红细胞分布宽度/血小板比值、血小板/淋巴细胞比值、中性粒细胞/淋巴细胞比值对慢性丙型肝炎肝硬化代偿期的预测价值
DOI: 10.3969/j.issn.1001-5256.2021.06.021
Value of red blood cell distribution width-to-platelet ratio, platelet-to-lymphocyte ratio, and neutrophil-to-lymphocyte ratio in predicting compensated liver cirrhosis in patients with chronic hepatitis C
-
摘要:
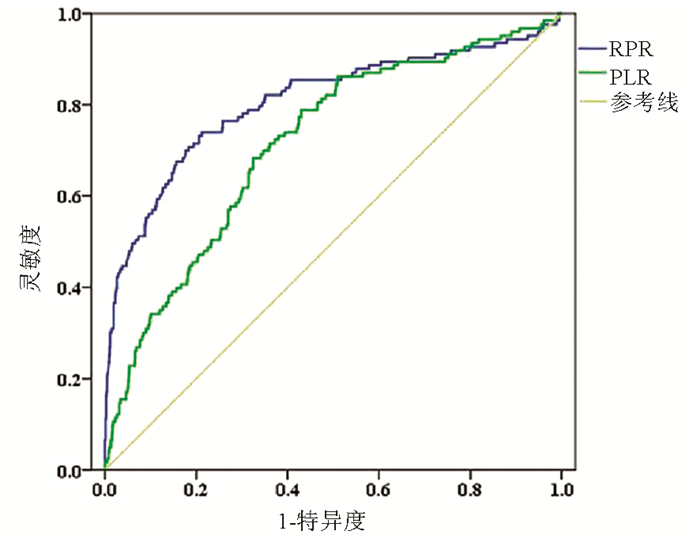
目的 通过比较慢性丙型肝炎患者和丙型肝炎肝硬化代偿期患者的血清学指标,分析红细胞分布宽度/血小板比值(RPR)、血小板/淋巴细胞比值(PLR)和中性粒细胞/淋巴细胞比值(NLR)对慢性丙型肝炎肝硬化代偿期的预测价值。 方法 在2019年9月—12月、2020年9月—12月分别在丙型肝炎发病较为集中的扶余县2个乡镇对慢性丙型肝炎患者开展肝硬化和肝癌筛查。收集所有患者的一般资料,检测其HCV RNA定量、肝功能和血常规,同时行肝瞬时弹性成像和腹部超声检查。计算RPR、PLR、NLR、FIB-4和APRI。计量资料2组间比较采用Mann-Whiney U检验;计数资料2组间比较采用χ2检验。采用受试者工作特征(ROC)曲线选取RPR、PLR的最佳截断值。采用多因素非条件logistic回归模型分析慢性丙型肝炎肝硬化的相关危险因素。采用线性回归趋势性检验分析不同纤维化分期的丙型肝炎患者之间RPR、PLR、FIB-4和APRI的变化趋势。 结果 共纳入慢性丙型肝炎患者968例,其中确诊为肝硬化代偿期(肝硬化组)患者123例(12.7%)。与慢性丙型肝炎组相比,肝硬化组RPR升高,PLR降低,差异均有统计学意义(P值均<0.001)。多因素分析结果显示,年龄>60岁、白蛋白<40 g/L、RPR>0.081、PLR<91.11、FIB-4>3.25、APRI>2与丙型肝炎性肝硬化代偿期的发生有关(OR值分别为1.79、10.40、3.83、2.25、3.14、3.60,95%CI值分别为1.12~2.86、3.47~31.18、2.19~6.69、1.31~3.89、1.74~5.67、1.10~11.78,P值分别为0.015、<0.001、<0.001、0.004、<0.001、0.035)。随着纤维化严重程度的加重,RPR、FIB-4、APRI呈逐渐升高趋势,PLR呈逐渐降低趋势(P值均<0.001)。 结论 RPR、PLR与慢性丙型肝炎肝硬化代偿期的发生、纤维化进展程度相关。对于慢性丙型肝炎老年患者(年龄>60岁),在监测白蛋白和肝纤维化指标变化的同时,也应定期监测RPR和PLR,以早期发现肝硬化,及时干预治疗,降低肝癌发生率。 -
关键词:
- 肝炎,丙型 /
- 肝硬化 /
- 红细胞分布宽度 /
- 平均血小板体积 /
- 中性粒细胞-淋巴细胞比值
Abstract:Objective To investigate the value of red blood cell distribution width-to-platelet ratio (RPR), platelet-to-lymphocyte ratio (PLR), and neutrophil-to-lymphocyte ratio (NLR) in predicting chronic hepatitis C (CHC)-related compensated liver cirrhosis by comparing serological markers between CHC patients and patients with compensated hepatitis C cirrhosis. Methods The patients with CHC in two townships of Fuyu County were screened for liver cirrhosis and liver cancer from September to December in 2019 and 2020, respectively. General information was collected; HCV RNA quantification, liver function, and routine blood test results were measured; liver transient elastography and abdominal ultrasound were performed at the same time. RPR, PLR, NLR, fibrosis-4 (FIB-4), and aspartate aminotransferase-to-platelet ratio index (APRI) were calculated. The Mann-Whiney U test was used for comparison between groups. The chi-square test was used for comparison of categorical data between groups. The receiver operating characteristic (ROC) curve was plotted to determine the optimal cut-off values of RPR and PLR. A multivariate unconditional logistic regression analysis was used to investigate the risk factors for CHC-related liver cirrhosis. The linear regression trend test was used to investigate the changing trend of RPR, PLR, FIB-4, and APRI in hepatitis C patients with different fibrosis stages. Results A total of 968 CHC patients were enrolled, among whom 123 (12.7%) were diagnosed with compensated liver cirrhosis (liver cirrhosis group). Compared with the CHC group, the liver cirrhosis group had a significant increase in RPR and a significant reduction in PLR (P < 0.001). The multivariate logistic regression analysis showed that age > 60 years (odds ratio [OR]=1.79, 95% confidence interval [CI]: 1.12-2.86, P=0.015), albumin < 40 g/L (OR=10.40, 95% CI: 3.47-31.18, P < 0.001), RPR > 0.081 (OR=3.83, 95% CI: 2.19-6.69, P < 0.001), PLR < 91.11 (OR=2.25, 95% CI: 1.31-3.89, P=0.004), FIB-4 > 3.25 (OR=3.14, 95% CI: 1.74-5.67, P < 0.001), and APRI > 2 (OR=3.60, 95% CI: 1.10-11.78, P=0.035) were associated with the development of CHC-related compensated liver cirrhosis. With the aggravation of liver fibrosis, RPR, FIB-4, and APRI gradually increased and PLR gradually decreased (all P < 0.001). Conclusion RPR and PLR are associated with the development and fibrosis progression of CHC-related compensated liver cirrhosis. Elderly patients with CHC (age > 60 years) should be monitored for the changes in albumin and liver fibrosis indicators, and RPR and PLR should also be monitored regularly to identify liver cirrhosis in the early stage, give timely treatment, and reduce the incidence rate of liver cancer. -
Key words:
- Hepatitis C /
- Liver Cirrhosis /
- Red Blood Cell /
- Mean Platelet Volume /
- Neutrophil-Lymphocyte Ratio
-
表 1 慢性丙型肝炎肝硬化发生的单因素分析
指标 例数 发生肝硬化[例(%)] χ2值 P值 性别 1.047 0.306 男 506 59(11.7) 女 462 64(13.9) 年龄 11.543 0.001 ≤60岁 539 51(9.5) >60岁 429 72(16.8) 教育水平 0.056 0.814 初中及以下 892 114(12.8) 高中及以上 76 9(11.8) BMI 1.786 0.618 低体重 42 4(9.5) 正常 444 63(14.2) 超重 359 42(11.7) 肥胖 123 14(11.4) 吸烟指数 1.288 0.256 <40包/年 870 107(12.3) ≥40包/年 98 16(16.3) 体育锻炼 0.294 0.588 否 458 61(13.3) 是 510 62(12.2) 一级亲属肝病史 0.970 0.325 无 847 111(13.1) 有 121 12(9.9) 治疗情况 0.032 0.984 未治疗 252 32(12.7) 抗病毒治疗 687 87(12.7) 治疗方案不明 29 4(13.8) HCV RNA 0.042 0.838 阴性 700 88(12.6) 阳性 268 35(13.1) 表 2 慢性丙型肝炎患者与丙型肝炎相关肝硬化患者血清学指标比较
指标 慢性丙型肝炎组(n=845) 丙型肝炎肝硬化组(n=123) U值 P值 WBC(×109/L) 5.89(4.88~7.10) 5.07(4.22~6.20) 37 138.0 <0.001 淋巴细胞数量(×109/L) 1.99(1.58~2.44) 1.71(1.27~2.23) 40 228.0 <0.001 中性粒细胞数量(×109/L) 3.39(2.64~4.26) 2.83(2.25~3.73) 40 107.0 <0.001 血小板(×109/L) 193(162~225) 123(86~169) 21 421.0 <0.001 AST(U/L) 22.7(19.0~28.9) 29.5(24.2~47.1) 27 690.0 <0.001 ALT(U/L) 18.7(13.4~27.4) 22.9(17.1~41.4) 37 433.0 <0.001 AAR 1.22(0.97~1.51) 1.31(1.02~1.59) 46 912.0 0.092 GGT(U/L) 23.0(15.5~36.0) 33.0(21.0~76.0) 35 655.0 <0.001 TBil(μmol/L) 10.0(7.5~13.1) 13.7(9.2~18.9) 33 935.0 <0.001 红细胞分布宽度(%) 12.7(12.3~13.1) 13.0(12.5~13.8) 37 824.0 <0.001 血红蛋白(g/L) 151(141~161) 145(136~157) 41 863.5 <0.001 白蛋白(g/L) 47.3(45.4~49.2) 44.6(42.4~46.9) 28 669.5 <0.001 总蛋白(g/L) 76.7(73.8~80.1) 76.7(73.7~81.3) 50 408.0 0.590 RPR 0.066(0.057~0.078) 0.108(0.078~0.153) 20 130.0 <0.001 PLR 96.67(74.37~126.25) 73.00(52.25~90.37) 29 626.0 <0.001 NLR 1.69(1.27~2.35) 1.84(1.29~2.56) 49 498.5 0.394 FIB-4 1.68(1.27~2.16) 3.38(2.16~5.84) 18 416.0 <0.001 APRI 0.33(0.25~0.45) 0.75(0.42~1.52) 20 084.5 <0.001 表 3 慢性丙型肝炎肝硬化发生的多因素分析
因素 OR值 95% CI P值 年龄(>60岁vs ≤60岁) 1.79 1.12~2.86 0.015 白蛋白(<40 g/L vs ≥40 g/L) 10.40 3.47~31.18 <0.001 RPR(>0.081 vs ≤0.081) 3.83 2.19~6.69 <0.001 PLR(<91.11 vs ≥91.11) 2.25 1.31~3.89 0.004 FIB~4(>3.25 vs ≤3.25) 3.14 1.74~5.67 <0.001 APRI(>2 vs ≤2) 3.60 1.10~11.78 0.035 表 4 RPR、PLR与肝纤维化严重程度之间的关系
指标 F0~1 F2 F2~3 F3~4 F4 P值 RPR 0.07(0.05~0.08) 0.07(0.06~0.09) 0.08(0.07~0.12) 0.09(0.07~0.12) 0.13(0.09~0.22) <0.001 PLR 99.3(77.3~129.8) 90.3(68.0~115.0) 88.7(58.7~119.8) 76.0(60.6~90.5) 62.4(49.4~88.6) <0.001 FIB-4 1.62(1.25~2.07) 1.88(1.39~2.68) 2.64(1.87~3.43) 3.26(2.20~4.64) 3.91(2.71~7.06) <0.001 APRI 0.31(0.24~0.41) 0.41(0.29~0.58) 0.58(0.37~0.78) 0.81(0.49~1.37) 1.10(0.51~1.78) <0.001 -
[1] CHEN YS, LI L, CUI FQ, et al. A sero-epidemiological study on hepatitis C in China[J]. Chin J Epidemiol, 2011, 32(9): 888-891. DOI: 10.3760/cma.j.issn.0254-6450.2011.09.009.陈园生, 李黎, 崔富强, 等. 中国丙型肝炎血清流行病学研究[J]. 中华流行病学杂志, 011, 2(9): 888-891. DOI: 10.3760/cma.j.issn.0254-6450.2011.09.009. [2] DUAN Z, JIA JD, HOU J, et al. Current challenges and the management of chronic hepatitis C in mainland China[J]. J Clin Gastroenterol, 2014, 48(8): 679-686. DOI: 10.1097/MCG.0000000000000109. [3] MCGLYNN KA, PETRICK JL, EL-SERAG HB. Epidemiology of hepatocellular carcinoma[J]. Hepatology, 2021, 73(Suppl 1): 4-13. DOI: 10.1002/hep.31288. [4] FATTOVICH G, STROFFOLINI T, ZAGNI I, et al. Hepatocellular carcinoma in cirrhosis: Incidence and risk factors[J]. Gastroenterology, 2004, 127(5 Suppl 1): s35-s50. DOI: 10.1053/j.gastro.2004.09.014. [5] KUMAR R, TEO EK, HOW CH, et al. A practical clinical approach to liver fibrosis[J]. Singapore Med J, 2018, 59(12): 628-633. DOI: 10.11622/smedj.2018145. [6] GRGUREVIC I, BOZIN T, MADIR A. Hepatitis C is now curable, but what happens with cirrhosis and portal hypertension afterwards?[J]. Clin Exp Hepatol, 2017, 3(4): 181-186. DOI: 10.5114/ceh.2017.71491. [7] KONG Y, SUN Y, ZHOU J, et al. Early steep decline of liver stiffness predicts histological reversal of fibrosis in chronic hepatitis B patients treated with entecavir[J]. J Viral Hepat, 2019, 26(5): 576-585. DOI: 10.1111/jvh.13058. [8] STASI C, MILANI S. Evolving strategies for liver fibrosis staging: Non-invasive assessment[J]. World J Gastroenterol, 2017, 23(2): 191-196. DOI: 10.3748/wjg.v23.i2.191. [9] CARMONA I, CORDERO P, AMPUERO J, et al. Role of assessing liver fibrosis in management of chronic hepatitis C virus infection[J]. Clin Microbiol Infect, 2016, 22(10): 839-845. DOI: 10.1016/j.cmi.2016.09.017. [10] ZHENG J, CAI J, LI H, et al. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as prognostic predictors for hepatocellular carcinoma patients with various treatments: A Meta-analysis and systematic review[J]. Cell Physiol Biochem, 2017, 44(3): 967-981. DOI: 10.1159/000485396. [11] STOJKOVIC LALOSEVIC M, PAVLOVIC MARKOVIC A, STANKOVIC S, et al. Combined diagnostic efficacy of neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and mean platelet volume (MPV) as biomarkers of systemic inflammation in the diagnosis of colorectal cancer[J]. Dis Markers, 2019, 2019: 6036979. DOI: 10.1155/2019/6036979. [12] PAN YC, JIA ZF, CAO DH, et al. Preoperative lymphocyte-to-monocyte ratio (LMR) could independently predict overall survival of resectable gastric cancer patients[J]. Medicine (Baltimore), 2018, 97(52): e13896. DOI: 10.1097/MD.0000000000013896. [13] LAI Q, CASTRO SANTA E, RICO JURI JM, et al. Neutrophil and platelet-to-lymphocyte ratio as new predictors of dropout and recurrence after liver transplantation for hepatocellular cancer[J]. Transpl Int, 2014, 27(1): 32-41. DOI: 10.1111/tri.12191. [14] LIN L, YANG F, WANG Y, et al. Prognostic nomogram incorporating neutrophil-to-lymphocyte ratio for early mortality in decompensated liver cirrhosis[J]. Int Immunopharmacol, 2018, 56: 58-64. DOI: 10.1016/j.intimp.2018.01.007. [15] MILAS GP, KARAGEORGIOU V, CHOLONGITAS E. Red cell distribution width to platelet ratio for liver fibrosis: A systematic review and meta-analysis of diagnostic accuracy[J]. Expert Rev Gastroenterol Hepatol, 2019, 13(9): 877-891. DOI: 10.1080/17474124.2019.1653757. [16] MENG X, WEI G, CHANG Q, et al. The platelet-to-lymphocyte ratio, superior to the neutrophil-to-lymphocyte ratio, correlates with hepatitis C virus infection[J]. Int J Infect Dis, 2016, 45: 72-77. DOI: 10.1016/j.ijid.2016.02.025. [17] ZHAO Z, LIU J, WANG J, et al. Platelet-to-lymphocyte ratio (PLR) and neutrophil-to-lymphocyte ratio (NLR) are associated with chronic hepatitis B virus (HBV) infection[J]. Int Immunopharmacol, 2017, 51: 1-8. DOI: 10.1016/j.intimp.2017.07.007. [18] PENG Y, LI Y, HE Y, et al. The role of neutrophil to lymphocyte ratio for the assessment of liver fibrosis and cirrhosis: a systematic review[J]. Expert Rev Gastroenterol Hepatol, 2018, 12(5): 503-513. DOI: 10.1080/17474124.2018.1463158. [19] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Guidelines for the prevention and treatment of hepatitis C (2019 version)[J]. J Clin Hepatol, 2019, 35(12): 2670-2686. DOI: 10.3969/j.issn.1001-5256.2019.12.008.中华医学会肝病学分会, 中华医学会感染病学分会. 丙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35(12): 2670-2686. DOI: 10.3969/j.issn.1001-5256.2019.12.008. [20] Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006.中华医学会肝病学分会. 肝硬化诊治指南[J]. 临床肝胆病杂志, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. [21] TSOCHATZIS EA, BOSCH J, BURROUGHS AK. Liver cirrhosis[J]. Lancet, 2014, 383(9930): 1749-1761. DOI: 10.1016/S0140-6736(14)60121-5. [22] D'AMICO G, GARCIA-TSAO G, PAGLIARO L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies[J]. J Hepatol, 2006, 44(1): 217-231. DOI: 10.1016/j.jhep.2005.10.013. [23] YANG M, PARIKH ND, LIU H, et al. Incidence and risk factors of hepatocellular carcinoma in patients with hepatitis C in China and the United States[J]. Sci Rep, 2020, 10(1): 20922. DOI: 10.1038/s41598-020-77515-y. [24] BIAN DD, JIANG YY, ZHOU HY, et al. Current status of antiviral therapy for hepatitis C related cirrhosis and hepatocellular carcinoma in mainland China[J]. Chin J Gastroenterol Hepatol, 2019, 28(7): 750-754. DOI: 10.3969/j.issn.1006-5709.2019.07.007.卞丹丹, 蒋莹莹, 周海洋, 等. 中国大陆丙肝相关肝硬化及肝癌患者抗病毒治疗现状调查[J]. 胃肠病学和肝病学杂志, 2019, 28(7): 750-754. DOI: 10.3969/j.issn.1006-5709.2019.07.007. [25] CAO MM, CHEN WQ. Research progress of liver cancer screening[J]. China Cancer, 2020, 29(12): 925-932. DOI: 10.11735/j.issn.1004-0242.2020.12.A007.曹毛毛, 陈万青. 肝癌筛查研究进展[J]. 中国肿瘤, 2020, 29(12): 925-932. DOI: 10.11735/j.issn.1004-0242.2020.12.A007. [26] LIPPI G, PLEBANI M. Red blood cell distribution width (RDW) and human pathology. One size fits all[J]. Clin Chem Lab Med, 2014, 52(9): 1247-1249. DOI: 10.1515/cclm-2014-0585. [27] TEKCE H, KIN TEKCE B, AKTAS G, et al. The evaluation of red cell distribution width in chronic hemodialysis patients[J]. Int J Nephrol, 2014, 2014: 754370. DOI: 10.1155/2014/754370. [28] JELKMANN W. Proinflammatory cytokines lowering erythropoietin production[J]. J Interferon Cytokine Res, 1998, 18(8): 555-559. DOI: 10.1089/jir.1998.18.555. [29] WANG ZD, WU H. Pathogenesis and treatment of thrombocytopenia in patients with liver cirrhosis[J]. Prac J Clin Med, 2020, 17(1): 212-215. DOI: 10.3969/j.issn.1672-6170.2020.01.065.王治东, 吴浩. 肝硬化患者血小板减少的发病机制及治疗[J]. 实用医院临床杂志, 2020, 17(1): 212-215. DOI: 10.3969/j.issn.1672-6170.2020.01.065. [30] KUROKAWA T, OHKOHCHI N. Platelets in liver disease, cancer and regeneration[J]. World J Gastroenterol, 2017, 23(18): 3228-3239. DOI: 10.3748/wjg.v23.i18.3228. [31] LI X, XU H, GAO P. Red Blood Cell Distribution width-to-platelet ratio and other laboratory indices associated with severity of histological hepatic fibrosis in patients with autoimmune hepatitis: A retrospective study at a single center[J]. Med Sci Monit, 2020, 26: e927946. DOI: 10.12659/MSM.927946. [32] HE Q, HE Q, QIN X, et al. The relationship between inflammatory marker levels and hepatitis C virus severity[J]. Gastroenterol Res Pract, 2016, 2016: 2978479. DOI: 10.1155/2016/2978479. [33] GOMEZ D, FARID S, MALIK HZ, et al. Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma[J]. World J Surg, 2008, 32(8): 1757-1762. DOI: 10.1007/s00268-008-9552-6. [34] LI X, WANG L, GAO P. Chronic hepatitis C virus infection: Relationships between inflammatory marker levels and compensated liver cirrhosis[J]. Medicine (Baltimore), 2019, 98(39): e17300. DOI: 10.1097/MD.0000000000017300. [35] ABDEL-RAZIK A, MOUSA N, BESHEER T A, et al. Neutrophil to lymphocyte ratio as a reliable marker to predict insulin resistance and fibrosis stage in chronic hepatitis C virus infection[J]. Acta Gastroenterol Belg, 2015, 78(4): 386-392. DOI: 10.1109/APS.2006.1711016. 期刊类型引用(11)
1. 阳丽华,梁英,刘仁峰,刘志昂. 甲状腺癌与甲状腺肿患者相关实验室指标的比较分析. 甘肃医药. 2025(01): 53-55+59 .  百度学术
百度学术2. 张海苗. HBV感染原发性肝癌患者血常规指标的检测意义. 包头医学院学报. 2024(02): 67-71 .  百度学术
百度学术3. 戴倩梅,丁体龙,代雪枫,于莉,陈策. 高敏丙型肝炎病毒核糖核酸在丙型肝炎中的诊断价值. 检验医学与临床. 2024(04): 487-490 .  百度学术
百度学术4. 李晓宇,黄秀香,叶迎宾. 血清壳多糖酶3样蛋白1和PLT的比值与FIB-4指数在慢性乙型肝炎轻、中度诊断效价的比较. 标记免疫分析与临床. 2024(09): 1693-1697 .  百度学术
百度学术5. 何萍,徐瑞,华秋菊,姜璐,王维平. 红细胞分布宽度与血小板比值对终末期肾病维持性血液透析患者动静脉内瘘失功的预测分析. 中国医师进修杂志. 2024(11): 988-994 .  百度学术
百度学术6. 岳丽,孙佳瑶,刘龙芳. 脑小血管病患者外周血GPR30 mRNA、PLR、NPAS4表达及与认知功能、短期预后的关系. 临床误诊误治. 2023(01): 69-74 .  百度学术
百度学术7. 杨杨,刘付弟,曾方林. 人类免疫缺陷病毒/乙型肝炎病毒合并感染者CD4~+T细胞计数和乙型肝炎病毒复制、中性粒细胞与淋巴细胞比值水平的相关性. 中国医药导报. 2023(10): 145-148 .  百度学术
百度学术8. 王跃帮,常珊碧,王梦林,崔倩,裴兵. RLR在HBV相关性肝硬化诊断中的应用. 热带医学杂志. 2023(10): 1451-1455 .  百度学术
百度学术9. 邱建华. PLT联合凝血功能检测对早期肝硬化的诊断价值分析. 现代诊断与治疗. 2023(22): 3433-3435 .  百度学术
百度学术10. 赵霄君,谢建刚,段楚君,刘善收,王倩梅,思艺,王林潇,吴丹,王一帆,李俊杰. 血常规指标与脓毒症患者短期预后的相关性研究. 临床误诊误治. 2022(08): 73-77 .  百度学术
百度学术11. 邵林楠,张树婷,王霓,周世航,刘铭. 血细胞各比值对慢性丙型肝炎病毒患者肝纤维化程度的评估. 临床血液学杂志. 2022(12): 874-877 .  百度学术
百度学术其他类型引用(7)
-




 PDF下载 ( 1977 KB)
PDF下载 ( 1977 KB)

 下载:
下载:

 百度学术
百度学术

