非酒精性脂肪性肝病相关肝细胞癌的诊断和治疗
DOI: 10.3969/j.issn.1001-5256.2021.08.002
利益冲突声明:所有作者均声明不存在利益冲突。
作者贡献声明:颜士岩负责文献检索,撰写文章;范建高负责文章的整体指导、审核以及修改完善。
Diagnosis and treatment of hepatocellular carcinoma associated with nonalcoholic fatty liver disease
-
摘要: 全球大部分肝细胞癌(HCC)(>80%)主要因HBV或HCV慢性感染导致。在中国,高达80%的HCC是由HBV引起,但目前HBV相关HCC死亡率降低了30%。与此同时,肥胖、2型糖尿病和非酒精性脂肪性肝病正在取代肝炎病毒和酒精滥用成为HCC的重要致病因素,代谢功能障碍及其相关脂肪性肝病导致的HCC近年来有不断增加趋势。为此需要重视非酒精性脂肪性肝病相关HCC的诊断、治疗并探讨其可能的发病机制。Abstract: At present, the majority (> 80%) of hepatocellular carcinoma (HCC) cases in the world is mainly caused by chronic HBV or HCV infection, and in China, up to 80% of HCC cases are caused by HBV, but the mortality rate of HBV-related HCC has decreased by 30% recently. At the same time, obesity, type 2 diabetes, and nonalcoholic fatty liver disease (NAFLD) gradually replace hepatitis virus infection and alcohol abuse and have become the important pathogenic factors for HCC, and there is also a tendency of increase in HCC cases caused by metabolic dysfunction and fatty liver disease in recent years. For this reason, it is particularly important to investigate the diagnosis, treatment, and possible pathogenesis of HCC associated with NAFLD.
-
Key words:
- Non-Alcoholic Fatty Liver Disease /
- Carcinoma, Hepatocellular /
- Diagnosis /
- Therapeutics
-
表 1 NAFLD-HCC与其他原因引起的HCC患者的特征
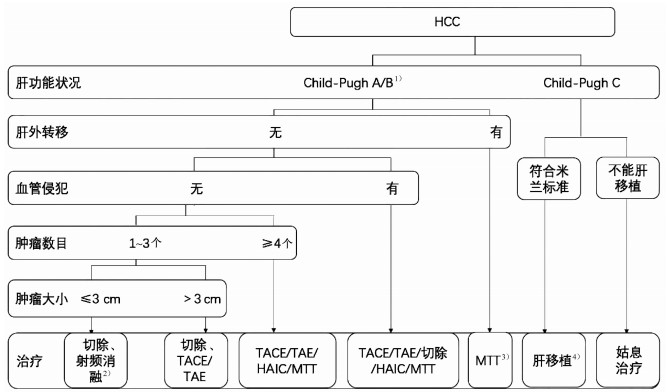
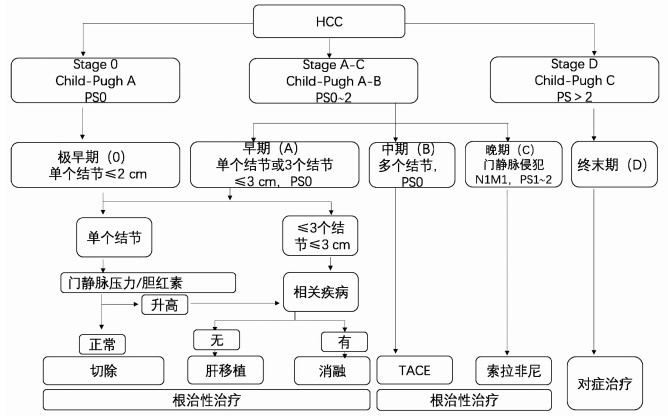
特征 NAFLD-HCC 其他原因引起的HCC 主要发生性别 男性 男性 诊断时年龄(岁) 65~70 60~65 代谢综合征(%) 45~58 14~18 2型糖尿病(%) 54~74 12~49 肥胖(%) 48~66 12~37 高血压(%) 47~60 18~52 血脂异常(%) 28~35 6~14 肝硬化的发生率(%) 51~62 78~97 肝功能状况 大多数尚可 较差 平均肿瘤大小(cm) ≥3 ≤3 肿瘤分化程度 高分化 高分化到中分化 -
[1] MARENGO A, ROSSO C, BUGIANESI E. Liver cancer: Connections with obesity, fatty liver, and cirrhosis[J]. Annu Rev Med, 2016, 67: 103-117. DOI: 10.1146/annurev-med-090514-013832. [2] PEISELER M, TACKE F. Inflammatory mechanisms underlying nonalcoholic steatohepatitis and the transition to hepatocellular carcinoma[J]. Cancers (Basel), 2021, 13(4): 730. DOI: 10.3390/cancers13040730. [3] MASSOUD O, CHARLTON M. Nonalcoholic fatty liver disease/nonalcoholic steatohepatitis and hepatocellular carcinoma[J]. Clin Liver Dis, 2018, 22(1): 201-211. DOI: 10.1016/j.cld.2017.08.014. [4] YOUNOSSI ZM, GOLABI P, DE AVILA L, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis[J]. J Hepatol, 2019, 71(4): 793-801. DOI: 10.1016/j.jhep.2019.06.021. [5] YOUNOSSI Z, STEPANOVA M, ONG JP, et al. Nonalcoholic steatohepatitis is the fastest growing cause of hepatocellular carcinoma in liver transplant candidates[J]. Clin Gastroenterol Hepatol, 2019, 17(4): 748-755. e3. DOI: 10.1016/j.cgh.2018.05.057. [6] ESTES C, RAZAVI H, LOOMBA R, et al. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease[J]. Hepatology, 2018, 67(1): 123-133. DOI: 10.1002/hep.29466. [7] YOUNOSSI ZM, OTGONSUREN M, HENRY L, et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004 to 2009[J]. Hepatology, 2015, 62(6): 1723-1730. DOI: 10.1002/hep.28123. [8] RINELLA M, CHARLTON M. The globalization of nonalcoholic fatty liver disease: Prevalence and impact on world health[J]. Hepatology, 2016, 64(1): 19-22. DOI: 10.1002/hep.28524. [9] ERTLE J, DECHÊNE A, SOWA JP, et al. Non-alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis[J]. Int J Cancer, 2011, 128(10): 2436-2443. DOI: 10.1002/ijc.25797. [10] DYSON J, JAQUES B, CHATTOPADYHAY D, et al. Hepatocellular cancer: The impact of obesity, type 2 diabetes and a multidisciplinary team[J]. J Hepatol, 2014, 60(1): 110-117. DOI: 10.1016/j.jhep.2013.08.011. [11] WALLACE MC, PREEN D, JEFFREY GP, et al. The evolving epidemiology of hepatocellular carcinoma: A global perspective[J]. Expert Rev Gastroenterol Hepatol, 2015, 9(6): 765-779. DOI: 10.1586/17474124.2015.1028363. [12] WANG FS, FAN JG, ZHANG Z, et al. The global burden of liver disease: The major impact of China[J]. Hepatology, 2014, 60(6): 2099-2108. DOI: 10.1002/hep.27406. [13] ZHOU M, WANG H, ZHU J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: A systematic subnational analysis for the Global Burden of Disease Study 2013[J]. Lancet, 2016, 387(10015): 251-272. DOI: 10.1016/S0140-6736(15)00551-6. [14] CHO EJ, KWACK MS, JANG ES, et al. Relative etiological role of prior hepatitis B virus infection and nonalcoholic fatty liver disease in the development of non-B non-C hepatocellular carcinoma in a hepatitis B-endemic area[J]. Digestion, 2011, 84(Suppl 1): 17-22. DOI: 10.1159/000333210. [15] Bureau of Medical AdministrationNational Health Commission of the People's Republic of China. Guidelines for diagnosis and treatment of primary liver cancer in China (2019 edition)[J]. J Clin Hepatol, 2020, 36(2): 277-292. DOI: 10.3969/j.issn.1001-5256.2020.02.007.中华人民共和国国家卫生健康委员会医政医管局. 原发性肝癌诊疗规范(2019年版)[J]. 临床肝胆病杂志, 2020, 36(2): 277-292. DOI: 10.3969/j.issn.1001-5256.2020.02.007. [16] MYERS S, NEYROUD-CASPAR I, SPAHR L, et al. NAFLD and MAFLD as emerging causes of HCC: A populational study[J]. JHEP Rep, 2021, 3(2): 100231. DOI: 10.1016/j.jhepr.2021.100231. [17] DUAN XY, QIAO L, FAN JG. Clinical features of nonalcoholic fatty liver disease-associated hepatocellular carcinoma[J]. Hepatobiliary Pancreat Dis Int, 2012, 11(1): 18-27. DOI: 10.1016/s1499-3872(11)60120-3. [18] STARLEY BQ, CALCAGNO CJ, HARRISON SA. Nonalcoholic fatty liver disease and hepatocellular carcinoma: A weighty connection[J]. Hepatology, 2010, 51(5): 1820-1832. DOI: 10.1002/hep.23594. [19] TOKUSHIGE K, HYOGO H, NAKAJIMA T, et al. Hepatocellular carcinoma in Japanese patients with nonalcoholic fatty liver disease and alcoholic liver disease: Multicenter survey[J]. J Gastroenterol, 2016, 51(6): 586-596. DOI: 10.1007/s00535-015-1129-1. [20] KOBAYASHI S, MATSUI O, GABATA T, et al. Hemodynamics of small sclerosing hepatocellular carcinoma without fibrous capsule: Evaluation with single-level dynamic CT during hepatic arteriography[J]. Abdom Imaging, 2008, 33(4): 425-427. DOI: 10.1007/s00261-007-9288-z. [21] KANG BK, YU ES, LEE SS, et al. Hepatic fat quantification: A prospective comparison of magnetic resonance spectroscopy and analysis methods for chemical-shift gradient echo magnetic resonance imaging with histologic assessment as the reference standard[J]. Invest Radiol, 2012, 47(6): 368-375. DOI: 10.1097/RLI.0b013e31824baff3. [22] ZHANG ZJ, ZHENG ZJ, SHI R, et al. Metformin for liver cancer prevention in patients with type 2 diabetes: A systematic review and meta-analysis[J]. J Clin Endocrinol Metab, 2012, 97(7): 2347-53. DOI: 10.1210/jc.2012-1267. [23] TRAN KT, MCMENAMIN úC, COLEMAN HG, et al. Statin use and risk of liver cancer: Evidence from two population-based studies[J]. Int J Cancer, 2020, 146(5): 1250-1260. DOI: 10.1002/ijc.32426. [24] KOGISO T, TOKUSHIGE K. The current view of nonalcoholic fatty liver disease-related hepatocellular carcinoma[J]. Cancers (Basel), 2021, 13(3): 516. DOI: 10.3390/cancers13030516. [25] KUDO M, MATSUI O, IZUMI N, et al. JSH consensus-based clinical practice guidelines for the management of hepatocellular carcinoma: 2014 Update by the Liver Cancer Study Group of Japan[J]. Liver Cancer, 2014, 3(3-4): 458-468. DOI: 10.1159/000343875. [26] BRUIX J, SHERMAN M. Management of hepatocellular carcinoma: An update[J]. Hepatology, 2011, 53(3): 1020-1022. DOI: 10.1002/hep.24199. [27] KOKUDO N, TAKEMURA N, HASEGAWA K, et al. Clinical practice guidelines for hepatocellular carcinoma: The Japan Society of Hepatology 2017 (4th JSH-HCC guidelines) 2019 update[J]. Hepatol Res, 2019, 49(10): 1109-1113. DOI: 10.1111/hepr.13411. [28] MALLIK R, CHOWDHURY TA. Metformin in cancer[J]. Diabetes Res Clin Pract, 2018, 143: 409-419. DOI: 10.1016/j.diabres.2018.05.023. [29] COYLE C, CAFFERTY FH, VALE C, et al. Metformin as an adjuvant treatment for cancer: A systematic review and meta-analysis[J]. Ann Oncol, 2016, 27(12): 2184-2195. DOI: 10.1093/annonc/mdw410. [30] SHI T, KOBARA H, OURA K, et al. Mechanisms underlying hepatocellular carcinoma progression in patients with type 2 diabetes[J]. J Hepatocell Carcinoma, 2021, 8: 45-55. DOI: 10.2147/JHC.S274933. [31] ADAM R, KARAM V, CAILLIEZ V, et al. 2018 Annual Report of the European Liver Transplant Registry (ELTR) - 50-year evolution of liver transplantation[J]. Transpl Int, 2018, 31(12): 1293-1317. DOI: 10.1111/tri.13358. [32] COTTER TG, CHARLTON M. Nonalcoholic steatohepatitis after liver transplantation[J]. Liver Transpl, 2020, 26(1): 141-159. DOI: 10.1002/lt.25657. [33] WONG RJ, CHEUNG R, AHMED A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U. S[J]. Hepatology, 2014, 59(6): 2188-2195. DOI: 10.1002/hep.26986. [34] CHARLTON MR, BURNS JM, PEDERSEN RA, et al. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States[J]. Gastroenterology, 2011, 141(4): 1249-1253. DOI: 10.1053/j.gastro.2011.06.061. [35] YOUNOSSI Z, ANSTEE QM, MARIETTI M, et al. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention[J]. Nat Rev Gastroenterol Hepatol, 2018, 15(1): 11-20. DOI: 10.1038/nrgastro.2017.109. [36] HONAP S, OBEN JA. Fat and hidden liver cancer[J]. Clin Liver Dis (Hoboken), 2021, 17(2): 49-52. DOI: 10.1002/cld.1011. [37] RAMAI D, TAI W, RIVERA M, et al. Natural progression of non-alcoholic steatohepatitis to hepatocellular carcinoma[J]. Biomedicines, 2021, 9(2): 184. DOI: 10.3390/biomedicines9020184. [38] European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma[J]. J Hepatol, 2018, 69(1): 182-236. DOI: 10.1016/j.jhep.2018.03.019. [39] MARRERO JA, KULIK LM, SIRLIN CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases[J]. Hepatology, 2018, 68(2): 723-750. DOI: 10.1002/hep.29913. -



 PDF下载 ( 2794 KB)
PDF下载 ( 2794 KB)

 下载:
下载: