MELD评分联合血小板/白细胞比值对HBV相关慢加急性肝衰竭患者预后的预测价值
DOI: 10.3969/j.issn.1001-5256.2021.05.019
Value of Model for End-Stage Liver Disease score combined with platelet-to-white blood cell ratio in predicting the prognosis of patients with hepatitis B virus-associated acute-on-chronic liver failure
-
摘要:
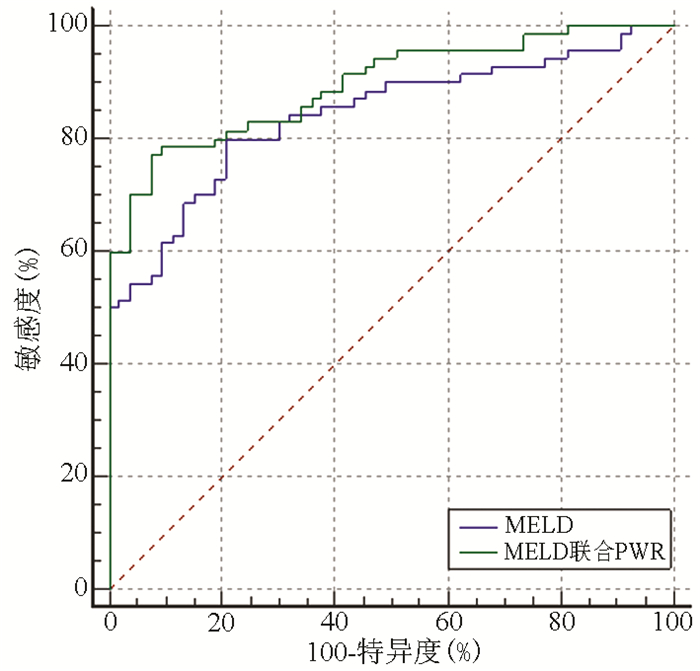
目的 探讨终末期肝病模型(MELD)评分系统联合血小板/白细胞比值(PWR)在预测HBV相关慢加急性肝衰竭(HBV-ACLF)短期预后中的价值。 方法 回顾性分析2014年6月—2019年6月苏州大学附属第一医院收治的123例HBV-ACLF患者的临床资料,根据其入院后90 d的预后分为生存组(n=53)和死亡组(n=70)。记录患者的年龄、性别及入院24 h内患者TBil、ALT、AST、GGT、ALP、SCr、Alb、前白蛋白(PAB)、INR、WBC、淋巴细胞计数(LY)、单核细胞计数(MO)、中性粒细胞计数(NE)、Hb、PLT,并计算PWR和MELD评分。计量资料2组间比较采用t检验或Mann-Whitney U检验,单因素及多因素二元logistic回归分析各因素与HBV-ACLF预后的关系,并建立MELD评分联合PWR的预测模型。绘制受试者工作特征曲线(ROC曲线),并计算约登指数、临界值、敏感度、特异度,比较单独MELD评分和MELD评分联合PWR的ROC曲线下面积(AUC),比较两者评价HBV-ACLF患者预后的价值。 结果 两组患者TBil、ALT、SCr、INR、WBC、MO、NE、Hb、PLT、PWR和MELD评分比较差异均有统计学意义(P值均<0.05)。单因素分析显示,TBil、SCr、INR、WBC、MO、NE、MELD评分对HBV-ACLF患者的预后有影响(P值均<0.05)。多因素分析显示,PWR(OR=0.883, 95%CI: 0.798~0.977, P=0.016)和MELD评分(OR=1.442, 95%CI: 1.225~1.698, P<0.001)为HBV-ACLF患者预后的独立影响因素。MELD评分联合PWR(AUC=0.895,95%CI:0.827~0.943)对HBV-ACLF患者预后的预测能力高于单独MELD评分(AUC=0.842,95%CI:0.765~0.902),差异有统计学意义(P<0.05)。 结论 MELD评分联合PWR可以提高MELD评分预测HBV-ACLF患者预后的预测效能。 Abstract:Objective To investigate the value of Model for End-Stage Liver Disease (MELD) score combined with platelet-to-white blood cell ratio (PWR) in predicting the short-term prognosis of patients with hepatitis B virus-associated acute-on-chronic liver failure (HBV-ACLF). Methods A retrospective analysis was performed for the clinical data of 123 HBV-ACLF patients who were admitted to The First Affiliated Hospital of Suzhou University from June 2014 to June 2019, and according to the prognosis on day 90 after admission, these patients were divided into survival group with 53 patients and death group with 70 patients. Related clinical data were recorded, including age, sex, and total bilirubin (TBil), alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transpeptidase (GGT), alkaline phosphatase (ALP), serum creatinine (SCr), Albumin (Alb), prealbumin (PAB), international normalized ratio (INR), white blood cell count (WBC), lymphocyte count (LY), monocyte count (MO), neutrophil count (NE), hemoglobin (Hb), and platelet count (PLT) within 24 hours after admission, and PWR and MELD score were calculated. The t-test and the Mann-Whitney U test were used for comparison of continuous data between two groups; univariate and multivariate binary logistic regression analyses were used to analyze the association between each factor and the prognosis of HBV-ACLF; a predictive model of MELD score combined with PWR was established. The receiver operating characteristic (ROC) curve was plotted, and Youden index, cut-off value, sensitivity, and specificity were calculated; the area under the ROC curve (AUC) was calculated for MELD score alone or combined with PWR to compare their value in predicting the prognosis of HBV-ACLF patients. Results There were significant differences between the two groups in TBil, ALT, SCr, INR, WBC, MO, NE, Hb, PLT, PWR, and MELD score (all P < 0.05). TBil, SCr, INR, WBC, MO, NE, and MELD score were risk factors for prognosis of HBV-ACLF patients(all P < 0.05); PWR (odds ratio [OR]=0.883, 95% confidence interval [CI]: 0.798-0.977, P=0.016) and MELD score (OR=1.442, 95%CI: 1.225-1.698, P < 0.001) were independent predictive factors for the prognosis of HBV-ACLF patients. MELD score combined with PWR had a stronger predictive efficiency than MELD score alone in predicting the prognosis of HBV-ACLF patients [0.895 (95%CI: 0.827-0.943) vs 0.842 (95%CI: 0.765-0.902), P < 0.05]. Conclusion MELD score combined with PWR can improve the efficiency of MELD score alone in predicting the prognosis of HBV-ACLF patients. -
Key words:
- Acute-On-Chronic Liver Failure /
- Hepatitis B Virus /
- Prognosis
-
表 1 两组患者一般资料比较
指标 生存组(n=53) 死亡组(n=70) 统计值 P值 年龄(岁) 47.81±14.66 52.34±11.84 t=-1.897 0.112 TBil(μmol/L) 287.80(231.10~368.65) 350.60(257.83~457.40) Z=-2.316 0.021 ALT(U/L) 472.00(227.50~889.55) 247.20(59.45~728.00) Z=-2.155 0.031 AST(U/L) 275.00(124.55~626.20) 210.60(92.75~520.50) Z=-0.950 0.342 GGT(U/L) 99.40(65.50~142.05) 81.50(51.50~123.88) Z=-1.785 0.074 ALP(U/L) 127.70(108.50~163.05) 137.00(104.30~164.23) Z=-0.020 0.984 SCr(μmol/L) 58.00(49.70~66.00) 70.00(53.50~111.38) Z=-3.210 0.001 Alb(g/L) 32.17±4.11 30.58±5.30 t=1.818 0.231 PAB(mg/L) 39.20(28.70~59.00) 41.45(28.90~64.60) Z=-0.444 0.657 INR 1.81(1.68~2.02) 2.56(2.01~3.22) Z=-5.480 <0.001 WBC(109/L) 5.92(4.47~8.02) 9.48(6.42~12.07) Z=-4.446 <0.001 LY(109/L) 1.01(0.75~1.47) 0.92(0.61~1.24) Z=-1.918 0.055 MO(109/L) 0.42(0.29~0.65) 0.61(0.35~0.90) Z=-2.541 0.011 NE(109/L) 4.21(2.97~5.77) 7.49(4.63~10.29) Z=-4.334 <0.001 Hb(g/L) 132(115~148) 120(87~141) Z=-2.166 0.018 PLT(109/L) 100(76~129) 80(45~110) Z=-2.745 0.006 PWR 16.57(11.35~23.59) 8.97(4.64~15.12) Z=-4.985 <0.001 MELD评分 20.18(18.17~22.06) 26.57(22.52~30.93) Z=-6.481 <0.001 表 2 单因素logistics分析
指标 OR 95%CI P值 TBil 1.004 1.001~1.007 0.017 ALT 1.000 0.999~1.000 0.718 SCr 1.032 1.013~1.051 0.001 INR 6.119 2.669~14.025 <0.001 WBC 1.226 1.096~1.372 <0.001 MO 2.731 1.031~7.230 0.043 NE 1.282 1.126~1.458 <0.001 Hb 0.983 0.970~0.996 0.010 PLT 0.994 0.987~1.000 0.067 PWR 0.870 0.819~0.925 <0.001 MELD评分 1.386 1.217~1.578 <0.001 表 3 MELD评分及MELD评分联合PWR预测HBV-ACLF患者预后的ROC曲线
指标 AUC 约登指数 临界值 敏感度(%) 特异度(%) MELD评分 0.842 0.593 22.315 80.00 79.25 MELD评分联合PWR 0.895 0.696 0.507 77.14 92.45 -
[1] SARIN SK, CHOUDHURY A, SHARMA MK, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific association for the study of the liver (APASL): An update[J]. Hepatol Int, 2019, 13(4): 353-390. DOI: 10.1007/s12072-019-09946-3. [2] SONG Y, SHEN Y, LU W, et al. Analysis of biochemical features of hepatitis B virus infected patients in southwest China[J]. Clin Lab, 2016, 62(9): 1803-1807. DOI: 10.7754/Clin.Lab.2016.160140. [3] HA JM, SOHN W, CHO JY, et al. Static and dynamic prognostic factors for hepatitis-B-related acute-on-chronic liver failure[J]. Clin Mol Hepatol, 2015, 21(3): 232-241. DOI: 10.3350/cmh.2015.21.3.232. [4] ZHANG Y, WANG QC. The value of PLT/WBC ratio in the evaluation of infection and thrombosis after splenectomy[J]. Chin J Gastroenterol Hepatol, 2017, 26(1): 96-98. DOI: 10.3969/j.issn.1006-5709.2017.01.027.张燕, 王全楚. 脾切除术后血小板/白细胞比值在感染判定和血栓预测中的价值[J]. 胃肠病学和肝病学杂志, 2017, 26(1): 96-98. DOI: 10.3969/j.issn.1006-5709.2017.01.027. [5] LATHOURAS K, PANAGAKIS G, BOWDEN SJ, et al. Diagnostic value of post-operative platelet-to-white blood cell ratio after splenectomy in patients with advanced ovarian cancer[J]. Int J Gynecol Cancer, 2019, 29(8): 1292-1297. DOI: 10.1136/ijgc-2019-000712. [6] GARBENS A, WALLIS C, BJARNASON G, et al. Platelet to white blood cell ratio predicts 30-day postoperative infectious complications in patients undergoing radical nephrectomy for renal malignancy[J]. Can Urol Assoc J, 2017, 11(11): e414-414e420. DOI: 10.5489/cuaj.4478. [7] CHEN Z, HUANG Y, LI S, et al. Platelet-to-white blood cell ratio: A prognostic predictor for 90-day outcomes in ischemic stroke patients with intravenous thrombolysis[J]. J Stroke Cerebrovasc Dis, 2016, 25(10): 2430-2438. DOI: 10.1016/j.jstrokecerebrovasdis.2016.06.015. [8] Liver Failure and ArtificiaI Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [9] LI SS, DUAN ZP, CHEN Y. New ideas and methods for the diagnosis and treatment of acute-on-chronic liver failure[J]. J Clin Hepatol, 2018, 34(4): 877-882. DOI: 10.3969/j.issn.1001-5256.2018.04.039.李珊珊, 段钟平, 陈煜. 慢加急性肝衰竭诊治新思路与新方法[J]. 临床肝胆病杂志, 2018, 34(4): 877-882. DOI: 10.3969/j.issn.1001-5256.2018.04.039. [10] ZHOU ZJ, LI JQ, BIN YY, et al. Effect of donor risk index on early prognosis of liver transplantation for acute-on-chronic liver failure: Experience of 159 cases in one single center[J]. Ogran Transplantation, 2019, 10(3): 318-322. DOI: 10.3969/j.issn.1674-7445.2019.03.016.周政俊, 李杰群, 宾阳阳, 等. 供体风险指数对慢加急性肝衰竭肝移植治疗早期预后的影响: 单中心159例经验[J]. 器官移植, 2019, 10(3): 318-322. DOI: 10.3969/j.issn.1674-7445.2019.03.016 [11] ZHANG Q, GUO X, ZHAO S, et al. Prognostic performance of clinical indices and model scorings for acute-on-chronic liver failure: A study of 164 patients[J]. Exp Ther Med, 2016, 11(4): 1348-1354. DOI: 10.3892/etm.2016.3037. [12] WU T, LI J, SHAO L, et al. Development of diagnostic criteria and a prognostic score for hepatitis B virus-related acute-on-chronic liver failure[J]. Gut, 2018, 67(12): 2181-2191. DOI: 10.1136/gutjnl-2017-314641. [13] ZHANG J, QIU Y, HE X, et al. Platelet-to-white blood cell ratio: A novel and promising prognostic marker for HBV-associated decompensated cirrhosis[J]. J Clin Lab Anal, 2020, 34(12): e23556. DOI: 10.1002/jcla.23556. [14] JIE Y, GONG J, XIAO C, et al. Low platelet to white blood cell ratio indicates poor prognosis for acute-on-chronic liver failure[J]. Biomed Res Int, 2018, 2018: 7394904. DOI: 10.1155/2018/7394904. [15] LIU Y, LI SQ, LI S, et al. Correlation of platelet-lymphocyte ratio and neutrophil-lymphocyte ratio with prognosis of liver failure[J]. Chin J Gastroenterol Hepatol, 2019, 28(5): 546-551. DOI: 10.3969/j.issn.1006-5709.2019.05.014.刘影, 李淑芹, 李莎, 等. 血小板/淋巴细胞比值和中性粒细胞/淋巴细胞比值与肝衰竭预后相关性研究[J]. 胃肠病学和肝病学杂志, 2019, 28(5): 546-551. DOI: 10.3969/j.issn.1006-5709.2019.05.014. [16] GANGIREDDY VG, KANNEGANTI PC, SRIDHAR S, et al. Management of thrombocytopenia in advanced liver disease[J]. Can J Gastroenterol Hepatol, 2014, 28(10): 558-564. DOI: 10.1155/2014/532191. [17] SAKAI K, IWAO T, OHO K, et al. Propranolol ameliorates thrombocytopenia in patients with cirrhosis[J]. J Gastroenterol, 2002, 37(2): 112-118. DOI: 10.1007/s005350200005. [18] LI WY, ZHANG MX, QI TT, et al. The potential factors contributing to thrombocytopenia in acute on chronic liver failure patients[J]. Chin Hepatol, 2015, 20(6): 457-461. DOI: 10.3969/j.issn.1008-1704.2015.06.009.李文燕, 张明霞, 祁婷婷, 等. 慢加急性肝衰竭患者血小板减少的可能原因[J]. 肝脏, 2015, 20(6): 457-461. DOI: 10.3969/j.issn.1008-1704.2015.06.009. [19] WANG YJ. Liver failure related bacterial infection and antimicrobial treatment[J]. J Prac Hepatol, 2014, 17(2): 117-120. DOI: 10.3969/j.issn.1672-5069.2014.02.002.王英杰. 肝衰竭并发细菌感染与抗生素治疗[J]. 实用肝脏病杂志, 2014, 17(2): 117-120. DOI: 10.3969/j.issn.1672-5069.2014.02.002. [20] ZIDER AD, ZOPEY R, GARG R, et al. Prognostic significance of infections in critically ill adult patients with acute liver injury: A retrospective cohort study[J]. Liver Int, 2016, 36(8): 1143-1150. DOI: 10.1111/liv.13073. [21] MALINCHOC M, KAMATH PS, GORDON FD, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts[J]. Hepatology, 2000, 31(4): 864-871. DOI: 10.1053/he.2000.5852. [22] ZHANG DJ, ZHOU B, HOU JL. Research progress in prognostic models of acute-on-chronic liver failure[J]. J Clin Hepatol, 2018, 34(6): 1351-1356. DOI: 10.3969/j.issn.1001-5256.2018.06.047.张东敬, 周彬, 侯金林. 慢加急性肝衰竭预后模型的研究进展[J]. 临床肝胆病杂志, 2018, 34(6): 1351-1356. DOI: 10.3969/j.issn.1001-5256.2018.06.047. [23] ZHANG WJ, ZHAO LJ, WU JZ. Value of MELD, AARC, COSSH scoring systems in evaluating the 90-day prognosis of hepatitis B virus-related acute-on-chronic liver failure[J]. J Clin Hepatol, 2020, 36(4): 813-817. DOI: 10.3969/j.issn.1001-5256.2020.04.021.张文佳, 赵丽娟, 吴基洲. MELD、AARC、COSSH评分系统对乙型肝炎相关慢加急性肝衰竭90天预后的评估价值[J]. 临床肝胆病杂志, 2020, 36(4): 813-817. DOI: 10.3969/j.issn.1001-5256.2020.04.021. [24] LI C, YOU SL, LIU HL, et al. The value of the baseline MELD scores, MELD-Na scores and iMELD scores in short-tern prognosis in hepatitis B virus related acute-on-chronic liver failure patients[J]. Chin Critical Care Med, 2014, 26(8): 539-543. DOI: 10.3760/cma.j.issn.2095-4352.2014.08.003.李晨, 游绍莉, 刘鸿凌, 等. 基线MELD、MELD-Na、iMELD 3种模型对乙型肝炎病毒相关慢加急性肝衰竭患者近期预后的评估价值[J]. 中华危重病急救医学, 2014, 26(8): 539-543. DOI: 10.3760/cma.j.issn.2095-4352.2014.08.003. [25] LI L, HU H, ZHENG XW, et al. Prediction of short-term survival by four scoring systems based on MELD in patients with acute-on-chronic hepatitis B-induced liver failure[J]. J Prac Hepatol, 2018, 21(3): 417-420. DOI: 10.3969/j.issn.1672-5069.2018.03.025.李磊, 胡辉, 郑晓玮, 等. 四种基于MELD的评分系统对慢加急性乙型肝炎肝衰竭患者短期生存的预测价值分析[J]. 实用肝脏病杂志, 2018, 21(3): 417-420. DOI: 10.3969/j.issn.1672-5069.2018.03.025. [26] ZHANG H, JIA L, YAO SW, et al. Value of MELD combined with serum sodium concentration in predicting the short-term outcome of patients with HBV-related acute-on-chronic liver failure in China: A meta-analysis[J]. J Clin Hepatol, 2018, 34(9): 1950-1955. DOI: 10.3969/j.issn.1001-5256.2018.09.024.张辉, 贾雷, 姚士伟, 等. MELD-Na评分对我国HBV相关慢加急性肝衰竭短期预后预测价值的Meta分析[J]. 临床肝胆病杂志, 2018, 34(9): 1950-1955. DOI: 10.3969/j.issn.1001-5256.2018.09.024. [27] LIU YM, LIU XJ, CHEN ZX, et al Comparison of different score systems in predicting prognosis of hepatitis B virus-associated acute-on-chronic liver failure[J]. Chin J Infect Dis, 2015, 33(12): 737-741. DOI: 10.3760/cma.j.issn.1000-6680.2015.12.004.刘艳梅, 刘先进, 陈智娴, 等. 不同评分系统判断乙型肝炎慢加急性肝衰竭预后的价值[J]. 中华传染病杂志, 2015, 33(12): 737-741. DOI: 10.3760/cma.j.issn.1000-6680.2015.12.004. [28] CHENG XP, ZHAO J, CHEN Y, et al. Comparison of the ability of the PDD-ICG clearance test, CTP, MELD, and MELD-Na to predict short-term and medium-term mortality in patients with decompensated hepatitis B cirrhosis[J]. Eur J Gastroenterol Hepatol, 2016, 28(4): 444-448. DOI: 10.1097/MEG.0000000000000538. [29] ZHANG L, CHEN W, SHENG YJ, et al. Value of Model for End-Stage Liver Disease score combined with neutrophil -lymphocyte ratio in predicting the short-term prognosis of patients with HBV-related acute-on-chronic liver failure[J]. J Clin Hepatol, 2018, 34(3): 553-557. DOI: 10.3969/j.issn.1001-5256.2018.03.021.张丽, 陈文, 盛云健, 等. MELD评分联合中性粒细胞/淋巴细胞比值对HBV相关慢加急性肝衰竭短期预后的预测价值[J]. 临床肝胆病杂志, 2018, 34(3): 553-557. DOI: 10.3969/j.issn.1001-5256.2018.03.021. -




 PDF下载 ( 1967 KB)
PDF下载 ( 1967 KB)

 下载:
下载:


