慢加急性肝衰竭合并细菌感染患者的临床特征及预后影响因素分析
DOI: 10.3969/j.issn.1001-5256.2021.09.028
Clinical features of patients with acute-on-chronic liver failure and bacterial infection and influencing factors for prognosis
-
摘要:
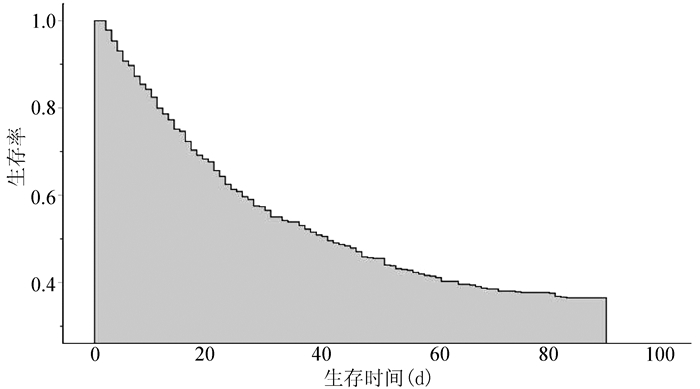
目的 研究慢加急性肝衰竭(ACLF)合并细菌感染患者的临床感染特点及90 d生存率的相关影响因素。 方法 选取2014年1月—2015年12月解放军总医院第五医学中心收治的ACLF患者,收集和分析患者的相关临床资料:感染时间及部位、微生物培养情况、生化及炎性指标、合并感染后28 d及90 d预后情况等。计量资料两组间比较采用t检验或Mann-Whitney U检验;计数资料两组间比较采用χ2检验。应用寿命表法绘制生存曲线。将单因素分析中对预后有影响的指标进一步行多因素logistic回归分析。 结果 共收治ACLF患者1074例,其中609例合并细菌感染,感染发生率为56.7%。有16例患者在90 d内行肝移植手术,其余593例均完成了相关数据统计。各部位感染占总感染人数比例分别为:腹腔70.15%、肺部41.15%、败血症11.97%、泌尿系统5.40%、胸腔4.89%,其他部位8.6%。64.76%的患者为单部位感染。微生物培养阳性率分别为:腹水22.70%、痰52.82%、尿40.63%、胸水35.71%。腹水中大肠埃希菌占首位(43.82%);痰液中肺炎克雷伯菌、铜绿假单胞菌和鲍曼不动杆菌分别占22.67%、24.00%、22.67%;血培养中大肠埃希菌和肺炎克雷伯菌分别占33.80%、29.58%,其次为葡萄球菌(15.49%)。ACLF合并细菌感染后90 d生存率为38.11%(226/593),多因素logistic回归分析结果显示年龄(P=0.006)、肝性脑病分期(P<0.001)、肝衰竭分期(P<0.001)和急性肾损伤(P<0.001)是影响ACLF合并细菌感染患者90 d生存的独立危险因素。 结论 ACLF合并细菌感染发生率高,90 d生存率较低,出现急性肾损伤、Ⅲ期以上肝性脑病或肝衰竭晚期时提示预后差。 Abstract:Objective To investigate the clinical features of infection in patients with acute-on-chronic liver failure (ACLF) and bacterial infection and the influencing factors for 90-day survival rate. Methods The patients with ACLF who were admitted to The Fifth Medical Center of Chinese PLA General Hospital from January 2014 to December 2015 were enrolled, and related clinical data were collected and analyzed, including infection time and site, microbial culture, biochemical parameters and inflammatory markers, and 28- and 90-day prognosis after infection. The t-test or the Mann-Whitney U test was used for comparison of continuous data between two groups, and the chi-square test was used for comparison of categorical data between two groups. The life-table method was used to plot survival curves. The indices affecting prognosis in the univariate analysis were further included in the multivariate logistic regression analysis. Results A total of 1074 patients with ACLF were admitted, among whom 609 had bacterial infection, and the incidence rate of bacterial infection was 56.7%. Among these 609 patients, 16 underwent liver transplantation within 90 days and related data statistics were obtained for the remaining 593 patients. As for infection site, among the patients with infection, 70.15% had abdominal infection, 41.15% had pulmonary infection, 11.97% had sepsis, 5.40% had urinary system infection, 4.89% had thoracic infection, and 8.6% had infection at other sites. Among the patients with infection, 64.76% had infection at a single site. The positive rates of microbial culture of ascites, phlegm, urine, and pleural effusion were 22.70%, 52.82%, 40.63%, and 35.71%, respectively. Escherichia coli was the most common bacterium in ascites and accounted for 43.82%; Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter baumannii accounted for 22.67%, 24.00%, and 22.67%, respectively, in phlegm; Escherichia coli, Klebsiella pneumoniae, and Staphylococcaceae accounted for 33.80%, 29.58%, and 15.49%, respectively, in blood culture. The 90-day survival rate after infection was 38.11% (226/593) in the patients with ACLF, and the multivariate logistic regression analysis showed that age (P=0.006), stage of hepatic encephalopathy (HE) (P < 0.001), stage of liver failure (P < 0.001), and acute kidney injury (AKI) (P < 0.001) were independent risk factors for 90-day survival in patients with ACLF and infection. Conclusion There is a high incidence rate of infection in patients with ACLF. The 90-day survival rate is relatively low, and the presence of AKI, HE stage III or above, and advanced liver failure may indicate poor prognosis. -
Key words:
- Acute-On-Chronic Liver Failure /
- Bacterial Infections /
- Prognosis
-
表 2 不同部位细菌培养阳性情况
细菌 腹腔感染(n=89) 肺炎(n=75) 败血症(n=71) 尿路感染(n=13) 胸腔感染(n=9) 革兰阴性菌[例(%)] 大肠埃希菌 39(43.82) 4(5.33) 24(33.80) 3(23.08) 2(22.22) 肺炎克雷伯菌 8(8.99) 17(22.67) 21(29.58) 0 4(44.44) 铜绿假单胞菌 0 18(24.00) 2(2.82) 0 0 鲍曼不动杆菌 4(4.49) 17(22.67) 3(4.23) 0 0 嗜麦芽寡养单胞菌 0 8(10.67) 3(4.23) 0 0 其他 6(6.74) 0 2(2.82) 2(15.38) 0 革兰阳性菌[例(%)] 链球菌 5(5.62) 4(5.33) 3(4.23) 0 1(11.11) 葡萄球菌 10(11.24) 7(9.33) 11(15.49) 2(15.38) 1(11.11) 肠球菌 12(13.48) 0 0 6(46.15) 2(22.22) 其他 5(5.62) 0 2(2.82) 0 0 表 3 生存组和死亡组单因素分析结果
指标 存活组(n=226) 死亡组(n=367) 统计值 P值 男/女(例) 189/37 295/72 χ2=0.983 0.321 年龄(岁) 47.38±10.68 51.49±11.89 t=4.248 <0.001 病因(HBV/酒精/自身免疫性/药物/其他,例) 159/45/10/1/11 229/76/19/13/30 χ2=18.732 0.002 肝硬化(有/无,例) 199/27 326/41 χ2=0.083 0.774 感染部位(单/多,例) 178/48 206/161 χ2=593.000 <0.001 腹水(有/无,例) 223/3 362/5 χ2=0.001 0.970 肝性脑病(无、Ⅰ/Ⅱ期、Ⅲ/Ⅳ期,例) 167/48/11 138/97/132 χ2=29.907 <0.001 肺部感染(有/无,例) 57/169 187/180 χ2=38.250 <0.001 自发性腹膜炎(有/无,例) 169/57 247/120 χ2=3.730 0.050 上消化道出血(有/无,例) 15/211 68/299 χ2=16.430 <0.001 败血症(有/无,例) 26/200 45/322 χ2=0.076 0.780 胸腔感染(有/无,例) 5/221 24/343 χ2=5.130 0.020 国际标准化比值 1.85±0.44 2.56±1.21 χ2=-8.460 <0.001 总胆红素(μmol/L) 303.27±137.06 335.81±158.53 t=-2.597 0.010 血肌酐(μmol/L) 106.70±67.63 152.48±125.37 t=-6.165 <0.001 白细胞(×109/L) 7.00(4.75~9.68) 8.34(5.43~13.07) Z=-3.883 <0.001 中性粒细胞(×109/L) 4.87(3.01~7.41) 6.18(3.78~10.48) Z=-4.645 <0.001 降钙素原(ng/ml) 0.70(0.39~1.45) 0.79(0.42~1.91) Z=-1.955 0.050 C反应蛋白(g/L) 16.78(9.28~36.30) 17.60(9.64~36.11) Z=-0.937 0.349 乳酸(mmol/L) 1.56(1.25~2.01) 1.69(1.28~2.73) Z=-1.837 0.066 肝衰竭分期(早期/中期/晚期,例) 195/25/6 73/170/124 χ2=59.300 <0.001 MELD评分 22.71±6.18 27.99±8.29 t=-7.971 <0.001 表 4 影响ACLF合并感染患者90 d生存的多因素logistic回归分析
指标 B值 SE Wald Exp(B) 95%CI P值 年龄 -0.038 0.014 7.442 0.963 0.937~0.989 0.006 自发性腹膜炎 -0.214 0.440 0.236 0.807 0.341~1.913 0.627 肝性脑病分期 23.332 <0.001 Ⅰ/Ⅱ期vs无 2.409 0.508 22.523 11.128 4.114~30.099 <0.001 Ⅲ/Ⅳ期vs无 1.860 0.546 11.603 6.427 2.203~18.747 0.001 急性肾损伤 -1.288 0.315 16.744 0.276 0.149~0.511 <0.001 白细胞 -0.014 0.024 0.366 0.986 0.941~1.032 0.545 总胆红素 -0.001 0.001 1.183 0.999 0.997~1.001 0.277 血肌酐 0.000 0.002 0.017 1.000 0.996~1.003 0.896 肝衰竭分期 19.104 <0.001 中期vs早期 1.954 0.449 18.933 7.057 2.927~17.017 <0.001 晚期vs早期 1.463 0.466 9.838 4.318 1.731~10.772 0.002 降钙素原 -0.101 0.063 2.633 0.903 0.799~1.021 0.105 常量 -1.153 1.023 1.270 0.316 0.260 -
[1] LIU XY, CHEN J, TONG JJ, et al. The causes of death and clinical characteristic of patients with HBV-ACLF[J]. Chin J Hepatol, 2015, 23(9): 704-706. DOI: 10.3760/cma.j.issn.1007-3418.2015.09.015.刘晓燕, 陈婧, 童晶晶, 等. 393例乙型肝炎病毒相关慢加急性肝衰竭死亡患者死因及临床特征分析[J]. 中华肝脏病杂志, 2015, 23(9): 704-706. DOI: 10.3760/cma.j.issn.1007-3418.2015.09.015. [2] BAJAJ JS, O'LEARY JG, REDDY KR, et al. Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures[J]. Hepatology, 2014, 60(1): 250-256. DOI: 10.1002/hep.27077. [3] MOREAU R, JALAN R, GINES P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis[J]. Gastroenterology, 2013, 144(7): 1426-1437. DOI: 10.1053/j.gastro.2013.02.042. [4] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, CMA; Severe Liver Diseases and Artificial Liver Group, Chinese Society of Hepatology, CMA. Guideline for diagnosis and treatment of liver failure (2012 version)[J]. Chin J Clin Infect Dis, 2012, 5(6): 321-327. DOI: 10.3760/cma.j.issn.1674-2397.2012.06.001.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2012年版)[J]. 中华临床感染病杂志, 2012, 5(6): 321-327. DOI: 10.3760/cma.j.issn.1674-2397.2012.06.001. [5] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of ascites and complications in cirrhosis[J]. J Clin Hepatol, 2017, 33(10): 1847-1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003.中华医学会肝病学分会. 肝硬化腹水及相关并发症的诊疗指南[J]. 临床肝胆病杂志, 2017, 33(10): 1847-1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003. [6] ANGELI P, GINÈS P, WONG F, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: Revised consensus recommendations of the International Club of Ascites[J]. J Hepatol, 2015, 62(4): 968-974. DOI: 10.1016/j.jhep.2014.12.029. [7] Society of Infectious Diseases, Chinese Medical Association. Expert consensus on diagnosis and treatment of end-stage liver disease complicated with infections[J]. J Clin Hepatol, 2018, 34(9): 1862-1872. DOI: 10.3969/j.issn.1001-5256.2018.09.008.中华医学会感染病学分会. 终末期肝病合并感染诊治专家共识[J]. 临床肝胆病杂志, 2018, 34(9): 1862-1872. DOI: 10.3969/j.issn.1001-5256.2018.09.008. [8] FERNÁNDEZ J, ACEVEDO J, WIEST R, et al. Bacterial and fungal infections in acute-on-chronic liver failure: Prevalence, characteristics and impact on prognosis[J]. Gut, 2018, 67(10): 1870-1880. DOI: 10.1136/gutjnl-2017-314240. [9] ARVANITI V, D'AMICO G, FEDE G, et al. Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis[J]. Gastroenterology, 2010, 139(4): 1246-1256. DOI: 10.1053/j.gastro.2010.06.019. [10] JALAN R, FERNANDEZ J, WIEST R, et al. Bacterial infections in cirrhosis: A position statement based on the EASL Special Conference 2013[J]. J Hepatol, 2014, 60(6): 1310-1324. DOI: 10.1016/j.jhep.2014.01.024. [11] BAJAJ JS, O'LEARY JG, TANDON P, et al. Hepatic encephalopathy is associated with mortality in patients with cirrhosis independent of other extrahepatic organ failures[J]. Clin Gastroenterol Hepatol, 2017, 15(4): 565-574. DOI: 10.1016/j.cgh.2016.09.157. [12] LIU XY, XIN SJ, CHEN J, et al. Significance of liver failure staging in predicting the prognosis of HBV-acute-on-chronic liver failure[J]. Acad J Chin PLA Med Sch, 2014, 35(6): 521-524, 544. DOI: 10.3969/j.issn.2095-5227.2014.06.001.刘晓燕, 辛绍杰, 陈婧, 等. 肝衰竭分期对HBV感染慢加急性肝衰竭预后判断的意义[J]. 解放军医学院学报, 2014, 35(6): 521-524, 544. DOI: 10.3969/j.issn.2095-5227.2014.06.001. [13] GUPTA S, JASWANI P, SHARMA RK, et al. Procalcitonin as a diagnostic biomarker of sepsis: A tertiary care centre experience[J]. J Infect Public Health, 2019, 12(3): 323-329. DOI: 10.1016/j.jiph.2018.11.004. [14] CHOI JJ, MCCARTHY MW. Novel applications for serum procalcitonin testing in clinical practice[J]. Expert Rev Mol Diagn, 2018, 18(1): 27-34. DOI: 10.1080/14737159.2018.1407244. 期刊类型引用(2)
1. 鞠迪,李汨,韩曼,房冰莹,闫曙光,安荣,李京涛. 益脾养肝方对肝癌前病变大鼠肝星状细胞活化的影响. 陕西中医药大学学报. 2024(02): 83-88 .  百度学术
百度学术2. 黄玉,苟雪源,关茜,焦俊喆,闫曙光,常占杰,闫瑞娟,李京涛. 基于M1型巨噬细胞极化-慢性炎症-肝细胞恶变探究益脾养肝方治疗肝癌前病变作用机制. 中国中医药信息杂志. 2024(10): 81-88 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 2088 KB)
PDF下载 ( 2088 KB)

 下载:
下载:
 百度学术
百度学术

