术前外周血单个核细胞微RNA-192对孤立性肝细胞癌微血管侵犯的预测价值
DOI: 10.3969/j.issn.1001-5256.2021.05.028
Value of preoperative microRNA-192 in peripheral blood mononuclear cells in predicting microvascular invasion of solitary hepatocellular carcinoma
-
摘要:
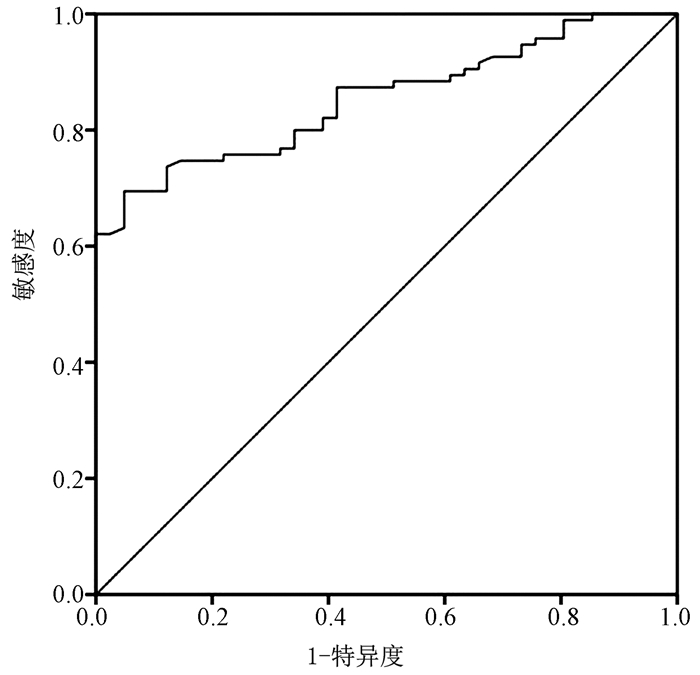
目的 探讨术前外周血单个核细胞微RNA(miRNA, miR)-192对孤立性肝细胞癌(简称肝癌)血管侵犯(MVI)的预测价值。 方法 选取2018年3月—2020年4月于北京朝阳医院西区肝胆胰脾外科接受手术治疗的HCC患者136例,收集患者相关资料,术前行超声检查,并检测患者外周血单个核细胞miR-192表达情况。根据术后病理检查是否有MVI分为MVI组(n=41)和非MVI组(n=95)。计量资料2组间比较采用t检验,计数资料2组间比较采用χ2检验。对可能影响MVI的各因素进行单因素及多因素logistic回归分析,采用ROC曲线分析术前miR-192表达对MVI的预测价值。 结果 MVI组患者术前外周血单个核细胞miR-192相对表达量明显低于非MVI组,差异有统计学意义(0.798±0.164 vs 1.086±0.215,t=7.663, P<0.01)。多因素logistic回归分析结果显示,术前miR-192(OR=3.999,95%CI: 1.585~10.086,P=0.003)、结节类型(OR=3.241,95%CI: 1.154~9.106,P=0.026)以及包膜类型(OR=2.776,95%CI: 1.088~7.084,P=0.033)是影响肝癌患者MVI发生的独立危险因素。术前外周血单个核细胞miR-192预测MVI的ROC曲线下面积为0.872,,95%CI: 0.768~0.931,敏感度68.38%、特异度70.59%,最佳截断值为0.858。 结论 术前外周血单个核细胞miR-192与孤立性肝癌患者MVI的发生有密切联系,术前miR-192偏低、多结节以及无包膜将增加MVI的发生风险,术前miR-192水平对孤立性肝癌MVI具有良好的预测价值。 Abstract:Objective To investigate the value of preoperative microRNA-192 (miR-192) in peripheral blood mononuclear cells (PBMCs) in predicting microvascular invasion (MVI) of solitary hepatocellular carcinoma (HCC). Methods A total of 136 patients with HCC who underwent surgical treatment in Department of Hepatobiliary-Pancreatic-Splenic Surgery, West Branch of Chaoyang Hospital, Capital Medical University, from March 2018 to April 2020 were enrolled and related data were collected. Ultrasound examination was performed and the expression of miR-192 in PBMCs was measured before surgery. According to the presence or absence of MVI after postoperative pathological examination, the patients were divided into MVI group with 41 patients and non-MVI group with 95 patients. The t-test was used for comparison of continuous data between two groups, and the chi-square test was used for comparison of categorical data between two groups. Univariate and multivariate logistic regression analyses were used to analyze the factors that may be associated with MVI, and the receiver operating characteristic (ROC) curve was used to analyze the value of preoperative miR-192 expression in predicting MVI. Results The MVI group had significantly lower preoperative relative expression of miR-192 in PBMCs than the non-MVI group (0.798±0.164 vs 1.086±0.215, t=7.663, P < 0.01). The multivariate logistic regression analysis showed that preoperative miR-192 (odds ratio [OR]=3.999, 95% confidence interval [CI]: 1.585-10.086, P=0.003), nodule type (OR=3.241, 95%CI: 1.154-9.106, P=0.026), and capsule type (OR=2.776, 95%CI: 1.088-7.084, P=0.033) were independent risk factors for MVI in HCC patients. The area under the ROC curve was 0.872 (95%CI: 0.768-0.931), with a sensitivity of 68.38% and a specificity of 70.59% at the optimal cut-off value of 0.858. Conclusion Preoperative miR-192 in PBMCs is closely associated with the development of MVI in patients with solitary HCC. Low preoperative miR-192, multiple nodules, and absence of capsule may increase the risk of MVI. Preoperative miR-192 level has a good value in predicting MVI in patients with solitary HCC. -
Key words:
- Carcinoma, Hepatocellular /
- Microvascularinvasion /
- MicroRNAs /
- Risk Factors
-
表 1 引物序列
引物 序列 miR-192 上游引物:5′-CTGACCTATGAATTGACAGCC-3′ 下游引物:5′-TTAGGCTCCAGACGGTTTAT-3′ U6 上游引物:5′-CTCGCTTCGGCAGCACA-3′ 下游引物:5′-TCTGCGACTATAAATACGA-3′ 表 2 MVI发生单因素分析
因素 MVI组(n=41) 非MVI组(n=95) 统计值 P值 性别(例) χ2=0.138 0.710 男 23 50 女 18 45 年龄(岁) 50.72±9.17 49.87±10.22 t=0.459 0.647 肿瘤直径(cm) 5.64±2.16 4.28±1.78 t=3.828 <0.001 肿瘤位置(例) χ2=1.434 0.152 跨叶 9 12 左叶 15 33 右叶 17 50 结节类型(例) χ2=5.422 <0.001 类圆型 15 78 单结节型 14 13 多结节型 12 4 包膜类型(例) χ2=5.914 <0.001 包膜完整 9 69 包膜缺损 14 19 无包膜 18 7 Child-Pugh分级(例) χ2=0.416 0.519 A级 27 57 B级 14 38 肝硬化(例) χ2=0.558 0.455 有 24 49 无 17 46 表 3 多因素logistic回归分析
因素 B值 SE Wald P值 OR 95%CI 术前miR-192(偏低vs偏高) 1.386 0.472 8.623 0.003 3.999 1.585~10.086 结节类型(多结节vs单结节) 1.176 0.527 4.980 0.026 3.241 1.154~9.106 包膜类型(无包膜vs有包膜) 1.021 0.478 4.562 0.033 2.776 1.088~7.084 -
[1] KULIK L, EI-SERAG HB. Epidemiology and management of hepatocellular carcinoma[J]. Gastroenterology, 2019, 156(2): 477-491. e1. http://www.sciencedirect.com/science/article/pii/S0891552010000590 [2] WILSON GC, GELLER DA. Evolving surgical options for hepatocellular carcinoma[J]. Surg Oncol Clin N Am, 2019, 28(4): 645-661. DOI: 10.1016/j.soc.2019.06.006. [3] GAO H, WEN SJ, ZHANG X, et al. Preoperative risk factor analysis and prediction model establishment of microvascular invasion in small hepatocellular carcinoma[J]. Chin J Gen Surg, 2019, 34(11): 921-924. DOI: 10.3670.cma.j.issn.1007-631X.2019.11.003.高航, 翁山耕, 张翔, 等. 小肝癌合并微血管侵犯的术前危险因素分析及预测模型构建[J]. 中华普通外科杂志, 2019, 34(11): 921-924. DOI: 10.3670.cma.j.issn.1007-631X.2019.11.003. [4] TIWARI A, MUKHERJEE B, DIXIT M. MicroRNA key to angiogenesis regulation: MiRNA biology and therapy[J]. Curr Cancer Drug Targets, 2018, 18(3): 266-277. DOI: 10.2174/1568009617666170630142725. [5] LIU C, SONG Z. Relationship between microRNA-21 and TLRs/NF-κB signaling pathway in peripheral blood mononuclear cells of rats with hepatocellular carcinoma[J]. Chin Hepatol, 2018, 23(2): 162-164. DOI: 10.3969/j.issn.1008-1704.2018.02.020.刘驰, 宋展. 肝癌大鼠癌组织microRNA-21与外周血单个核细胞TLRs/NF-κB信号通路的关系[J]. 肝脏, 2018, 23(2): 162-164. DOI: 10.3969/j.issn.1008-1704.2018.02.020. [6] Liver cancer committee of China Anti Cancer Association, Hepatology group of Hepatology branch of Chinese Medical Association, Pathology Committee of China Anti Cancer Association, et al. Evidence-based practice guidelines for the standardized pathological diagnosis of primary liver cancer in China (2015 update)[J]. J Clin Hepatol, 2015, 31(6): 833-839. DOI: 10.3969/j.issn.1001-5256.2015.06.004.中国抗癌协会肝癌专业委员会, 中华医学会肝病学分会肝癌学组, 中国抗癌协会病理专业委员会, 等. 原发性肝癌规范化病理诊断指南(2015年版)[J]. 临床肝胆病杂志, 2015, 31(6): 833-839. DOI: 10.3969/j.issn.1001-5256.2015.06.004. [7] ZENG F, CHEN B, ZENG J, et al. Preoperative neutrophil-lymphocyte ratio predicts the risk of microvascular invasion in hepatocellular carcinoma: A meta-analysis[J]. Int J Biol Markers, 2019, 34(3): 213-220. DOI: 10.1177/1724600819874487. [8] NITTA H, ALLARD MA, SEBAGH M, et al. Predictive model for microvascular invasion of hepatocellular carcinoma among candidates for either hepatic resection or liver transplantation[J]. Surgery, 2019, 165(6): 1168-1175. DOI: 10.1016/j.surg.2019.01.012. [9] YANG GH, GAO ZL, SUN WJ, et al. The risk factors of microvascular invasion in hepatocellular carcinoma based on CT characteristics[J]. J Pract Radiol, 2020, 36(8): 1248-1252, 1265. DOI: 10.3969/j.issn.1002-1671.2020.08.018.杨冠华, 高知玲, 孙文杰, 等. 基于CT特征肝细胞癌微血管侵犯危险因素研究[J]. 实用放射学杂志, 2020, 36(8): 1248-1252, 1265. DOI: 10.3969/j.issn.1002-1671.2020.08.018. [10] BAI X, MA ZH, HAO ZQ, et al. Research advances in the risk factors for microvascular invasion in hepatocellular carcinoma[J]. J Clin Hepatol, 2019, 35(11): 2578-2581. DOI: 10.3969/j.issn.1001-5256.2019.11.042.白雪, 马作红, 郝志强, 等. 肝细胞癌微血管侵犯相关危险因素[J]. 临床肝胆病杂志, 2019, 35(11): 2578-2581. DOI: 10.3969/j.issn.1001-5256.2019.11.042. [11] ERSTAD DJ, TANABE KK. Prognostic and therapeutic implications of microvascular invasion in hepatocellular carcinoma[J]. Ann Surg Oncol, 2019, 26(5): 1474-1493. DOI: 10.1245/s10434-019-07227-9. [12] SOTIROPOULOS GC, MACHAIRAS N, FOUZAS I, et al. Prediction of microvascular tumor invasion in liver transplant candidates with hepatocellular carcinoma: A feasible concept or a misleading illusion?[J]. Transplant Proc, 2019, 51(2): 421-423. DOI: 10.1016/j.transproceed.2019.01.016. [13] AST V, KORDAβ T, OSWALD M, et al. MiR-192, miR-200c and miR-17 are fibroblast-mediated inhibitors of colorectal cancer invasion[J]. Oncotarget, 2018, 9(85): 35559-35580. DOI: 10.18632/oncotarget.26263. [14] ZOU P, ZHU M, LIAN C, et al. miR-192-5p suppresses the progression of lung cancer bone metastasis by targeting TRIM44[J]. Sci Rep, 2019, 9(1): 19619. DOI: 10.1038/s41598-019-56018-5. [15] ZHAO J, XU J, ZHANG R. SRPX2 regulates colon cancer cell metabolism by miR-192/215 via PI3K-Akt[J]. Am J Transl Res, 2018, 10(2): 483-490. http://europepmc.org/abstract/MED/29511442 [16] GU Y, WEI X, SUN Y, et al. miR-192-5p silencing by genetic aberrations is a key event in hepatocellular carcinomas with cancer stem cell features[J]. Cancer Res, 2019, 79(5): 941-953. DOI: 10.1158/0008-5472.CAN-18-1675. [17] LI Y, ZHANG J, YAN LM. Values of miR-9, miR-192 and miR-205 in diagnosis of cervical cancer[J]. J Nanchang Univ(Med Sci Edition), 2020, 60(3): 74-77, 97. DOI: 10.13764/j.cnki.ncdm.2020.03.016.李艳, 张锦, 闫丽明. miR-9、miR-192和miR-205在宫颈癌诊断中的价值[J]. 南昌大学学报(医学版), 2020, 60(3): 74-77, 97. DOI: 10.13764/j.cnki.ncdm.2020.03.016. [18] DU X, QI F, LU S, et al. Nicotine upregulates FGFR3 and RB1 expression and promotes non-small cell lung cancer cell proliferation and epithelial-to-mesenchymal transition via downregulation of miR-99b and miR-192[J]. Biomed Pharmacother, 2018, 101: 656-662. DOI: 10.1016/j.biopha.2018.02.113. [19] WANG XZ, WU WF. Correlation of the expressions of miR-155 and suppressor of cytokine signaling 1 mRNA in peripheral blood mononuclear cells with the degree of liver injury in patients with chronic hepatitis B[J/CD]. Chin J Liver Dis(Electronic Edition), 2019, 11(3): 14-20. DOI: 10.3969/j.issn.1674-7380.2019.03.003.汪增秀, 吴卫锋. 慢性乙型肝炎患者外周血单个核细胞中miR-155和细胞因子信号转导抑制分子1相对表达量与肝功能损伤程度的相关性[J/CD]. 中国肝脏病杂志(电子版), 2019, 11(3): 14-20. DOI: 10.3969/j.issn.1674-7380.2019.03.003. [20] SHAO MF, ZOU JA, YU ZQ, et al. Expression and clinical significance of miR-21 in peripheral blood mononuclear cells of patients with prostate cancer[J]. Chin J Med Offic, 2019, 47(8): 799-801, 803. DOI: 10.16680/j.1671-3826.2019.08.09.邵明峰, 邹建安, 余子强, 等. 前列腺癌患者外周血单个核细胞中miR-21表达及临床意义[J]. 临床军医杂志, 2019, 47(8): 799-801, 803. DOI: 10.16680/j.1671-3826.2019.08.09. -



 PDF下载 ( 1989 KB)
PDF下载 ( 1989 KB)

 下载:
下载:


