非酒精性脂肪性肝炎新药临床试验的难度与挑战
DOI: 10.3969/j.issn.1001-5256.2021.08.044
利益冲突声明:所有作者均声明不存在利益冲突。
作者贡献声明:黄樱硕负责查询资料及分析,撰写论文;董瑞华参与修改论文;尤红拟定写作思路,指导撰写文章并最后定稿。
Difficulties and challenges in the clinical trial of new drugs for nonalcoholic steatohepatitis
-
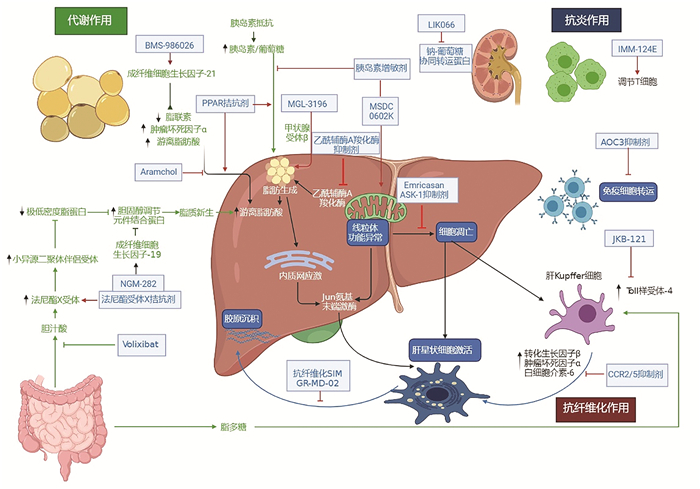
摘要: 近年来非酒精性脂肪性肝炎(NASH)的发病率不断增长,且临床上缺乏有效的治疗药物。从NASH的异质性(如体质量、性别、年龄和代谢因素)、混杂因素的影响、量化指标的诊断一致性等方面分析了NASH新药临床试验开发的难度,提出可以通过分层分析、减弱混杂因素影响、提高诊断一致性等方式提高NASH新药临床试验的质量。包括生活方式改善在内的联合治疗可能是有效的NASH治疗策略,以改善NASH和抗纤维化及长期代谢获益为目标的治疗是未来药物研发的研究方向。Abstract: The incidence rate of nonalcoholic steatohepatitis (NASH) keeps increasing in recent years, and there is still a lack of effective therapeutic drugs in clinical practice. This article analyzes the difficulties in the clinical trial of new drugs for NASH from the aspects of the heterogeneity of NASH (body weight, sex, age, and metabolic factors), the influence of confounding factors, and the diagnostic consistency of quantitative indicators, and it is pointed out that conducting a stratified analysis, reducing the influence of confounding factors, and improving diagnostic consistency can help to improve the quality of the clinical trials of new drugs for NASH. Combination therapy including lifestyle improvement may be an effective treatment strategy for NASH, and therapies aiming at improving NASH, exerting an anti-fibrosis effect, and obtaining long-term metabolic benefits are the direction for drug research and development in the future.
-
Key words:
- Non-Alcoholic Steatohepatitis /
- Drugs, Investigational /
- Therapeutics
-
表 1 国内外NASH新药研发情况
药物名称 研发公司 作用机制 研究及分期 研发情况 Obeticholic acid(奥贝胆酸) Intercept FXR激动剂 REGENERATE[9],3期 美国食品药品监督管理局拒绝上市(中期组织学终点数据带来的获益仍具有不确定性,建议提供后续有效性和安全性数据,以评估是否达到获益风险比) Selonsertib/GS-0976 Gilead ACC抑制剂 STELLAR-3[10-11]和STELLAR-4[12],3期 以纤维化伴或不伴NASH恶化作为关键终点。STELLAR-3评估Selonsertib对NASH引起的桥接纤维化(F3)患者的安全性和有效性,未能到达48周的预期临床终点。STELLAR-4评估Selonsertib对NASH引起的代偿性肝硬化(F4)患者的安全性和有效性,亦未达到主要终点 Elafibranor Genfit PPARα/δ双重激动剂 RESOLVE-IT[13],3期 未能达到NASH病理改善伴或不伴纤维化恶化的关键终点 Cenicriviroc Allergan CCR2/CCR5受体抑制剂 AURORA[14-15],3期 以纤维化改善伴或不伴NASH恶化作为关键终点,评估CCR相比安慰剂治疗NASH患者的有效性和安全性。目前研究正在进行中 MGL-3196 Magrigal TRβ激动剂 MAESTRO-NAFLD[16-17],3期 评估Resmetirom相比安慰剂治疗NAFLD/NASH患者的安全性和生化标志物。研究正在进行中 LMB763 诺华 FXR激动剂 ELIVATE[18],2期 研究终点为提高胰岛素敏感性,减少肝脂肪变、炎症和纤维化。研究正在进行中 ASC40 歌礼 & 3-V Biosciences 脂肪酸合成酶抑制剂 FASCINATE-1[19],2期 研究终点为降低肝脏脂肪含量。研究正在进行中 HTD1801[20] 君圣泰 多功能小分子药物,机制未公布 2期 改善肝组织学特征,降低肝脏胆固醇和甘油三酯。研究正在进行中 ZSP1601[21] 广东众生药业 小分子化学药物,机制未公布 Ⅰb/Ⅱa期 改善NASH纤维化。研究正在进行中 注:FXR,法尼酯X受体; ACC,乙酰辅酶A羧化酶;PPAR,过氧化物酶体增殖剂激活受体;CCR,Cenicriviroc;TR, 甲状腺受体。 -
[1] YOUNOSSI ZM, KOENIG AB, ABDELATIF D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes[J]. Hepatology, 2016, 64(1): 73-84. DOI: 10.1002/hep.28431. [2] CHALASANI N, YOUNOSSI Z, LAVINE JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases[J]. Hepatology, 2018, 67(1): 328-357. DOI: 10.1002/hep.29367. [3] European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease[J]. J Hepatol, 2016, 64(6): 1388-1402. DOI: 10.1016/j.jhep.2015.11.004. [4] RINELLA ME, LOOMBA R, CALDWELL SH, et al. Controversies in the diagnosis and management of NAFLD and NASH[J]. Gastroenterol Hepatol (N Y), 2014, 10(4): 219-227. [5] SANYAL AJ, FRIEDMAN SL, McCULLOUGH AJ, et al. Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: Findings and recommendations from an American Association for the Study of Liver Diseases-U.S. Food and Drug Administration Joint Workshop[J]. Hepatology, 2015, 61(4): 1392-1405. DOI: 10.1002/hep.27678. [6] YOUNOSSI ZM, LOOMBA R, RINELLA ME, et al. Current and future therapeutic regimens for nonalcoholic fatty liver disease and nonalcoholic steatohepatitis[J]. Hepatology, 2018, 68(1): 361-371. DOI: 10.1002/hep.29724. [7] KONERMAN MA, JONES JC, HARRISON SA. Pharmacotherapy for NASH: Current and emerging[J]. J Hepatol, 2018, 68(2): 362-375. DOI: 10.1016/j.jhep.2017.10.015. [8] SIDDIQUI MS, IDOWU MO, PARMAR D, et al. A phase 2 double blinded, randomized controlled trial of saroglitazar in patients with nonalcoholic steatohepatitis[J]. Clin Gastroenterol Hepatol, 2020. DOI: 10.1016/j.cgh.2020.10.051.[Onlineaheadofprint] [9] YOUNOSSI ZM, RATZIU V, LOOMBA R, et al. Obeticholic acid for the treatment of non-alcoholic steatohepatitis: Interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial[J]. Lancet, 2019, 394(10215): 2184-2196. DOI: 10.1016/S0140-6736(19)33041-7. [10] HARRISON SA, WONG VW, OKANOUE T, et al. Selonsertib for patients with bridging fibrosis or compensated cirrhosis due to NASH: Results from randomized phase Ⅲ STELLAR trials[J]. J Hepatol, 2020, 73(1): 26-39. DOI: 10.1016/j.jhep.2020.02.027. [11] Gilead Science. Safety and efficacy of selonsertib in adults with nonalcoholic steatohepatitis (NASH) and bridging (F3) fibrosis (STELLAR-3)[EB/OL]. [2021-01-21]. https://clinicaltrials.gov/ct2/show/NCT03053050. [12] Gilead Science. Safety and efficacy of selonsertib in adults with compensated cirrhosis due to nonalcoholic steatohepatitis (NASH) (STELLAR-4)[EB/OL]. [2021-01-21]. https://clinicaltrials.gov/ct2/show/NCT03053063. [13] Genfit. Phase 3 study to evaluate the efficacy and safety of elafibranor versus placebo in patients with nonalcoholic steatohepatitis (NASH) (RESOLVE-IT)[EB/OL]. [2021-01-21]. https://clinicaltrials.gov/ct2/show/NCT02704403. [14] ANSTEE QM, NEUSCHWANDER-TETRI BA, WONG VW, et al. Cenicriviroc for the treatment of liver fibrosis in adults with nonalcoholic steatohepatitis: AURORA Phase 3 study design[J]. Contemp Clin Trials, 2020, 89: 105922. DOI: 10.1016/j.cct.2019.105922. [15] Tobira Therapeutics Inc. AURORA: Phase 3 study for the efficacy and safety of CVC for the treatment of liver fibrosis in adults with NASH[EB/OL]. [2021-01-21]. https://clinicaltrials.gov/ct2/show/NCT03028740. [16] HARRISON SA, BASHIR MR, GUY CD, et al. Resmetirom (MGL-3196) for the treatment of non-alcoholic steatohepatitis: A multicentre, randomised, double-blind, placebo-controlled, phase 2 trial[J]. Lancet, 2019, 394(10213): 2012-2024. DOI: 10.1016/S0140-6736(19)32517-6. [17] Madrigal Pharmaceuticals Inc. Phase 2 study of MGL-3196 in patients with non-alcoholic steatohepatitis (NASH)[EB/OL]. [2021-01-21]. https://clinicaltrials.gov/ct2/show/NCT02912260. [18] CHIANELLI D, RUCKER PV, ROLAND J, et al. Nidufexor (LMB763), a novel FXR modulator for the treatment of nonalcoholic steatohepatitis[J]. J Med Chem, 2020, 63(8): 3868-3880. DOI: 10.1021/acs.jmedchem.9b01621. [19] Sagimet Biosciences Inc. Study of TVB 2640 in subjects with non-alcoholic steatohepatitis (NASH)[EB/OL]. [2021-01-21]. https://clinicaltrials.gov/ct2/show/NCT03938246. [20] A study of HTD1801 in adults with nonalcoholic steatohepatitis (NASH) and type 2 diabetes mellitus (T2DM)[EB/OL]. [2021-01-21]. https://clinicaltrials.gov/ct2/show/NCT03656744. [21] Guangdong Zhongsheng Pharmaceutical Co. Ltd. Tolerability, pharmacokinetics, and early pharmacodynamics of ZSP1601 tablets in NASH patients: A multicenter, randomized, double-blind, dose-escalation, and placebo-controlled phase Ib/Ⅱa clinical trial[EB/OL]. [2021-01-21]. http://www.chinadrugtrials.org.cn.广东众生药业股份有限公司. 评价ZSP1601片在NASH患者多中心、随机、双盲、剂量递增、安慰剂对照的耐受性、药代动力学和早期药效学Ib/Ⅱa期临床试验[EB/OL]. [2021-01-21]. http://www.chinadrugtrials.org.cn. [22] YOUNES R, BUGIANESI E. NASH in lean individuals[J]. Semin Liver Dis, 2019, 39(1): 86-95. DOI: 10.1055/s-0038-1677517. [23] SHI Y, WANG Q, SUN Y, et al. The prevalence of lean/nonobese nonalcoholic fatty liver disease: A systematic review and meta-analysis[J]. J Clin Gastroenterol, 2020, 54(4): 378-387. DOI: 10.1097/MCG.0000000000001270. [24] HAGSTRÖM H, NASR P, EKSTEDT M, et al. Risk for development of severe liver disease in lean patients with nonalcoholic fatty liver disease: A long-term follow-up study[J]. Hepatol Commun, 2018, 2(1): 48-57. DOI: 10.1002/hep4.1124. [25] WANG Q, YOU H, OU X, et al. Non-obese histologically confirmed NASH patients with abnormal liver biochemistry have more advanced fibrosis[J]. Hepatol Int, 2019, 13(6): 766-776. DOI: 10.1007/s12072-019-09982-z. [26] TOBARI M, HASHIMOTO E, TANIAI M, et al. Characteristics of non-alcoholic steatohepatitis among lean patients in Japan: Not uncommon and not always benign[J]. J Gastroenterol Hepatol, 2019, 34(8): 1404-1410. DOI: 10.1111/jgh.14585. [27] CURCIC IB, BERKOVIC MC, KUNA L, et al. Obesity paradox in chronic liver diseases: Product of bias or a real thing?[J]. J Clin Transl Hepatol, 2019, 7(3): 275-279. DOI: 10.14218/JCTH.2019.00029. [28] LONARDO A, NASCIMBENI F, BALLESTRI S, et al. Sex differences in nonalcoholic fatty liver disease: State of the art and identification of research gaps[J]. Hepatology, 2019, 70(4): 1457-1469. DOI: 10.1002/hep.30626. [29] SHEEDFAR F, DI BIASE S, KOONEN D, et al. Liver diseases and aging: Friends or foes?[J]. Aging Cell, 2013, 12(6): 950-954. DOI: 10.1111/acel.12128. [30] YOUNOSSI ZM, GOLABI P, de AVILA L, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis[J]. J Hepatol, 2019, 71(4): 793-801. DOI: 10.1016/j.jhep.2019.06.021. [31] BAZICK J, DONITHAN M, NEUSCHWANDER-TETRI BA, et al. Clinical model for NASH and advanced fibrosis in adult patients with diabetes and NAFLD: Guidelines for referral in NAFLD[J]. Diabetes Care, 2015, 38(7): 1347-1355. DOI: 10.2337/dc14-1239. [32] SUNG KC, WILD SH, BYRNE CD. Resolution of fatty liver and risk of incident diabetes[J]. J Clin Endocrinol Metab, 2013, 98(9): 3637-3643. DOI: 10.1210/jc.2013-1519. [33] LONARDO A, NASCIMBENI F, MANTOVANI A, et al. Hypertension, diabetes, atherosclerosis and NASH: Cause or consequence?[J]. J Hepatol, 2018, 68(2): 335-352. DOI: 10.1016/j.jhep.2017.09.021. [34] AMPUERO J, ALLER R, GALLEGO-DURáN R, et al. The effects of metabolic status on non-alcoholic fatty liver disease-related outcomes, beyond the presence of obesity[J]. Aliment Pharmacol Ther, 2018, 48(11-12): 1260-1270. DOI: 10.1111/apt.15015. [35] VILAR-GOMEZ E, MARTINEZ-PEREZ Y, CALZADILLA-BERTOT L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis[J]. Gastroenterology, 2015, 149(2): 367-378. DOI: 10.1053/j.gastro.2015.04.005. [36] ROMERO-GÓMEZ M, ZELBER-SAGI S, TRENELL M. Treatment of NAFLD with diet, physical activity and exercise[J]. J Hepatol, 2017, 67(4): 829-846. DOI: 10.1016/j.jhep.2017.05.016. [37] DAVISON BA, HARRISON SA, COTTER G, et al. Suboptimal reliability of liver biopsy evaluation has implications for randomized clinical trials[J]. J Hepatol, 2020, 73(6): 1322-1332. DOI: 10.1016/j.jhep.2020.06.025. [38] HOOKER JC, HAMILTON G, PARK CC, et al. Inter-reader agreement of magnetic resonance imaging proton density fat fraction and its longitudinal change in a clinical trial of adults with nonalcoholic steatohepatitis[J]. Abdom Radiol (NY), 2019, 44(2): 482-492. DOI: 10.1007/s00261-018-1745-3. [39] HONG CW, MARSH A, WOLFSON T, et al. Reader agreement and accuracy of ultrasound features for hepatic steatosis[J]. Abdom Radiol (NY), 2019, 44(1): 54-64. DOI: 10.1007/s00261-018-1683-0. [40] RATZIU V, FRIEDMAN SL. Why do so many NASH trials fail?[J]. Gastroenterology, 2020. DOI: 10.1053/j.gastro.2020.05.046.[Onlineaheadofprint] -



 PDF下载 ( 2745 KB)
PDF下载 ( 2745 KB)

 下载:
下载:


