at more than 1 week after admission. The t-test was used for comparison of continuous data between groups, and the chi-square test was used for comparison of categorical data between groups; a multivariate logistic regression analysis was used to determine the independent predictive factors for OPN. Results The probability of OPN was 19.2% for SAP patients in the later stage. Compared with the PCD+OPN group, the PCD group had a significantly lower proportion of patients with MOF on admission [27.0% (34/126) vs 70.0% (21/30), χ2=19.642, P < 0.01] and a significantly higher proportion of patients undergoing PCD at less than 1 week after admission [61.9% (78/126) vs 20.0% (6/30), χ2=17.121, P < 0.01]. MOF on admission (odds ratio [OR]=5.343, 95% confidence interval [CI]: 1.832-15.583, P < 0.05), initial PCD performed at more than 1 week after admission (OR= 5.518, 95% CI: 1.742-17.477, P < 0.05), and infection on admission (OR=5.016, 95% CI: 1.322-19.378, P < 0.05) were independent risk factors for subsequent OPN in SAP patients. Conclusion SAP with MOF on admission, initial PCD performed at more than 1 week after admission, and SAP with infection on admission are independent risk factors for subsequent OPN in SAP patients undergoing PCD in the early stage based on the step-up approach. Timely identification of related risk factors helps to grasp the timing of OPN in clinical practice and improve the clinical prognosis of SAP patients. -
Key words:
- Pancreatitis /
- Risk Factors /
- Step-up Surgery
-
表 1 SAP行OPN单因素分析
因素 单纯PCD组(n=126) PCD+OPN组(n=30) 统计值 P值 年龄(岁) 47±14 45±18 t=-0.074 0.941 性别[例(%)] 男 75(59.5) 15(50.0) χ2=0.900 0.343 女 51(40.5) 15(50.0) 病因[例(%)] χ2=0.535 0.911 胆源性 32(25.4) 6(20.0) 高脂性 48(38.1) 12(40.0) 酒精性 14(11.1) 3(10.0) 其他 32(25.4) 9(30.0) 入院合并MOF[例(%)] 34(27.0) 21(70.0) χ2=19.642 0.001 CTSI评分≥7分[例(%)] 47(37.3) 17(56.7) χ2=3.756 0.053 入院血钙(mmol/L) 1.93±0.33 1.82±0.26 t=-1.930 0.054 入院白细胞(×109/L) 13.06±6.42 13.19±5.48 t=-0.418 0.674 APACHE-Ⅱ评分(分) 10.85±1.92 11.00±1.46 t=-0.677 0.498 Ronson评分(分) 4.18±0.85 4.10±0.80 t=-0.299 0.765 胰周液体积聚[例(%)] 86(68.3) 24(80.0) χ2=1.608 0.205 合并感染[例(%)] 16(12.7) 7(23.3) χ2=2.180 0.140 入院1周内行PCD[例(%)] 78(61.9) 6(20.0) χ2=17.121 0.001 表 2 SAP行OPN多因素logistic回归分析
变量 B值 SE Wald df P值 OR 95%CI 外科干预前合并MOF 1.676 0.546 9.418 1 0.002 5.343 1.832~15.583 入院超过1周行PCD 1.708 0.588 8.433 1 0.004 5.518 1.742~17.477 合并感染 1.622 0.685 5.603 1 0.018 5.061 1.322~19.378 -
[1] PORTELLI M, JONES CD. Severe acute pancreatitis: Pathogenesis, diagnosis and surgical management[J]. Hepatobiliary Pancreat Dis Int, 2017, 16(2): 155-159. DOI: 10.1016/s1499-3872(16)60163-7. [2] GUO Q, LI A, XIA Q, et al. The role of organ failure and infection in necrotizing pancreatitis: A prospective study[J]. Ann Surg, 2014, 259(6): 1201-1207. DOI: 10.1097/SLA.0000000000000264. [3] PETROV MS, WINDSOR JA. Classification of the severity of acute pancreatitis: How many categories make sense?[J]. Am J Gastroenterol, 2010, 105(1): 74-76. DOI: 10.1038/ajg.2009.597. [4] BRADLEY EL 3rd, DEXTER ND. Management of severe acute pancreatitis: A surgical odyssey[J]. Ann Surg, 2010, 251(1): 6-17. DOI: 10.1097/SLA.0b013e3181c72b79. [5] VAN SANTVOORT HC, BESSELINK MG, BAKKER OJ, et al. A step-up approach or open necrosectomy for necrotizing pancreatitis[J]. N Engl J Med, 2010, 362(16): 1491-1502. DOI: 10.1056/NEJMoa0908821. [6] HOLLEMANS RA, BAKKER OJ, BOERMEESTER MA, et al. Superiority of step-up approach vs open necrosectomy in long-term follow-up of patients with necrotizing pancreatitis[J]. Gastroenterology, 2019, 156(4): 1016-1026. DOI: 10.1053/j.gastro.2018.10.045. [7] UHL W. Systematic review of percutaneous catheter drainage as primary treatment for necrotizing pancreatitis (Br J Surg 2011; 98: 18-27)[J]. Br J Surg, 2011, 98(1): 27-28. DOI: 10.1002/bjs.7309. [8] SUN B, JI L. Concerns relating the surgical management of severe acute pancreatitis[J]. Chin J Dig Surg, 2017, 16(10): 987-990. DOI: 10.3760/cma.j.issn.1673-9752.2017.10.003.孙备, 冀亮. 重症急性胰腺炎外科干预应重视的问题[J]. 中华消化外科杂志, 2017, 16(10): 987-990. DOI: 10.3760/cma.j.issn.1673-9752.2017.10.003. [9] BELLAM BL, SAMANTA J, GUPTA P, et al. Predictors of outcome of percutaneous catheter drainage in patients with acute pancreatitis having acute fluid collection and development of a predictive model[J]. Pancreatology, 2019, 19(5): 658-664. DOI: 10.1016/j.pan.2019.05.467. [10] GUO Q, LI A, HU W. Predictive factors for successful ultrasound-guided percutaneous drainage in necrotizing pancreatitis[J]. Surg Endosc, 2016, 30(7): 2929-2934. DOI: 10.1007/s00464-015-4579-x. [11] Pancreas Study Group, Chinese Society of Gastroenterology, Chinese Medical Association; Editorial Board of Chinese Journal of Pancreatology; Editorial Board of Chinese Journal of Digestion. Chinese guidelines for the management of acute pancreatitis (Shenyang, 2019)[J]. J Clin Hepatol, 2019, 35(12): 2706 -2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013.中华医学会消化病学分会胰腺疾病学组, 中华胰腺病杂志编辑委员会, 中华消化杂志编辑委员会. 中国急性胰腺炎诊治指南(2019年, 沈阳)[J]. 临床肝胆病杂志, 2019, 35(12): 2706-2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013. [12] LEI RQ, ZHANG SD. Significance of systemic inflammatory response in the pathogenesis of acute pancreatitis[J]. Chin J Hepatobiliary Surg, 2000, 6(1): 76. DOI: 10.3760/cma.j.issn.1007-8118.2000.01.033.雷若庆, 张圣道. 全身炎症反应在急性胰腺炎发病机理中的意义[J]. 中华肝胆外科杂志, 2000, 6(1): 76. DOI: 10.3760/cma.j.issn.1007-8118.2000.01.033. [13] van BAAL MC, van SANTVOORT HC, BOLLEN TL, et al. Systematic review of percutaneous catheter drainage as primary treatment for necrotizing pancreatitis[J]. Br J Surg, 2011, 98(1): 18-27. DOI: 10.1002/bjs.7304. [14] SUN B, LI GQ. Surgical intervention strategies for local complications of severe acute pancreatitis[J]. Chin J Dig Surg, 2020, 19(4): 379-383. DOI: 10.3760/ cma.j.cn115610-20200121-00040.孙备, 李冠群. 重症急性胰腺炎局部并发症外科干预策略[J]. 中华消化外科杂志, 2020, 19(4): 379-383. DOI: 10.3760/ cma.j.cn115610-20200121-00040. [15] BANKS PA, FREEMAN ML, Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis[J]. Am J Gastroenterol, 2006, 101(10): 2379-2400. DOI: 10.1111/j.1572-0241.2006.00856.x. [16] SHI N, LIU T, de la IGLESIA-GARCIA D, et al. Duration of organ failure impacts mortality in acute pancreatitis[J]. Gut, 2020, 69(3): 604-605. DOI: 10.1136/gutjnl-2019-318241. [17] ROCHA FG, BENOIT E, ZINNER MJ, et al. Impact of radiologic intervention on mortality in necrotizing pancreatitis: The role of organ failure[J]. Arch Surg, 2009, 144(3): 261-265. DOI: 10.1001/archsurg.2008.587. [18] SCHEPERS NJ, BAKKER OJ, BESSELINK MG, et al. Impact of characteristics of organ failure and infected necrosis on mortality in necrotising pancreatitis[J]. Gut, 2019, 68(6): 1044-1051. DOI: 10.1136/gutjnl-2017-314657. [19] TENNER S, BAILLIE J, DEWITT J, et al. American College of Gastroenterology guideline: Management of acute pancreatitis[J]. Am J Gastroenterol, 2013, 108(9): 1400-1415. DOI: 10.1038/ajg.2013.218. [20] BABU RY, GUPTA R, KANG M, et al. Predictors of surgery in patients with severe acute pancreatitis managed by the step-up approach[J]. Ann Surg, 2013, 257(4): 737-750. DOI: 10.1097/SLA.0b013e318269d25d. [21] JI L, WANG G, LI L, et al. Risk factors for the need of surgical necrosectomy after percutaneous catheter drainage in the management of infection secondary to necrotizing pancreatitis[J]. Pancreas, 2018, 47(4): 436-443. DOI: 10.1097/MPA.0000000000001031. [22] Italian Association for the Study of the Pancreas (AISP), PEZZILLI R, ZERBI A, et al. Consensus guidelines on severe acute pancreatitis[J]. Dig Liver Dis, 2015, 47(7): 532-543. DOI: 10.1016/j.dld.2015.03.022. [23] van GRINSVEN J, van SANTVOORT HC, BOERMEESTER MA, et al. Timing of catheter drainage in infected necrotizing pancreatitis[J]. Nat Rev Gastroenterol Hepatol, 2016, 13(5): 306-312. DOI: 10.1038/nrgastro.2016.23. [24] WANG YZ, ZHANG L, QIN T, et al. The individualized treatment of the severe acute pancreatitis[J]. Chin J Gen Surg, 2011, 20(3): 312-313. https://www.cnki.com.cn/Article/CJFDTOTAL-ZPWZ201103036.htm王玉柱, 张莉, 秦涛, 等. 重症急性胰腺炎的个体化诊治体会[J]. 中国普通外科杂志, 2011, 20(3): 312-313. https://www.cnki.com.cn/Article/CJFDTOTAL-ZPWZ201103036.htm [25] ZHENG Q, LIU JS. Minimally invasive intervention strategy for severe acute pancreatitis[J]. J Clin Hepatol, 2020, 36(8): 1909-1912. DOI: 10.3969/j.issn.1001-5256.2020.08.051.郑琦, 刘建生. 重症急性胰腺炎的微创干预策略[J]. 临床肝胆病杂志, 2020, 36(8): 1909-1912. DOI: 10.3969/j.issn.1001-5256.2020.08.051. [26] AI X, QIAN X, PAN W, et al. Ultrasound-guided percutaneous drainage may decrease the mortality of severe acute pancreatitis[J]. J Gastroenterol, 2010, 45(1): 77-85. DOI: 10.1007/s00535-009-0129-4. [27] SMIT M, BUDDINGH KT, BOSMA B, et al. Abdominal compartment syndrome and intra-abdominal ischemia in patients with severe acute pancreatitis[J]. World J Surg, 2016, 40(6): 1454-1461. DOI: 10.1007/s00268-015-3388-7. [28] TIAN H, LI FX, SONG SW. Features of infection secondary to severe acute pancreatitis and related control strategies[J]. J Clin Hepatol, 2019, 35(2): 451-456. DOI: 10.3969/j.issn.1001-5256.2019.02.048.田浩, 李富兴, 宋少伟. 重症急性胰腺炎继发感染的特点及防治进展[J]. 临床肝胆病杂志, 2019, 35(2): 451-456. DOI: 10.3969/j.issn.1001-5256.2019.02.048. [29] BOSSCHA K, HULSTAERT PF, HENNIPMAN A, et al. Fulminant acute pancreatitis and infected necrosis: Results of open management of the abdomen and "planned" reoperations[J]. J Am Coll Surg, 1998, 187(3): 255-262. DOI: 10.1016/s1072-7515(98)00153-7. [30] Group of Pancreas Surgery, Chinese Society of Surgery, Chinese Medical Association. Guidelines for the management of acute pancreatitis(2014)[J]. J Clin Hepatol, 2015, 31(1): 17-20. DOI: 10.3969/j.issn.1001-5256.2015.01.004.中华医学会外科学分会胰腺外科学组. 急性胰腺炎诊治指南(2014)[J]. 临床肝胆病杂志, 2015, 31(1): 17-20. DOI: 10.3969/j.issn.1001-5256.2015.01.004. [31] SORRENTINO L, CHIARA O, MUTIGNANI M, et al. Combined totally mini-invasive approach in necrotizing pancreatitis: A case report and systematic literature review[J]. World J Emerg Surg, 2017, 12: 16. DOI: 10.1186/s13017-017-0126-5. [32] ZHANG H, CHEN GY, XIAO L, et al. Ultrasonic/CT image fusion guidance facilitating percutaneous catheter drainage in treatment of acute pancreatitis complicated with infected walled-off necrosis[J]. Pancreatology, 2018, 18(6): 635-641. DOI: 10.1016/j.pan.2018.06.004. [33] YOKOI Y, KIKUYAMA M, KUROKAMI T, et al. Early dual drainage combining transpapillary endotherapy and percutaneous catheter drainage in patients with pancreatic fistula associated with severe acute pancreatitis[J]. Pancreatology, 2016, 16(4): 497-507. DOI: 10.1016/j.pan.2016.03.007. -



 PDF下载 ( 2166 KB)
PDF下载 ( 2166 KB)

 下载:
下载:


