癌旁组织二酯酰甘油激酶γ表达水平对肝细胞癌患者术后生存的影响
DOI: 10.3969/j.issn.1001-5256.2021.05.023
Effect of the expression level of diacylglycerol kinase gamma in paracancerous tissue on postoperative survival in patients with hepatocellular carcinoma
-
摘要:
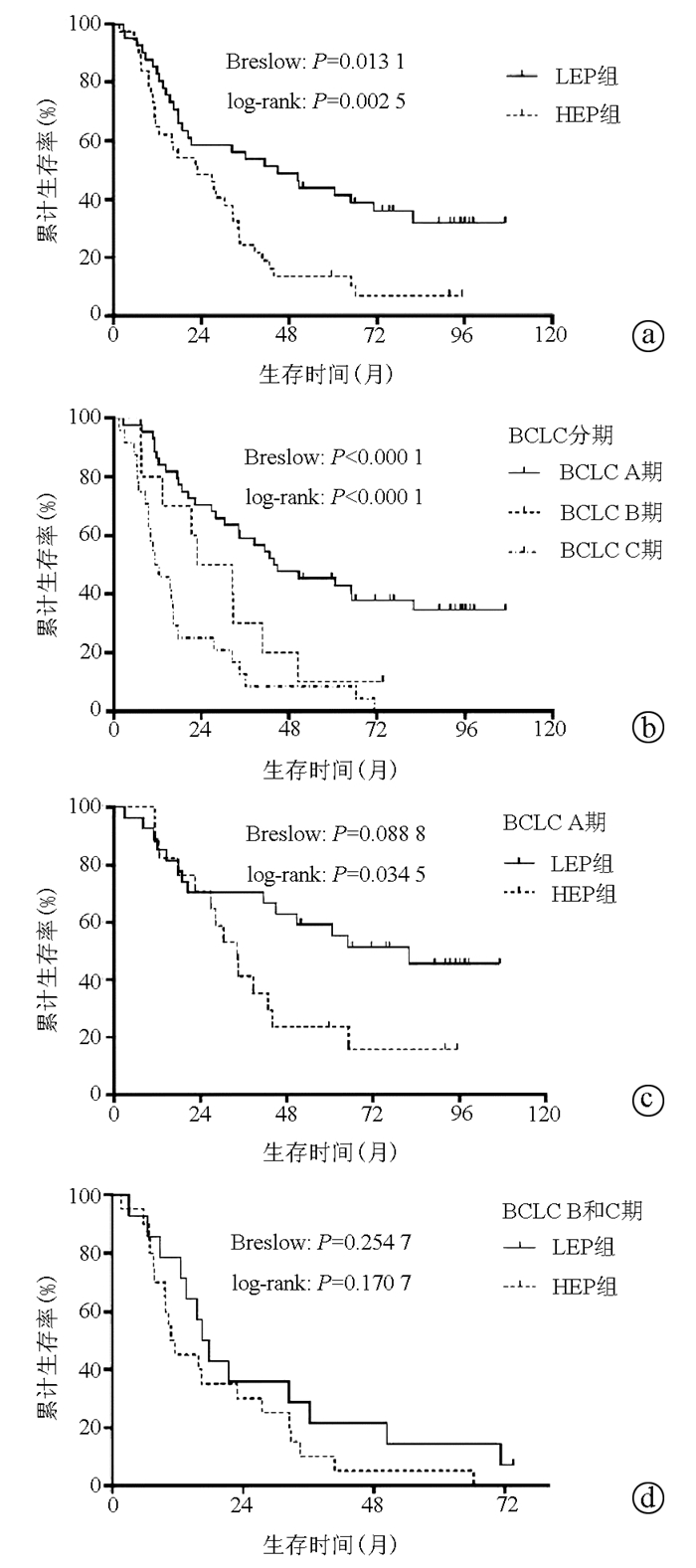
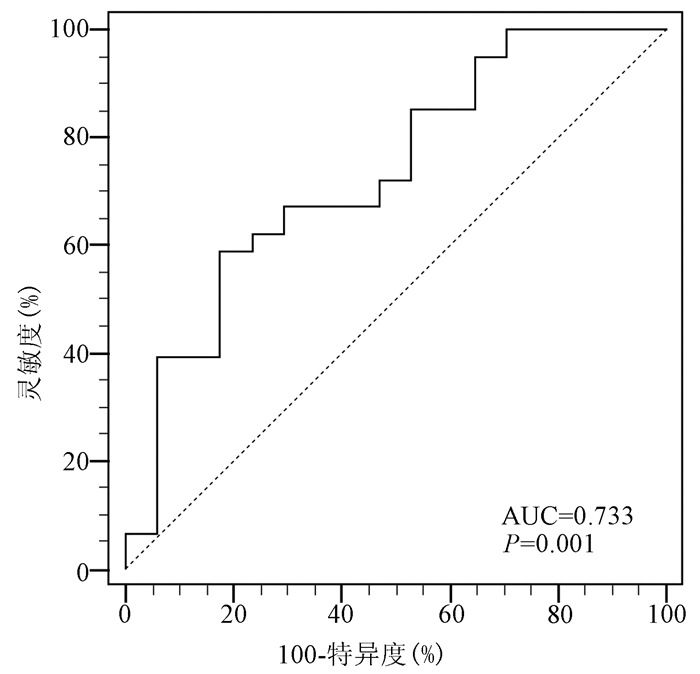
目的 探究肝癌患者癌旁组织中二酯酰甘油激酶γ(DGKγ)的表达水平对术后生存的影响及临床价值。 方法 收集2008年12月—2012年8月郑州大学附属肿瘤医院收治的78例行手术切除的肝癌患者资料。实时荧光定量PCR检测癌旁组织中DGKγmRNA的表达水平,将78例患者分为低表达组(DGKγ<0.0862,简称LEP组)和高表达组(DGKγ≥0.0862,简称HEP组),比较2组间的基本资料特征。计量资料2组间比较使用t检验与Mann-Whitney U检验;计数资料2组间比较使用χ2检验。单因素和多因素Cox回归分析患者生存预后的独立影响因素;Kaplan-Meier法分析所有患者和巴塞罗那(BCLC)分期各亚组中LEP组和HEP组的生存情况。 结果 多因素Cox分析显示:癌旁DGKγ表达水平(HR=1.913,95%CI:1.111~3.296,P=0.019)、HBsAg(HR=2.645,95%CI:1.264~5.537,P=0.010)、Alb(HR=0.952,95%CI:0.916~0.990,P=0.013)、BCLC分期(HR=1.702,95%CI:1.267~2.286,P<0.001)、肿瘤大小(HR=1.083,95%CI:1.019~1.152,P=0.011)是肝癌患者术后长期生存的独立影响因素。78例患者中,LEP组的中位生存时间为45.0个月,显著高于HEP组的22.9个月(P=0.0025)。分层分析显示,BCLC A期中,LEP组的远期生存情况显著的优于HEP组(P=0.0345);B和C期中,LEP组和HEP组中位生存时间分别为16.5个月和10.8个月,2组间的近期和远期生存差异无统计学意义(P>0.05)。 结论 癌旁组织中DGKγ的表达水平可能是一种新的能够预测和评估肝癌患者术后长期生存风险的指标,具有一定的临床应用价值。 Abstract:Objective To investigate the effect of the expression level of diacylglycerol kinase gamma (DGKγ) in paracancerous tissue on the postoperative prognosis of patients with hepatocellular carcinoma (HCC) and its clinical value. Methods Related clinical data were collected from 78 HCC patients who were admitted and underwent surgical resection from December 2008 to August 2012 in the Affiliated Cancer Hospital of Zhengzhou University. Quantitative real-time PCR was used to measure the mRNA expression level of DGKγ in paracancerous tissue, and then the 78 patients were divided into low expression group (DGKγ < 0.086 2, LEP group) and high expression group (DGKγ ≥0.086 2, HEP group). Basic data and clinical features were compared between the two groups. The t-test and the Mann-Whitney U test were used for comparison of continuous data, and the chi-square test and the corrected chi-square test were used for comparison of categorical data. Univariate and multivariate Cox regression analyses were used to investigate independent influencing factors for survival and prognosis, and the Kaplan-Meier method was used to analyze the overall survival trends of all patients and the LEP and HEP groups in each subgroup of Barcelona Clinic Liver Cancer (BCLC) stages. Results The multivariate Cox regression analysis showed that the expression level of DGKγ (HR=1.913, 95%CI: 1.111-3.296, P=0.019), HBsAg (HR=2.645, 95%CI: 1.264- 5.537, P=0.010), Alb (HR=0.952, 95%CI: 0.916-0.990, P=0.013), BCLC stage (HR=1.702, 95%CI: 1.267-2.286, P < 0.001) and tumor size (HR=1.083, 95%CI: 1.019-1.152, P=0.011) were independent influencing factors for long-term survival of HCC patients; the LEP group had a significantly longer median survival time than the HEP group (45.0 months vs 22.9 months, P= 0.002 5). The stratified analysis showed that for BCLC stage A HCC, the LEP group had significantly better long-term survival than the HEP group (P=0.034 5); for BCLC stage B/C HCC, the LEP group had a longer median survival time than the HEP group (16.5 months vs 10.8 months), but there was no significant difference in short- and long-term survival between the two groups (P > 0.05). Conclusion The expression level of DGKγ in paracancerous tissue may be a new index for predicting and evaluating the long-term survival risk of HCC patients after surgery and has certain value in clinical application. -
Key words:
- Liver Neoplasms /
- Diglycerides /
- Prognosis
-
表 1 癌旁组织DGKγ LEP组与HEP组的临床资料比较
指标 总患者(n=78) LEP组(n=41) HEP组(n=37) 统计值 P值 年龄(岁) 54.32±10.74 55.17±10.62 53.38±10.94 t=0.734 0.465 性别(男/女) 67/11 33/8 34/3 χ2=1.253 0.263 HBsAg(阳性/阴性) 60/18 28/13 32/5 χ2=2.674 0.102 AFP(ng/μl) 420.2(12.7~1210.0) 237.6(4.3~1039.0) 532.4(21.1~1210.0) Z=-1.621 0.105 ALT(U/L) 38.0(25.0~63.3) 38.0(24.5~55.0) 38.0(25.5~70.5) Z=-0.280 0.779 AST(U/L) 44.0(31.0~66.0) 42.0(32.0~60.0) 49.0(28.5~72.0) Z=-0.756 0.450 ALP(U/L) 113.5(86.8~147.0) 123.0(90.0~153.0) 100.0(85.5~126.0) Z=-1.501 0.133 GGT(U/L) 96.0(56.8~179.0) 117.0(50.5~191.7) 87.0(60.5~150.9) Z=-1.046 0.296 TBil(μmol/L) 15.4(10.9~20.6) 15.5(11.4~20.5) 14.4(9.9~20.7) Z=-0.530 0.596 Alb(g/L) 39.88±6.61 39.71±7.77 40.08±5.11 t=-0.247 0.806 Glb(g/L) 29.56±6.34 30.07±5.79 28.99±6.93 t=0.751 0.455 RBC(×1012/L) 4.31±0.63 4.36±0.59 4.25±0.66 t=0.775 0.441 PLT(×109/L) 151(104~200) 167(113~212) 140(102~186) Z=-1.256 0.209 PT(s) 13.4(12.1~14.4) 13.0(11.7~14.4) 13.7(12.7~14.7) Z=-1.987 0.047 INR 1.15(1.02~1.23) 1.10(0.99~1.25) 1.16(1.08~1.23) Z=-1.392 0.164 FIB(g/L) 3.00±0.85 3.02±0.93 2.97±0.76 t=0.097 0.767 Child-Pugh分级(A/B) 69/9 38/3 31/6 χ2=0.763 0.382 术中输血(是/否) 26/52 12/29 14/23 χ2=0.643 0.423 BCLC分期(A/B/C) 44/10/24 27/4/10 17/6/14 χ2=3.143 0.208 肿瘤大小(cm) 7.0(5.0~11.0) 7.0(4.5~12.0) 8.0(5.0~10.5) Z=-0.431 0.666 肿瘤数目(1个/≥2个) 58/20 33/8 25/12 χ2=1.703 0.192 切缘(是/否) 48/30 26/15 22/15 χ2=0.129 0.720 表 2 所有患者生存预后的单因素分析
指标 HR(95%CI) P值 年龄(岁) 0.984(0.960~1.008) 0.186 性别(男/女) 0.775(0.381~1.577) 0.482 HBsAg(阳性/阴性) 2.376(1.198~4.710) 0.013 AFP(ng/μl) 1.001(1.000~1.001) 0.016 ALT(U/L) 1.001(1.000~1.001) 0.293 AST(U/L) 1.001(1.000~1.001) 0.088 ALP(U/L) 1.004(1.000~1.008) 0.080 GGT(U/L) 1.002(1.000~1.004) 0.063 TBil(μmol/L) 0.994(0.966~1.022) 0.660 Alb(g/L) 0.953(0.926~0.981) 0.001 Glb(g/L) 1.007(0.967~1.048) 0.749 RBC(×1012/L) 0.817(0.508~1.314) 0.405 PLT(×109/L) 1.003(1.000~1.006) 0.037 PT(s) 1.059(0.945~1.186) 0.324 INR 2.649(0.825~8.508) 0.102 FIB(g/L) 1.338(0.999~1.791) 0.051 Child-Pugh分级(A/B) 1.517(0.718~3.203) 0.275 术中输血(是/否) 2.430(1.437~4.111) 0.001 BCLC分期(A/B/C) 2.033(1.532~2.699) <0.001 肿瘤大小(cm) 1.088(1.030~1.148) 0.002 肿瘤数目(1个/≥2个) 1.814(1.039~3.167) 0.036 切缘(是/否) 1.859(1.112~3.107) 0.018 癌旁DGKγ (HEP/LEP) 2.188(1.302~3.677) 0.003 -
[1] BRAY F, FERLAY J, SOERJOMATARAM I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2018, 68(6): 394-424. DOI: 10.3322/caac.21492. [2] TORRE LA, BRAY F, SIEGEL RL, et al. Global cancer statistics, 2012[J]. CA Cancer J Clin, 2015, 65(2): 87-108. DOI: 10.3322/caac.21262. [3] ZHOU M, WANG H, ZENG X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2019, 394(10204): 1145-1158. DOI: 10.1016/S0140-6736(19)30427-1. [4] LIU AX, WANG HQ, BO WT, et al. Clinical efficacy and prognostic factors analysis of hepatectomy for hepatocellular carcinoma[J]. Chin J Dig Surg, 2019, 18(4): 368-374. DOI: 10.3760/cma.j.issn.1673-9752.2019.04.012.刘爱祥, 王海清, 薄文滔, 等. 肝细胞癌肝切除术的临床疗效及预后因素分析[J]. 中华消化外科杂志, 2019, 18(4): 368-374. DOI: 10.3760/cma.j.issn.1673-9752.2019.04.012. [5] European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma[J]. J Hepatol, 2018, 69(1): 182-236. DOI: 10.1016/j.jhep.2018.03.019. [6] Bureau of Medical Administration, National Health Commission of The People's Republic of China. Guidelines for diagnosis and treatment of primary liver cancer in China (2019 edition)[J]. J Clin Hepatol, 2020, 36(2): 277-292. DOI: 10.3969/j.issn.1001-5256.2020.02.007.中华人民共和国国家卫生健康委员会医政医管局. 原发性肝癌诊疗规范(2019年版)[J]. 临床肝胆病杂志, 2020, 36(2): 277-292. DOI: 10.3969/j.issn.1001-5256.2020.02.007. [7] QIAN XJ, QU CF, LU FM. The tumor markers of hepatocellular carcinoma play an indispensable role in ultrasound screening and monitoring early hepatocellular carcinoma[J]. Liver, 2019, 24(8): 851-853. DOI: 10.3969/j.issn.1008-1704.2019.08.003.钱相君, 曲春枫, 鲁凤民. 肝癌肿瘤标记物在超声筛查监测早期肝细胞癌中的作用不可或缺[J]. 肝脏, 2019, 24(8): 851-853. DOI: 10.3969/j.issn.1008-1704.2019.08.003. [8] HUANG C, FRETER C. Lipid metabolism, apoptosis and cancer therapy[J]. Int J Mol Sci, 2015, 16(1): 924-949. DOI: 10.3390/ijms16010924. [9] ARRANZ-NICOLÁS J, MÉRIDA I. Biological regulation of diacylglycerol kinases in normal and neoplastic tissues: New opportunities for cancer immunotherapy[J]. Adv Biol Regul, 2020, 75: 100663. DOI: 10.1016/j.jbior.2019.100663. [10] MÉRIDA I, TORRES-AYUSO P, ÁVILA-FLORES A, et al. Diacylglycerol kinases in cancer[J]. Adv Biol Regul, 2017, 63: 22-31. DOI: 10.1016/j.jbior.2016.09.005. [11] KAI M, YAMAMOTO E, SATO A, et al. Epigenetic silencing of diacylglycerol kinase gamma in colorectal cancer[J]. Mol Carcinog, 2017, 56(7): 1743-1752. DOI: 10.1002/mc.22631. [12] GUO Z, JIA J, YAO M, et al. Diacylglycerol kinase γ predicts prognosis and functions as a tumor suppressor by negatively regulating glucose transporter 1 in hepatocellular carcinoma[J]. Exp Cell Res, 2018, 373(1-2): 211-220. DOI: 10.1016/j.yexcr.2018.11.001. [13] HE Z, CHEN J, WANG J, et al. Expression of hepatitis B surface antigen in liver tissues can serve as a predictor of prognosis for hepatitis B virus-related hepatocellular carcinoma patients after liver resection[J]. Eur J Gastroenterol Hepatol, 2021, 33(1): 76-82. DOI: 10.1097/MEG.0000000000001698. [14] WANG L, LI Q, ZHANG J, et al. A novel prognostic scoring model based on albumin and γ-glutamyltransferase for hepatocellular carcinoma prognosis[J]. Cancer Manag Res, 2019, 11: 10685-10694. DOI: 10.2147/CMAR.S232073. [15] YAN X, YAO M, WEN X, et al. Elevated apolipoprotein B predicts poor postsurgery prognosis in patients with hepatocellular carcinoma[J]. Onco Targets Ther, 2019, 12: 1957-1964. DOI: 10.2147/OTT.S192631. [16] WU G, WU J, WANG B, et al. Importance of tumor size at diagnosis as a prognostic factor for hepatocellular carcinoma survival: A population-based study[J]. Cancer Manag Res, 2018, 10: 4401-4410. DOI: 10.2147/CMAR.S177663. [17] WU XF, LIU YW, ZHANG H, et al. Application value of different Barcelona clinical liver cancer Kinki staging in radical resection of liver cancer[J]. Chin J Dig Surg, 2020, 19(12): 1266-1272. DOI: 10.3760/cma.j.cn115610-20201102-00691.吴晓峰, 刘一纬, 张慧, 等. 不同巴塞罗那临床肝癌Kinki分期在肝癌根治术中的应用价值[J]. 中华消化外科杂志, 2020, 19(12): 1266-1272. DOI: 10.3760/cma.j.cn115610-20201102-00691. [18] MASSART J, ZIERATH JR. Role of diacylglycerol kinases in glucose and energy homeostasis[J]. Trends Endocrinol Metab, 2019, 30(9): 603-617. DOI: 10.1016/j.tem.2019.06.003. [19] RAINERO E, CIANFLONE C, PORPORATO PE, et al. The diacylglycerol kinase α/atypical PKC/β1 integrin pathway in SDF-1α mammary carcinoma invasiveness[J]. PLoS One, 2014, 9(6): e97144. DOI: 10.1371/journal.pone.0097144. [20] FILIGHEDDU N, SAMPIETRO S, CHIANALE F, et al. Diacylglycerol kinase α mediates 17-β-estradiol-induced proliferation, motility, and anchorage-independent growth of Hec-1A endometrial cancer cell line through the G protein-coupled estrogen receptor GPR30[J]. Cell Signal, 2011, 23(12): 1988-1996. DOI: 10.1016/j.cellsig.2011.07.009. [21] DOMINGUEZ CL, FLOYD DH, XIAO A, et al. Diacylglycerol kinase α is a critical signaling node and novel therapeutic target in glioblastoma and other cancers[J]. Cancer Discov, 2013, 3(7): 782-797. DOI: 10.1158/2159-8290.CD-12-0215. [22] BACCHIOCCHI R, BALDANZI G, CARBONARI D, et al. Activation of alpha-diacylglycerol kinase is critical for the mitogenic properties of anaplastic lymphoma kinase[J]. Blood, 2005, 106(6): 2175-2182. DOI: 10.1182/blood-2005-01-0316. [23] KONG Y, ZHENG Y, JIA Y, et al. Decreased LIPF expression is correlated with DGKA and predicts poor outcome of gastric cancer[J]. Oncol Rep, 2016, 36(4): 1852-1860. DOI: 10.3892/or.2016.4989. [24] MCMURRAY HR, SAMPSON ER, COMPITELLO G, et al. Synergistic response to oncogenic mutations defines gene class critical to cancer phenotype[J]. Nature, 2008, 453(7198): 1112-1116. DOI: 10.1038/nature06973. [25] TAKEISHI K, TAKETOMI A, SHIRABE K, et al. Diacylglycerol kinase alpha enhances hepatocellular carcinoma progression by activation of Ras-Raf-MEK-ERK pathway[J]. J Hepatol, 2012, 57(1): 77-83. DOI: 10.1016/j.jhep.2012.02.026. -



 PDF下载 ( 2110 KB)
PDF下载 ( 2110 KB)

 下载:
下载: