肝脏三维可视化重建技术在儿童复杂肝母细胞瘤肝切除术中的应用价值
DOI: 10.3969/j.issn.1001-5256.2021.09.025
Application of liver three-dimensional visualized reconstruction technique in hepatectomy for children with complicated hepatoblastoma
-
摘要:
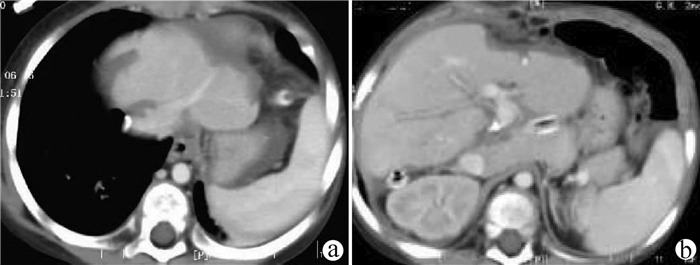
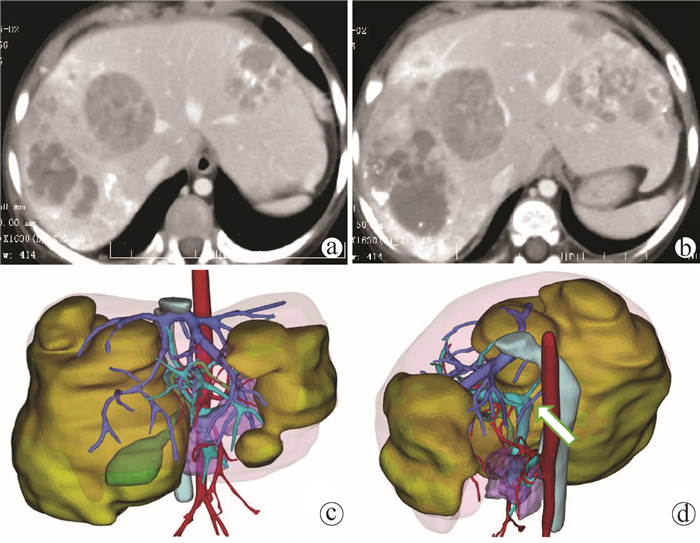
目的 探讨肝脏三维可视化重建技术在儿童复杂肝母细胞瘤肝切除术中的应用价值。 方法 回顾分析2018年1月—2020年10月于火箭军特色医学中心实施了以根治性切除为目的的肝肿瘤切除术的30例肝母细胞瘤患儿的临床资料,根据术前是否行肝脏三维重建(IQQA-Liver系统)将所有患儿分为三维重建组(n=15)和对照组(n=15),比较2组患儿围手术期临床参数以及短期预后和随访情况。符合正态分布的计量资料2组间比较采用独立样本t检验,不符合正态分布的计量资料2组间比较采用Mann-whitney U检验。计数资料2组间比较采用Fisher确切概率法。 结果 三维重建组较对照组平均年龄更大[(55.7±10.2)月vs (28.2± 2.7)月]、POSTTEXT Ⅲ/Ⅵ期(12例vs 5例)和肝静脉或下腔静脉受累者(11例vs 3例)更多,差异均有统计学意义(P值均<0.05)。所有患儿均顺利完成手术,2组在出血量、手术时间、肝门阻断次数/时间、行肝段及部分肝切除例数方面,差异均无统计学意义(P值均>0.05)。术后中位随访时间9.5个月,三维重建组2例复发,分别于术后10个月和12个月确诊,目前继续化疗中;对照组4例复发,高于三维重建组(P=0.651),其中2例在术后7个月复发接受肝移植存活至今,另有2例复发后短期内死亡。 结论 三维可视化重建技术有助于更安全精准实施复杂儿童肝母细胞瘤肝切除术,尤其是可以使部分POSTTEXT Ⅲ/Ⅵ期患者安全实施扩大肝切除,从而避免行肝移植。 Abstract:Objective To investigate the application of liver three-dimensional (3D) visualized reconstruction technique in hepatectomy for children with complicated hepatoblastoma. Methods A retrospective analysis was performed for the clinical data of 30 children with hepatoblastoma who underwent hepatectomy for radical resection in PLA Rocket Force Characteristic Medical Center from January 2018 to October 2020, and according to whether liver 3D visualization with IQQA-Liver system was performed before surgery, the children were divided into 3D reconstruction group with 15 children and control group with 15 children. The two groups were compared in terms of perioperative parameters, short-term prognosis, and follow-up conditions. The independent samples t-test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups; the Fisher's exact test was used for comparison of categorical data between two groups. Results Compared with the control group, the 3D reconstruction group had a significantly higher mean age (55.7±10.2 years vs 28.2±2.7 years, P < 0.05) and a significantly higher number of patients with POSTTEXT stage III/VI hepatoblastoma (12 vs 5, P < 0.05) or involvement of the hepatic vein or the inferior vena cava (11 vs 3, P < 0.05). All children completed the surgery successfully, and there were no significant differences between the two groups in blood loss, time of operation, number of times and duration of hepatic portal occlusion, and number of children receiving segmental hepatectomy or partial hepatectomy (all P > 0.05). The median follow-up after surgery was 9.5 months. In the 3D reconstruction group, 2 children experienced recurrence and were diagnosed at 10 and 12 months, respectively, after surgery, and they were treated with chemotherapy at the moment; in the control group, 4 children experienced recurrence, which was higher than that in the 3D reconstruction group (P=0.651), and among these 4 children, 2 had recurrence at 7 months after surgery, received liver transplantation, and survived up to now, and the other 2 children died shortly after recurrence. Conclusion 3D visualized reconstruction technique helps to perform hepatectomy for children with complicated hepatoblastoma more safely and accurately, especially extended hepatectomy for patients with stage POST TEXT III/IV hepatoblastoma, thereby avoiding liver transplantation. -
Key words:
- Hepatoblastoma /
- Hepatectomy /
- Imaging, Three-Dimensional /
- Child
-
表 1 2组患儿术前一般资料比较
项目 三维重建组(n=15) 对照组(n=15) 统计值 P值 男/女(例) 10/5 8/7 0.710 年龄(月) 55.7±10.2 28.2±2.7 t=2.603 0.019 化疗(次) 5.0±1.0 5.0±0.5 t=0.836 0.410 ALT (U/L) 22.0±4.4 20.9±2.6 t=0.214 0.832 AFP(ng/ml) 6240(686~16 805) 2800(947~18 465) Z=-0.041 0.967 血红蛋白(g/L) 99.8±3.8 95.8±4.4 t=0.692 0.495 血小板计数(×109/L) 194±23 225±35 t=-0.709 0.484 POSTTEXT分期(例) 0.025 Ⅰ期 0 0 Ⅱ期 3 10 Ⅲ期 8 5 Ⅳ期 4 0 多发病灶(例) 11 11 1.000 肝静脉或下腔静脉受累(例) 11 3 0.009 门静脉受累(例) 8 4 0.264 尾状叶受累(例) 3 2 1.000 肿瘤破裂/出血(例) 5 1 0.169 肿瘤大小(cm) 7.0±0.6 6.0±1.1 t=0.852 0.401 远处转移(例) 3 3 1.000 表 2 2组患儿手术方式及术中指标比较
项目 三维重建组(n=15) 对照组(n=15) t值 P值 出血量(ml) 520±123 562±195 -0.182 0.857 手术时间(min) 301±21 257±24 1.38 3 0.178 肝门阻断次数(次) 3.0±0.2 2.0±0.1 1.90 1 0.068 肝门阻断时间(min) 38.0±3.2 30.0±2.7 2.00 6 0.055 手术方式(例) 肝S4段切除术 1 0 肝S2~3段切除术 0 1 肝S4段切除联合肝S2~3段部分切除术 0 1 肝S2~4段切除术 1 3 肝S1, 2~4段切除术 1 0 肝S1, 2~4,5, 8段切除术 1 0 肝S1, 2~4,5, 8段切除术联合门静脉切开取栓术 0 1 肝S1段切除、S5, 8段局部切除、S6, 7段局部切除术 0 1 肝S5~8段切除术 1 1 肝S5~8段切除,S2~3段部分切除术 1 0 肝S1, 5~8切除术 0 1 肝S4段部分切除, 5~8段切除术 1 0 肝S4, 5~8段切除术 2 3 肝S4, 5~8段切除术联合门脉癌栓取出术 1 0 肝S4, 5, 8段切除术 1 2 肝S5, 7, 8段切除 1 0 肝S1切除术 1 0 肝S5段切除 0 1 肝S1, 4段切除,右肝胆管切开取栓,下腔静脉后段切除血管置换术 1 0 肝S1/S4切除,腹腔多发转移灶切除术 1 0 表 3 2组患儿术后情况比较
项目 三维重建组(n=15) 对照组(n=15) 统计值 P值 术后1 d ALT(U/L) 132.8(99.7~312.4) 225.8(153.6~290.2) Z=-1.224 0.221 TBil (μmol/L) 40.7(26.8~61.2) 25.9(20.0~44.4) Z=-1.472 0.141 术后3 d ALT(U/L) 92.3(65.2~156.2) 104.0(76.3~167.0) Z=-0.726 0.468 TBil (μmol/L) 13.5(11.8~25.7) 16.2(9.7~35.5) Z=-0.104 0.917 住院时间(d) 9.0±0.6 9.0±0.6 t=0.645 0.524 术后输血量(ml) 210±60 200±47 t=0.130 0.897 术后并发症(人次) 18 20 胸腔积液 11 8 0.450 腹腔积液 3 5 0.682 肺部感染 2 1 1 胆漏 1 2 1 切口感染 0 1 1 乳糜漏 0 1 1 轻中度肝损伤 0 1 1 泌尿系感染 0 1 1 门静脉血栓 1 0 1 表 4 2组患儿肝母细胞瘤病理分型
病理类型 三维重建组(n=15) 对照组(n=15) 上皮型(例) 12 13 胎儿型 11 7 胚胎型 1 1 粗小梁型 0 1 上皮混合型 0 4 上皮间叶混合型(例) 3 2 -
[1] YANG T, WHITLOCK RS, VASUDEVAN SA. Surgical management of hepatoblastoma and recent advances[J]. Cancers (Basel), 2019, 11(12): 1944. DOI: 10.3390/cancers11121944. [2] HAFBERG E, BORINSTEIN SC, ALEXOPOULOS SP. Contemporary management of hepatoblastoma[J]. Curr Opin Organ Transplant, 2019, 24(2): 113-117. DOI: 10.1097/MOT.0000000000000618. [3] WANG XS, YANG W, HUANG C, et al. Clinical features and outcome evaluation for children with hepatoblastoma[J]. J Capit Med Univ, 2019, 40(2): 169-173. DOI: 10.3969/j.issn.1006-7795.2019.02.003.王希思, 杨维, 黄程, 等. 儿童肝母细胞瘤的临床特征和治疗效果评价[J]. 首都医科大学学报, 2019, 40(2): 169-173. DOI: 10.3969/j.issn.1006-7795.2019.02.003. [4] LAKE CM, TIAO GM, BONDOC AJ. Surgical management of locally-advanced and metastatic hepatoblastoma[J]. Semin Pediatr Surg, 2019, 28(6): 150856. DOI: 10.1016/j.sempedsurg.2019.150856. [5] Compilation and Examination Expert Group for Guidelines for the diagnosis and treatment of hepatoblastoma (2019). Guidelines for the diagnosis and treatment of hepatoblastoma (2019)[J]. J Clin Hepatol, 2019, 35(11): 2431-2434. DOI: 10.3969/j.issn.1001-5256.2019.11.008.儿童肝母细胞瘤诊疗规范(2019年版)编写审定专家组. 儿童肝母细胞瘤诊疗规范(2019年版)[J]. 临床肝胆病杂志, 2019, 35(11): 2431-2434. DOI: 10.3969/j.issn.1001-5256.2019.11.008. [6] EL-GENDI A, FADEL S, EL-SHAFEI M, et al. Avoiding liver transplantation in post-treatment extent of disease III and IV hepatoblastoma[J]. Pediatr Int, 2018, 60(9): 862-868. DOI: 10.1111/ped.13634. [7] ZHU W, HE SS, ZENG SL, et al. Three-dimensional visual assessment and virtual reality study of centrally located hepatocellular carcinoma on the axis of blood vessels[J]. Chin J Surg, 2019, 57(5): 358-365. DOI: 10.3760/cma.j.issn.0529-5815.2019.05.008.祝文, 何松盛, 曾思略, 等. 以血管为轴心的中央型肝癌三维可视化评估及虚拟现实的研究[J]. 中华外科杂志, 2019, 57(5): 358-365. DOI: 10.3760/cma.j.issn.0529-5815.2019.05.008. [8] Chinese Society of Digital Medicine, Liver Cancer Committee of Chinese Medical Doctor Association, Clinical Precision Medicine Committee of Chinese Medical Doctor Association, et al. Specification for technical operation and clinical application of three-dimensional visualization technology for primary liver cancer (2020 edition)[J]. Chin J Dig Surg, 2020, 19(9): 897-918. DOI: 10.3760/cma.j.cn115610-20200720-00499.中华医学会数字医学分会, 中国医师协会肝癌专业委员会, 中国医师协会精准医学专业委员会, 等. 原发性肝癌三维可视化技术操作及诊疗规范(2020版)[J]. 中华消化外科杂志, 2020, 19(9): 897-918. DOI: 10.3760/cma.j.cn115610-20200720-00499. [9] FANG C, AN J, BRUNO A, et al. Consensus recommendations of three-dimensional visualization for diagnosis and management of liver diseases[J]. Hepatol Int, 2020, 14(4): 437-453. DOI: 10.1007/s12072-020-10052-y. [10] ZHANG G, ZHOU XJ, ZHU CZ, et al. Usefulness of three-dimensional(3D) simulation software in hepatectomy for pediatric hepatoblastoma[J]. Surg Oncol, 2016, 25(3): 236-243. DOI: 10.1016/j.suronc.2016.05.023. [11] SU L, DONG Q, ZHANG H, et al. Clinical application of a three-dimensional imaging technique in infants and young children with complex liver tumors[J]. Pediatr Surg Int, 2016, 32(4): 387-395. DOI: 10.1007/s00383-016-3864-7. [12] SU L, DONG Q, ZHANG H, et al. 3D Application of 3D visualization technology in precise hepatectomy for complex liver tumors in infants[J/CD]. Chin J Hepat Surg(Electronic Edition), 2015, 4(5): 274-278. DOI: 10.3877/cma.j.issn.2095-3232.2015.05.005.苏琳, 董蒨, 张虹, 等. 3D可视化技术在婴幼儿复杂肝肿瘤精准肝切除中的应用[J/CD]. 中华肝脏外科手术学电子杂志, 2015, 4(5): 274-278. DOI: 10.3877/cma.j.issn.2095-3232.2015.05.005. [13] ZHAO J, ZHOU XJ, ZHU CZ, et al. 3D simulation assisted resection of giant hepatic mesenchymal hamartoma in children[J]. Comput Assist Surg (Abingdon), 2017, 22(1): 54-59. DOI: 10.1080/24699322.2017.1358401. [14] FUCHS J, CAVDAR S, BLUMENSTOCK G, et al. POST-TEXT III and IV hepatoblastoma: Extended hepatic resection avoids liver transplantation in selected cases[J]. Ann Surg, 2017, 266(2): 318-323. DOI: 10.1097/SLA.0000000000001936. [15] ARONSON DC, WEEDA VB, MAIBACH R, et al. Microscopically positive resection margin after hepatoblastoma resection: What is the impact on prognosis? A Childhood Liver Tumours Strategy Group (SIOPEL) report[J]. Eur J Cancer, 2019, 106: 126-132. DOI: 10.1016/j.ejca.2018.10.013. [16] SONG D, SUN D, JIANG DS. Comparative study of three-dimensional visualization technology and two-dimensional imaging technology in liver resection of liver cancer patients[J]. J Clin Exp Med, 2020, 19(6): 656-660. DOI: 10.3969/j.issn.1671-4695.2020.06.026.宋铎, 孙铎, 姜德帅. 三维可视化技术与二维影像技术在肝癌患者肝切除术中的疗效比较研究[J]. 临床和实验医学杂志, 2020, 19(6): 656-660. DOI: 10.3969/j.issn.1671-4695.2020.06.026. -



 PDF下载 ( 3973 KB)
PDF下载 ( 3973 KB)

 下载:
下载: