改良客观性BISAP评分对急性胰腺炎严重程度及预后的预测价值
DOI: 10.3969/j.issn.1001-5256.2021.06.032
Value of modified objective Bedside Index for Severity in Acute Pancreatitis score in predicting the severity and prognosis of acute pancreatitis
-
摘要:
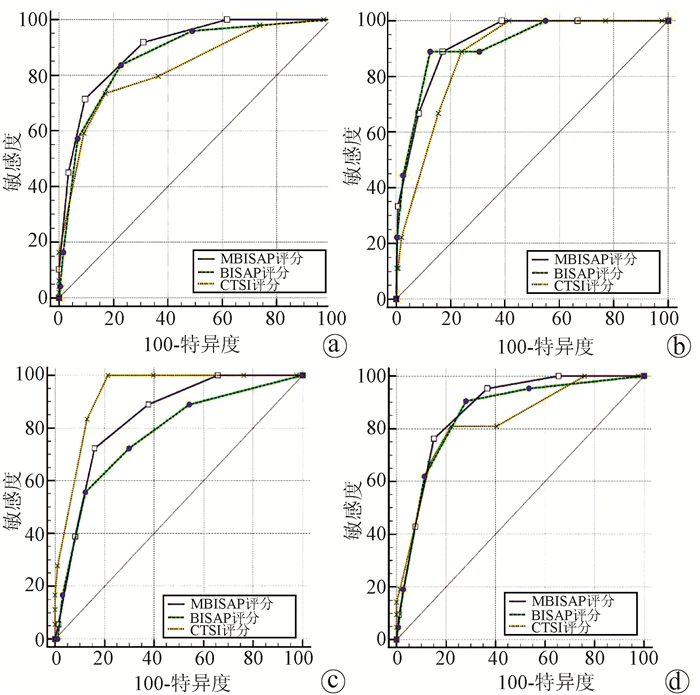
目的 探讨改良客观性BISAP评分(MBISAP)对急性胰腺炎(AP)严重程度及预后的预测价值。 方法 回顾性分析2018年6月—2020年6月川北医学院附属医院收治的313例AP患者资料,将BISAP评分中精神状态这一主观性指标去除,再根据CTSI(CT严重指数)评分标准,将胰腺坏死程度分为4类(0、0~30%、30%~50%、>50%),并给予相应的赋值(0~3分),MBISAP评分由上述指标赋值相加可得,最高为7分。根据受试者工作特征(ROC)曲线将313例胰腺炎患者分为MBISAP低级别组(MBISAP<3分)和MBISAP高级别组(MBISAP≥3分)2组。比较2组基线资料、临床结局,非正态分布的计量资料2组间比较采用Mann-Whitney U秩和检验;计数资料2组间比较采用χ2检验或Fisher精确检验。ROC曲线下面积(AUC)分析比较MBISAP评分、BISAP评分、CTSI评分对AP病情严重程度、预后的预测价值。 结果 2组患者在年龄(Z=-5.480,P<0.001)、病因(χ2=36.536,P<0.001)、住院时间(Z=-6.038,P<0.001)、病死率(P<0.001)、胰周感染(P<0.001)、多器官功能障碍综合征(MODS)(P<0.001)、BISAP评分(χ2=215.320, P<0.001)、CTSI评分(P<0.001)之间存在明显差异。随着MBISAP评分的增加,AP病情严重程度、病死率、胰周感染、MODS的发生呈增加趋势(P值均<0.001)。在预测SAP方面,MBISAP评分AUC=0.898(95%CI: 0.859~0.929,P<0.001),敏感度为71.43%,特异度为90.53%;当MBISAP≥3时为最佳临界值,优于BISAP评分(AUC=0.868,P<0.05)、CTSI评分(AUC=0.827,P<0.05)。在预测AP患者死亡方面,MBISAP评分AUC=0.925(95%CI: 0.890~0.952,P<0.001),敏感度为88.89%,特异度为82.89%;当MBISAP≥3时为最佳临界值,与BISAP评分(AUC=0.915,P>0.05)、CTSI评分(AUC=0.879,P>0.05)相似。在预测AP胰周感染方面,MBISAP评分AUC=0.842(95%CI: 0.796~0.880,P<0.001),敏感度为72.22%,特异度为84.07%;当MBISAP>2时为最佳临界值,优于BISAP评分(AUC= 0.776,P<0.05),但比CTSI评分(AUC=0.932,P<0.05)较差。在预测AP患者合并MODS方面,MBISAP评分AUC=0.874(95%CI: 0.832~0.909,P<0.001),敏感度为76.19%,特异度为84.93%,当MBISAP>2时为最佳临界值,与BISAP评分(AUC=0.855,P>0.05)、CTSI评分(AUC=0.829,P>0.05)相似。 结论 MBISAP评分在预测AP患者的严重程度及胰周感染方面优于BISAP评分,预测AP患者死亡及MODS方面也有较好的价值,相比BISAP评分能够更准确、客观地评估AP患者情况。 Abstract:Objective To investigate the value of modified objective Bedside Index for Severity in Acute Pancreatitis (BISAP) score (MBISAP) in predicting the severity and prognosis of acute pancreatitis (AP). Methods A retrospective analysis was performed for the data of 313 patients with AP who were treated in Affiliated Hospital of North Sichuan Medical College from June 2018 to June 2020, and the subjective indicator of mental state in BISAP score was removed. According to the scoring criteria for Computed Tomography Severity Index (CTSI), the degree of pancreatic necrosis was classified as 4 grades (0%, 0%-30%, 30%-50%, and > 50%) and was assigned a score of 0-3 points, respectively, and MBISAP score was determined by adding the above points, with the highest score of 7 points. According to the receiver operating characteristic (ROC) curve, the 313 patients with pancreatitis were divided into low-level MBISAP group (MBISAP < 3) and high-level MBISAP group (MBISAP ≥3). The two groups were compared in terms of baseline data and clinical outcome. The Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups, and the chi-square test or the Fisher's exact test was used for comparison of categorical data between two groups. The area under the ROC curve (AUC) was used to analyze an compare the value of MBISAP score, BISAP score, and CTSI score in predicting the severity and prognosis of AP. Results There were significant differences between the two groups in age (Z=-5.480, P < 0.001), etiology (χ2=36.536, P < 0.001), length of hospital stay (Z=-6.038, P < 0.001), mortality rate (P < 0.001), peripancreatic infection (P < 0.001), multiple organ dysfunction syndrome (MODS) (P < 0.001), BISAP score (χ2=215.320, P < 0.001), and CTSI score (P < 0.001). Severity of AP, mortality rate, and incidence rates of peripancreatic infection and MODS tended to increase with the increase in MBISAP score (P < 0.001). In predicting severe AP, MBISAP score had an AUC of 0.898 (95% confidence interval [CI]: 0.859-0.929, P < 0.001), with a sensitivity of 71.43% and a specificity of 90.53%; at the optimal cut-off value of ≥3, MBISAP score was significantly better than BISAP score (AUC=0.868) and CTSI score (AUC=0.827) (both P < 0.05). In predicting the mortality of patients with AP, MBISAP score had an AUC of 0.925 (95% CI: 0.890-0.952, P < 0.001), with a sensitivity of 88.89% and a specificity of 82.89%; at the optimal cut-off value of ≥3, MBISAP score was similar to BISAP score (AUC=0.915) and CTSI score (AUC=0.879) (both P > 0.05). In predicting peripancreatic infection in AP, MBISAP score had an AUC of 0.842 (95% CI: 0.796-0.880, P < 0.001), with a sensitivity of 72.22% and a specificity of 84.07%; at the optimal cut-off value of > 2, MBISAP score was better than BISAP score (AUC=0.776) and was inferior to CTSI score (AUC=0.932) (both P < 0.05). In predicting MODS in patients with AP, MBISAP score had an AUC of 0.874 (95% CI: 0.832-0.909, P < 0.001), with a sensitivity of 76.19% and a specificity of 84.93%; at the optimal cut-off value of > 2, MBISAP score was similar to BISAP score (AUC=0.855) and CTSI score (AUC=0.829) (both P > 0.05). Conclusion MBISAP score is better than BISAP score in predicting the severity of AP patients and peripancreatic infection, and it also has a good value in predicting mortality and MODS in patients with AP. MBISAP score can evaluate the conditions of AP patients more accurately and objectively than BISAP score. -
Key words:
- Pancreatitis /
- BISAP Score /
- CTSI Score
-
表 1 MBISAP评分系统赋值表
变量 0分 1分 2分 3分 尿素氮(mmol/L) ≤9 >9 SIRS 无 有 年龄(岁) ≤60 >60 胸腔积液 无 有 胰腺坏死面积 0 0~30% 30%~50% >50% 注:SIRS,全身炎症反应综合征。至少具备以下2项确诊:(1)体温<36 ℃/>38 ℃;(2)呼吸频率>20次/min或PCO2<32 mm Hg;(3)脉搏>90次/min;(4)WBC>12×109/L或<4×109/L。 表 2 2组患者基线资料比较
项目 MBISAP低级别组(n=253) MBISAP高级别组(n=60) 统计值 P值 年龄(岁) 49.0(41.0~57.5) 62.5(52.25~73.75) Z=-5.480 <0.001 性别[男(%)] 141(55.73) 28(46.67) χ2=1.604 0.205 吸烟[例(%)] 59(23.32) 21(35.00) χ2=3.477 0.062 饮酒[例(%)] 60(23.72) 19(31.67) χ2=1.625 0.202 糖尿病[例(%)] 46(18.18) 15(25.00) χ2=1.437 0.231 高血压[例(%)] 50(19.76) 13(21.67) χ2=0.109 0.741 病因[例(%)] χ2=36.536 <0.001 胆源性 111(43.87) 45(75.00) 高脂血症 89(35.18) 5(8.33) 酒精 25(9.88) 0 饮食 16(6.32) 1(1.67) 不祥 12(4.74) 9(15.00) 住院时间(d) 10.00(7.00~13.00) 16.00(12.00~20.75) Z=-6.038 <0.001 死亡[例(%)] 1(0.40) 8(13.33) <0.001 胰周感染[例(%)] 5(1.98) 13(21.67) <0.001 MODS[例(%)] 5(1.98) 16(26.67) <0.001 BISAP评分(轻/重,例) 252/1 15/45 χ2=215.320 <0.001 CTSI评分(轻/中/重,例) 215/38/0 17/42/1 <0.001 表 3 根据MBISAP评分分层的SAP、病死率、胰周感染、MODS患者数量及其比例
MBISAP评分 总例数 SAP[例(%)] 死亡[例(%)] 胰周感染[例(%)] MODS[例(%)] 0分 101 0 0 0 0 1分 85 4(4.71) 0 2(2.35) 1(1.18) 2分 67 10(14.93) 1(1.49) 3(4.48) 4(5.97) 3分 29 13(44.83) 2(6.90) 6(20.70) 7(24.14) 4分 26 17(65.38) 3(11.54) 6(23.08) 7(26.92) 5分 5 5(100) 3(60.00) 1(20.00) 2(40.00) 6分 0 7分 0 表 4 根据BISAP评分分层的SAP、病死率、胰周感染、MODS患者数量及其比例
BISAP评分 总例数 SAP[例(%)] 死亡[例(%)] 胰周感染[例(%)] MODS[例(%)] 轻(0~2分) 267 21(7.87) 1(0.37) 8(3.00) 8(3.00) 重(3~5分) 46 28(60.87) 8(17.39) 10(21.74) 13(28.26) 表 5 根据CTSI评分分层的SAP、病死率、胰周感染、MODS患者数量及其比例
CTSI评分 总例数 SAP[例(%)] 死亡[例(%)] 胰周感染[例(%)] MODS[例(%)] 轻(0~3分) 232 13(5.60) 1(0.43) 0 4(1.72) 中(4~6分) 80 35(43.75) 7(8.75) 17(21.25) 16(20.00) 重(7~10分) 1 1(100) 1(100) 1(100) 1(100) 表 6 MBISAP评分与BISAP、CTSI评分系统对AP严重程度及预后的预测效果比较
项目 AUC 95%CI 敏感度(%) 特异度(%) 最佳临界值 约登指数 P值 SAP MBISAP评分 0.898 0.859~0.929 71.43 90.53 ≥3 0.620 <0.001 BISAP评分 0.868 0.826~0.904 83.67 77.27 ≥2 0.610 <0.001 CTSI评分 0.827 0.780~0.867 73.47 82.95 >3 0.564 <0.001 死亡 MBISAP评分 0.925 0.890~0.952 88.89 82.89 ≥3 0.718 <0.001 BISAP评分 0.915 0.879~0.944 88.89 87.50 ≥3 0.764 <0.001 CTSI评分 0.879 0.838~0.913 88.89 75.99 >3 0.649 <0.001 胰周感染 MBISAP评分 0.842 0.796~0.880 72.22 84.07 >2 0.563 <0.001 BISAP评分 0.776 0.726~0.821 55.56 87.80 ≥3 0.434 <0.001 CTSI评分 0.932 0.902~0.960 100.00 78.64 >3 0.786 <0.001 MODS MBISAP评分 0.874 0.832~0.909 76.19 84.93 >2 0.611 <0.001 BISAP评分 0.855 0.811~0.892 90.48 71.92 ≥2 0.624 <0.001 CTSI评分 0.829 0.782~0.869 80.95 78.08 ≥4 0.590 <0.001 -
[1] HUBER W, PHILLIP V, SCHMID R, et al. Acute Pancreatitis: What is new?[J]. Dtsch Med Wochenschr, 2017, 142(7): 525-529. DOI: 10.1055/s-0042-100233. [2] VEGE SS, GARDNER TB, CHARI ST, et al. Low mortality and high morbidity in severe acute pancreatitis without organ failure: A case for revising the Atlanta classification to include "moderately severe acute pancreatitis"[J]. Am J Gastroenterol, 2009, 104(3): 710-715. DOI: 10.1038/ajg.2008.77. [3] GUDA NM, TRIKUDANATHAN G, FREEMAN ML. Idiopathic recurrent acute pancreatitis[J]. Lancet Gastroenterol Hepatol, 2018, 3(10): 720-728. DOI: 10.1016/S2468-1253(18)30211-5. [4] WANG L, ZENG YB, CHEN JY, et al. A simple new scoring system for predicting the mortality of severe acute pancreatitis: A retrospective clinical study[J]. Medicine (Baltimore), 2020, 99(23): e20646. DOI: 10.1097/MD.0000000000020646. [5] Pancreas Study Group, Chinese Society of Gastroenterology, Chinese Medical Association; Editorial Board of Chinese Journal of Pancreatology; Editorial Board of Chinese Journal of Digestion. Chinese guidelines for the management of acute pancreatitis (Shengyang, 2019)[J]. J Clin Hepatol, 2019, 35(12): 2706-2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013.中华医学会消化病学分会胰腺疾病学组, 《中华胰腺病杂志》编委会, 《中华消化杂志》编委会. 中国急性胰腺炎诊治指南(2019年, 沈阳)[J]. 临床肝胆病杂志, 2019, 35(12): 2706-2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013. [6] WU BU, JOHANNES RS, SUN X, et al. The early prediction of mortality in acute pancreatitis: A large population-based study[J]. Gut, 2008, 57(12): 1698-1703. DOI: 10.1136/gut.2008.152702. [7] ALHAJERI A, ERWIN S. Acute pancreatitis: Value and impact of CT severity index[J]. Abdom Imaging, 2008, 33(1): 18-20. DOI: 10.1007/s00261-007-9315-0. [8] XU HF, LI Y, YAN J, et al. Severity analysis of acute pancreatitis based on etiology[J]. Natal Med J China, 2014, 94(41): 3220-3223. DOI: 10.3760/cma.j.issn.0376-2491.2014.41.005.徐海峰, 李勇, 颜骏, 等. 急性胰腺炎病因与其严重程度的关系[J]. 中华医学杂志, 2014, 94(41): 3220-3223. DOI: 10.3760/cma.j.issn.0376-2491.2014.41.005. [9] CHEN HJ, WANG JJ, TSAY WI, et al. Epidemiology and outcome of acute pancreatitis in end-stage renal disease dialysis patients: A 10-year national cohort study[J]. Nephrol Dial Transplant, 2017, 32(10): 1731-1736. DOI: 10.1093/ndt/gfw400. [10] GARG PK, SINGH VP. Organ failure due to systemic injury in acute pancreatitis[J]. Gastroenterology, 2019, 156(7): 2008-2023. DOI: 10.1053/j.gastro.2018.12.041. [11] CHEN FY, BAI XY, WU D. The severity scoring system and prognostic biological markers of acute pancreatitis[J]. Chin J Intern Med, 2019, 58(8): 615-619. DOI: 10.3760/cma.j.issn.0578-1426.2019.08.016.陈方莹, 柏小寅, 吴东. 预测急性胰腺炎严重程度的评分系统及生物标志物[J]. 中华内科杂志, 2019, 58(8): 615-619. DOI: 10.3760/cma.j.issn.0578-1426.2019.08.016. [12] TAN Y, RAFI S, TYEBALLY FANG M, et al. Validation of the modified Ranson versus Glasgow score for pancreatitis in a Singaporean population[J]. ANZ J Surg, 2017, 87(9): 700-703. DOI: 10.1111/ans.13139. [13] KNOEPFLI AS, KINKEL K, BERNEY T, et al. Prospective study of 310 patients: Can early CT predict the severity of acute pancreatitis?[J]. Abdom Imaging, 2007, 32(1): 111-115. DOI: 10.1007/s00261-006-9034-y. [14] YE JF, ZHAO YX, JU J, et al. Building and verifying a severity prediction model of acute pancreatitis (AP) based on BISAP, MEWS and routine test indexes[J]. Clin Res Hepatol Gastroenterol, 2017, 41(5): 585-591. DOI: 10.1016/j.clinre.2016.11.013. [15] SAHU B, ABBEY P, ANAND R, et al. Severity assessment of acute pancreatitis using CT severity index and modified CT severity index: Correlation with clinical outcomes and severity grading as per the Revised Atlanta Classification[J]. Indian J Radiol Imaging, 2017, 27(2): 152-160. DOI: 10.4103/ijri.IJRI_300_16. [16] RIECHERS RG 2nd, RAMAGE A, BROWN W, et al. Physician knowledge of the Glasgow Coma Scale[J]. J Neurotrauma, 2005, 22(11): 1327-1334. DOI: 10.1089/neu.2005.22.1327. [17] BLEDSOE BE, CASEY MJ, FELDMAN J, et al. Glasgow coma scale scoring is often inaccurate[J]. Prehosp Disaster Med, 2015, 30(1): 46-53. DOI: 10.1017/S1049023X14001289. [18] HEIM C, SCHOETTKER P, GILLIARD N, et al. Knowledge of Glasgow coma scale by air-rescue physicians[J]. Scand J Trauma Resusc Emerg Med, 2009, 17: 39. DOI: 10.1186/1757-7241-17-39. [19] YANG YX, LI L. Evaluating the ability of the bedside index for severity of acute pancreatitis score to predict severe acute pancreatitis: A meta-analysis[J]. Med Princ Pract, 2016, 25(2): 137-142. DOI: 10.1159/000441003. [20] SENAPATI D, DEBATA PK, JENASAMANT SS, et al. A prospective study of the Bedside Index for Severity in Acute Pancreatitis (BISAP) score in acute pancreatitis: An Indian perspective[J]. Pancreatology, 2014, 14(5): 335-339. DOI: 10.1016/j.pan.2014.07.007. [21] HAGJER S, KUMAR N. Evaluation of the BISAP scoring system in prognostication of acute pancreatitis - A prospective observational study[J]. Int J Surg, 2018, 54(Pt A): 76-81. DOI: 10.1016/j.ijsu.2018.04.026. [22] HARSHIT KA, SINGH GM. A comparison of APACHE Ⅱ, BISAP, Ranson's score and modified CTSI in predicting the severity of acute pancreatitis based on the 2012 revised Atlanta Classification[J]. Gastroenterol Rep (Oxf), 2018, 6(2): 127-131. DOI: 10.1093/gastro/gox029. [23] BANDAY IA, GATTOO I, KHAN AM, et al. Modified computed tomography severity index for evaluation of acute pancreatitis and its correlation with clinical outcome: A tertiary care hospital based observational study[J]. J Clin Diagn Res, 2015, 9(8): TC01-TC05. DOI: 10.7860/JCDR/2015/14824.6368. [24] PETROV MS, SHANBHAG S, CHAKRABORTY M, et al. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis[J]. Gastroenterology, 2010, 139(3): 813-820. DOI: 10.1053/j.gastro.2010.06.010. [25] MOFIDI R, SUTTIE SA, PATIL PV, et al. The value of procalcitonin at predicting the severity of acute pancreatitis and development of infected pancreatic necrosis: Systematic review[J]. Surgery, 2009, 146(1): 72-81. DOI: 10.1016/j.surg.2009.02.013. 期刊类型引用(5)
1. 黄健佳,杨艳,万鑫,周光斌,陈晨,王飞兵,曹华斌. 血浆乳酸动态变化可作为母犬绝育术预后评估的重要参数. 中国兽医杂志. 2024(07): 136-143 .  百度学术
百度学术2. 葛孝定,刘斐. 乙型肝炎病毒相关慢加急性肝衰竭的MELD评分变化及意义. 中国现代医生. 2023(13): 15-18 .  百度学术
百度学术3. 殷春兰,赵瑞芹,付海燕,白革兰,程丽娟. 血脂及血乳酸在儿童CLD的表达水平及其临床意义. 川北医学院学报. 2023(06): 754-758+763 .  百度学术
百度学术4. 谢冰鑫,王娜. 免疫球蛋白联合肝功能指标检测在肝衰竭诊断和预后判断中的价值. 中国医药指南. 2022(10): 107-109 .  百度学术
百度学术5. 吴舒沁,吴倩,骆建军,蒋光伟,王黎鹏,邹春喜,杨箬箬,王晓霞,朱新新,孟威. 中心静脉血氧饱和度作为严重创伤低血容量休克患者容量复苏目标的生化指标的研究. 创伤外科杂志. 2021(12): 920-924 .  百度学术
百度学术其他类型引用(2)
-




 PDF下载 ( 2496 KB)
PDF下载 ( 2496 KB)

 下载:
下载:
 百度学术
百度学术

