Value of albumin-bilirubin grade in predicting liver function changes and prognosis of hepatocellular carcinoma patients undergoing transarterial chemoembolization: A Meta-analysis
-
摘要:
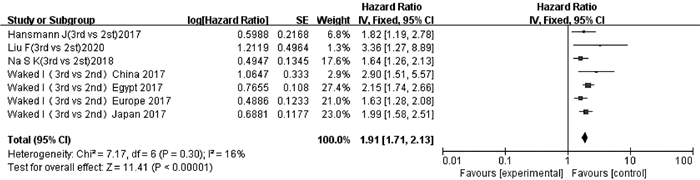
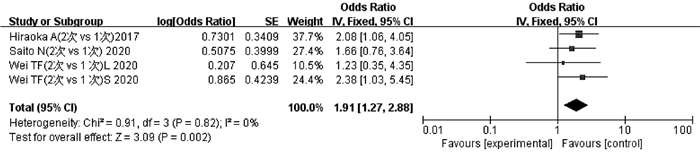
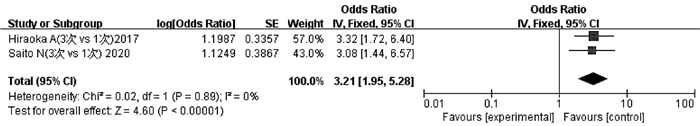
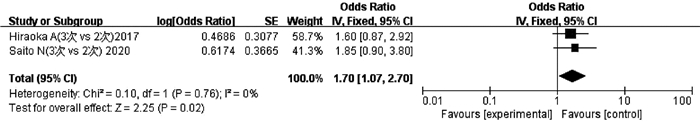
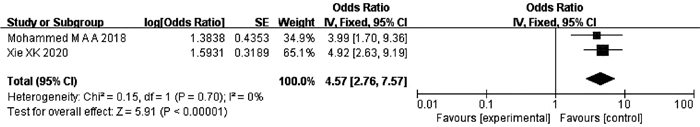
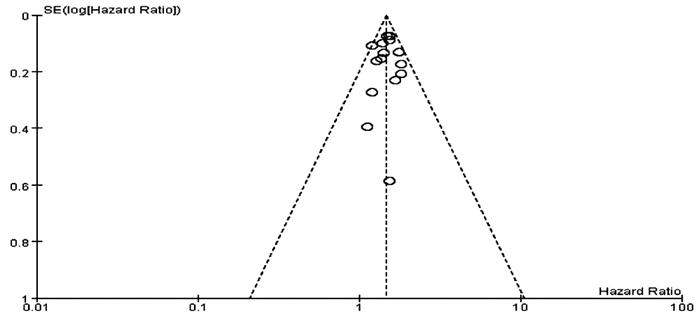
目的 分析白蛋白-胆红素(ALBI)分级对肝细胞癌(HCC)患者经肝动脉化疗栓塞术(TACE)后肝功能变化及其预后的评估价值。 方法 计算机检索PubMed、The Cochrane Library、EMbase、Web of Science、OVID、知网、万方、维普及中国生物医学文献数据库,收集所有关于ALBI分级对TACE治疗HCC患者肝功能变化及其预后评估的相关性研究,检索时间为数据库建立至2020年12月。对纳入文献进行质量评价及数据提取后,采用RevMan 5.3软件进行Meta分析。各研究间的异质性采用χ2检验判断;用HR或OR及其对应的95%CI评价结局指标;通过漏斗图评价发表偏倚。 结果 共纳入18篇文献,9940例患者。Meta分析结果显示:较高ALBI等级的HCC患者TACE后总生存期(OS)短于较低ALBI等级患者(2nd vs 1st:HR=1.48,95%CI:1.39~1.57,P<0.000 01;3rd vs 1st:HR=2.45,95%CI:1.92~3.13,P<0.000 01;3rd vs 2nd:HR=1.91,95%CI:1.71~2.13,P<0.000 01)。2次TACE累积导致的ALBI恶化程度高于1次TACE(OR=1.91,95%CI:1.27~2.88,P<0.05),3次TACE累积导致的ALBI恶化程度高于1次TACE(OR=3.21,95%CI:1.95~5.28,P<0.05),3次TACE累积导致的ALBI恶化程度高于2次TACE(OR=1.70,95%CI:1.07~2.70,P<0.05)。此外,ALBI可以预测TACE后慢加急性肝衰竭(ACLF)的发生(OR=4.57,95%CI:2.76~7.57,P<0.000 01)。 结论 重复TACE治疗可导致肝功能持续恶化,并且ALBI分级对于评估TACE的预后及预测ACLF发生风险具有重要临床价值。 -
关键词:
- ALBI分级 /
- 癌, 肝细胞 /
- 化学栓塞, 治疗性 /
- 预后 /
- Meta分析(主题)
Abstract:Objective To investigate the value of albumin-bilirubin (ALBI) grade in evaluating liver function changes and prognosis of hepatocellular carcinoma (HCC) patients undergoing transarterial chemoembolization (TACE). Methods PubMed, the Cochrane Library, EMbase, Web of Science, OVID, CNKI, Wanfang Data, VIP, and CBM databases were searched for studies on ALBI grade for evaluating liver function changes and prognosis of HCC patients undergoing TACE published up to December 2020. After quality assessment and data extraction, RevMan 5.3 was used to perform a meta-analysis of the studies included. The chi-square test was used to evaluate heterogeneity between studies; hazard ratio (HR)/odds ratio (OR) and corresponding 95% confidence interval (CI) were used to evaluate outcome measures; funnel plots were used to assess publication bias. Results A total of 18 articles were included, with 9940 patients in total. The meta-analysis showed that the HCC patients with higher ALBI grades after TACE had a shorter overall survival time than those with lower ALBI grades (2nd vs 1st: HR=1.48, 95%CI: 1.39-1.57, P < 0.000 01; 3rd vs 1st: HR=2.45, 95%CI: 1.92-3.13, P < 0.000 01; 3rd vs 2nd: HR=1.91, 95%CI: 1.71-2.13, P < 0.000 01). The degree of deterioration of ALBI caused by 2 times of TACE was higher than that caused by 1 time of TACE (OR=1.91, 95%CI: 1.27-2.88, P < 0.05); the degree of deterioration of ALBI caused by 3 times of TACE was higher than that caused by 1 time of TACE (OR=3.21, 95%CI: 1.95-5.28, P < 0.05); the degree of deterioration of ALBI caused by 3 times of TACE was higher than that caused by 2 times of TACE (OR=1.70, 95%CI: 1.07-2.70, P < 0.05). In addition, ALBI grade could predict the onset of acute-on-chronic liver failure (ACLF) after TACE (OR=4.57, 95%CI: 2.76-7.57, P < 0.000 01). Conclusion Repeated TACE treatment can cause continuous deterioration of liver function based on ALBI, and ALBI has an important clinical value in predicting prognosis and the risk of ACLF after TACE. -
表 1 纳入文献基本特征表
第一作者及年份 国家 研究合作 样本量(例) 男/女(例) ALBI分级 结局指标 HR/OR(95%CI) 提取方式 质量等级 Ho等[13]2017 中国 单中心 881 673/208 Ⅰ~Ⅲ OS 2nd vs 1st:1.531(1.285~1.823),3rd vs 1st:1.525(0.976~2.382) R(M) A Waked等[14]2017 埃及 多中心 3030 2769/261 Ⅰ~Ⅲ OS Europe 2nd vs 1st:1.48(1.28~1.71),3rd vs1st:2.59 (1.99~3.38),3rd vs 2nd:1.63(1.28~2.06)
Japan 2nd vs 1st:1.37(1.01~1.87),3rd vs 1st:2.66 (1.77~4.00),3rdvs2nd:1.99(1.58~2.51)
Egypt 2nd vs 1st:1.43(1.10~1.86),3rd vs 1st:2.77 (2.00~3.84),3rd vs 2nd:2.15(1.74~2.65)
China 2nd vs 1st:1.21(0.71~2.05),3rd vs 1st:4.54 (1.71~12.05),3rd vs 2nd:2.90(1.51~5.57)E(U) B Zhao等[15]2020 中国 单中心 221 194/27 Ⅰ~Ⅱ OS 2nd vs 1st:1.83(1.22~2.74) E(U) B Kim等[16]2018 韩国 单中心 476 381/95 Ⅰ~Ⅲ OS 2nd vs 1st:1.77(1.37~2.30),3rd vs 1st:7.11 (3.98~12.7) R(M) B Na等[17]2018 韩国 单中心 905 - Ⅰ~Ⅲ OS 2nd vs 1st:1.40(1.15~1.71),3rd vs 1st:2.02 (1.48~2.75),3rd vs 2nd:1.64(1.26~2.14) E(U) B Zhong等[18]2019 中国 多中心 548 448/100 Ⅰ~Ⅲ OS 2nd vs 1st:1.193(0.964~1.476),3rd vs 1st:1.922(1.180~3.132) R(M) B Carling等[19]2019 挪威 单中心 49 38/11 I~II OS 2nd vs 1st:1.13(0.52~2.46) E(U) B 王哲轩等[20]2020 中国 单中心 185 159/26 Ⅰ~Ⅱ OS 2nd vs 1st:1.82(1.29~2.59) R(M) A 刘芳等[21]2020 中国 单中心 129 104/25 I~III OS 2nd vs 1st:1.54(0.49~4.80),3rd vs 1st:4.74 (1.14~19.71),3rd vs 2nd:3.36(1.27~8.89) R(M) B 黄海等[22]2019 中国 单中心 119 88/31 I~III OS 2nd vs 1st:1.67(1.06~2.63),3rd vs 1st:2.47 (1.53~3.99) R(M) A 张争运等[23]2019 中国 单中心 233 198/35 I~II OS 2nd vs 1st:1.29(0.94~1.77) E(U) B Lee等[24]2019 韩国 单中心 1715 1470/440 Ⅰ~Ⅲ OS 2nd vs 1st:1.55(1.34~1.79),3rd vs 1st:1.39 (1.02~1.89) R(M) B Hansmann等[25]2017 美国 单中心 180 142/38 Ⅱ~Ⅲ OS 3rd vs 2nd:1.82(1.19~2.79) E(U) A Hiraoka等[26]2017 日本 单中心 212 163/49 Ⅰ~Ⅱ 肝功能恶化 2次TACE vs 1次TACE:2.08(1.06~4.05) 3次TACE vs 1次TACE:3.32(1.72~6.40) 3次TACE vs 2次TACE:1.60(0.87~2.92) E(U) B Saito等[27]2020 日本 单中心 113 84/29 Ⅰ~Ⅱ 肝功能恶化 2次TACE vs 1次TACE:1.66(0.76~3.64) 3次TACE vs 1次TACE:3.08(1.44~6.57) 3次TACE vs 2次TACE:1.85(0.90~3.80) E(U) A 魏庭丰等[28]2020 中国 单中心 110 72/18 Ⅰ~Ⅱ 肝功能恶化 2次TACE vs 1次TACE:1.23(0.35~4.35)(Long-term) 2次TACE vs 1次TACE:2.38(1.03~5.45)(Short-term) 谢雪焜等[29]2020 中国 单中心 711 628/83 Ⅰ~Ⅱ ACLF 4.919(2.633~9.188) R(M) A Mohammed等[30]2018 德国 单中心 123 81/42 Ⅱ~Ⅲ ACLF 3.99(1.70~9.40) R(M) B 注:E(U),估计值(单变量);R(M),报告值(多变量);OS,总生存期;2nd vs 1st,ALBI 2 vs ALBI 1;3rd vs 1st,ALBI 3 vs ALBI1;3rd vs 2nd,ALBI 3 vs ALBI 2。 表 2 Meta分析结果
分析 研究数目 合并的HR(95%CI) P值 异质性 I2值 P值 研究区域 China 5 2.09(1.62~2.70) <0.001 35% 0.190 Korean 3 2.01(1.63~2.46) <0.001 92% <0.001 Japan 1 2.66(1.77~4.00) <0.001 - - Egypt 1 2.77(2.00~3.84) <0.001 - - Europe 1 2.59(1.99~3.37) <0.001 - - 样本量 <400 3 2.90(1.90~4.43) <0.001 0 0.370 >400 6 2.24(1.97~2.54) <0.001 78% <0.001 HR提取方式 E(U) 6 2.54(2.17~2.96) <0.001 0 0.480 R(M) 5 1.95(1.61~2.37) <0.001 84% <0.001 -
[1] BRAY F, FERLAY J, SOERJOMATARAM I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2018, 68(6): 394-424. DOI: 10.3322/caac.21492. [2] FERLAY J, SOERJOMATARAM I, DIKSHIT R, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012[J]. Int J Cancer, 2015, 136(5): E359-386. DOI: 10.1002/ijc.29210. [3] FORNER A, REIG M, BRUIX J. Hepatocellular carcinoma[J]. Lancet, 2018, 391(10127): 1301-1314. DOI: 10.1016/S0140-6736(18)30010-2. [4] XU D, YUAN WD. Clinical efficacy of hepatic artery chemoembolization in the treatment of patients with primary liver cancer[J]. J Prac Hepatol, 2015, 18(2): 195-196. DOI: 10.3969/j.issn.1672-5069.2015.02.024.胥栋, 袁伟东. 肝动脉插管化疗栓塞术治疗原发性肝癌临床疗效分析[J]. 实用肝脏病杂志, 2015, 18(2): 195-196. DOI: 10.3969/j.issn.1672-5069.2015.02.024. [5] Bureau of Medical Administration, National Health Commission of the People's Republic of China. Guidelines for diagnosis and treatment of primary liver cancer in China (2019 edition)[J]. J Clin Hepatol, 2020, 36(2): 277-292. DOI: 10.3969/j.issn.1001-5256.2020.02.007.中华人民共和国国家卫生健康委员会医政医管局. 原发性肝癌诊疗规范(2019年版)[J]. 临床肝胆病杂志, 2020, 36(2): 277-292. DOI: 10.3969/j.issn.1001-5256.2020.02.007. [6] LLOVET JM, BRÚ C, BRUIX J. Prognosis of hepatocellular carcinoma: The BCLC staging classification[J]. Semin Liver Dis, 1999, 19(3): 329-338. DOI: 10.1055/s-2007-1007122. [7] WIESNER R, EDWARDS E, FREEMAN R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers[J]. Gastroenterology, 2003, 124(1): 91-96. DOI: 10.1053/gast.2003.50016. [8] JOHNSON PJ, BERHANE S, KAGEBAYASHI C, et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade[J]. J Clin Oncol, 2015, 33(6): 550-558. DOI: 10.1200/JCO.2014.57.9151. [9] XU Q, YAN Y, GU S, et al. A Novel inflammation-based prognostic score: The fibrinogen/albumin ratio predicts prognoses of patients after curative resection for hepatocellular carcinoma[J]. J Immunol Res, 2018, 2018: 4925498. DOI: 10.1155/2018/4925498. [10] GKIKA E, BETTINGER D, KRAFFT L, et al. The role of albumin-bilirubin grade and inflammation-based index in patients with hepatocellular carcinoma treated with stereotactic body radiotherapy[J]. Strahlenther Onkol, 2018, 194(5): 403-413. DOI: 10.1007/s00066-017-1256-0. [11] SAMAWI HH, SIM HW, CHAN KK, et al. Prognosis of patients with hepatocellular carcinoma treated with sorafenib: A comparison of five models in a large Canadian database[J]. Cancer Med, 2018, 7(7): 2816-2825. DOI: 10.1002/cam4.1493. [12] HAYDEN JA, CĈTÉ P, BOMBARDIER C. Evaluation of the quality of prognosis studies in systematic reviews[J]. Ann Intern Med, 2006, 144(6): 427-437. DOI: 10.7326/0003-4819-144-6-200603210-00010. [13] HO SY, LIU PH, HSU CY, et al. Prognostic role of noninvasive liver reserve markers in patients with hepatocellular carcinoma undergoing transarterial chemoembolization[J]. PLoS One, 2017, 12(7): e0180408. DOI: 10.1371/journal.pone.0180408. [14] WAKED I, BERHANE S, TOYODA H, et al. Transarterial chemo-embolisation of hepatocellular carcinoma: Impact of liver function and vascular invasion[J]. Br J Cancer, 2017, 116(4): 448-454. DOI: 10.1038/bjc.2016.423. [15] ZHAO S, ZHANG T, LI H, et al. Comparison of albumin-bilirubin grade versus Child-Pugh score in predicting the outcome of transarterial chemoembolization for hepatocellular carcinoma using time-dependent ROC[J]. Ann Transl Med, 2020, 8(8): 538. DOI: 10.21037/atm.2020.02.124. [16] KIM JH, SINN DH, LEE JH, et al. Novel albumin-bilirubin grade-based risk prediction model for patients with hepatocellular carcinoma undergoing chemoembolization[J]. Dig Dis Sci, 2018, 63(4): 1062-1071. DOI: 10.1007/s10620-018-4934-6. [17] NA SK, YIM SY, SUH SJ, et al. ALBI versus Child-Pugh grading systems for liver function in patients with hepatocellular carcinoma[J]. J Surg Oncol, 2018, 117(5): 912-921. DOI: 10.1002/jso.24992. [18] ZHONG BY, NI CF, JI JS, et al. Nomogram and artificial neural network for prognostic performance on the albumin-bilirubin grade for hepatocellular carcinoma undergoing transarterial chemoembolization[J]. J Vasc Interv Radiol, 2019, 30(3): 330-338. DOI: 10.1016/j.jvir.2018.08.026. [19] CARLING U, RØSOK B, LINE PD, et al. ALBI and P-ALBI grade in Child-Pugh A patients treated with drug eluting embolic chemoembolization for hepatocellular carcinoma[J]. Acta Radiol, 2019, 60(6): 702-709. DOI: 10.1177/0284185118799519. [20] WANG ZX, WANG EX, XIA DD, et al. Value of Child-Pugh score versus albumin-bilirubin grade in predicting the prognosis of unresectable hepatocellular carcinoma treated by transarterial chemoembolization[J]. J Clin Hepatol, 2020, 36(1): 113-117. DOI: 10.3969/j.issn.1001-5256.2020.01.025.王哲轩, 王恩鑫, 夏冬东, 等. Child-Pugh评分和ALBI分级预测经肝动脉化疗栓塞治疗不可切除肝细胞癌预后的价值比较[J]. 临床肝胆病杂志, 2020, 36(1): 113-117. DOI: 10.3969/j.issn.1001-5256.2020.01.025. [21] LIU F, ZHOU YF. Child-Pugh score and albumin-bilirubin classification in prognostic value of patients with hepatocellular carcinoma undergoing arterial chemoembolization[J]. Sma Healt, 2020, 6(11): 135-136. DOI: 10.19335/j.cnki.2096-1219.2020.11.052.刘芳, 周英发. Child-Pugh评分和白蛋白-胆红素分级在肝细胞癌经动脉化疗栓塞患者中预后的价值[J]. 智慧健康, 2020, 6(11): 135-136. DOI: 10.19335/j.cnki.2096-1219.2020.11.052. [22] HUANG H, ZHU Y, BAO ZJ. Prognostic factors of elderly patients with hepatocellular carcinoma undergoing transcatheter arte-rial chemoembolization[J]. Prac Geri, 2019, 33(6): 577-581. DOI: 10.3969/j.issn.1003-9198.2019.06.015.黄海, 竺越, 保志军. 肝动脉化疗栓塞术治疗老年肝癌病人的疗效及预后影响因素分析[J]. 实用老年医学, 2019, 33(6): 577-581. DOI: 10.3969/j.issn.1003-9198.2019.06.015. [23] ZHANG ZY, ZHANG GL, WAN L, et al. Prognostic value of ALBI grading in patients with hepatocellular carcinoma treated with repeated TACE[J]. Tumor, 2019, 39(9): 722-729. DOI: 10.3781/j.issn.1000-7431.2019.33.203.张争运, 张国梁, 万霖, 等. ALBI分级对反复行TACE治疗肝细胞癌患者预后评估的价值[J]. 肿瘤, 2019, 39(9): 722-729. DOI: 10.3781/j.issn.1000-7431.2019.33.203. [24] LEE SK, SONG MJ, KIM SH, et al. Comparing various scoring system for predicting overall survival according to treatment modalities in hepatocellular carcinoma focused on Platelet-albumin-bilirubin (PALBI) and albumin-bilirubin (ALBI) grade: A nationwide cohort study[J]. PLoS One, 2019, 14(5): e0216173. DOI: 10.1371/journal.pone.0216173. [25] HANSMANN J, EVERS MJ, BUI JT, et al. Albumin-bilirubin and platelet-albumin-bilirubin grades accurately predict overall survival in high-risk patients undergoing conventional transarterial chemoembolization for hepatocellular carcinoma[J]. J Vasc Interv Radiol, 2017, 28(9): 1224-1231. e2. DOI: 10.1016/j.jvir.2017.05.020. [26] HIRAOKA A, KUMADA T, KUDO M, et al. Hepatic function during repeated TACE procedures and prognosis after introducing sorafenib in patients with unresectable hepatocellular carcinoma: Multicenter analysis[J]. Dig Dis, 2017, 35(6): 602-610. DOI: 10.1159/000480256. [27] SAITO N, TANAKA T, NISHIOHUKU H, et al. Transarterial- chemoembolization remains an effective therapy for intermediate-stage hepatocellular carcinoma with preserved liver function[J]. Hepatol Res, 2020, 50(10): 1176-1185. DOI: 10.1111/hepr.13550. [28] WEI TF, HE SC, ZHU HD, et al. The impact of different intervals between two TACE procedures on the short-term liver functions in patients with hepatocellular carcinoma[J]. J Interv Radiol, 2020, 29(11): 1126-1130. DOI: 10.3969/j.issn.1008-794X.2020.11.014.魏庭丰, 何仕诚, 朱海东, 等. 原发性肝癌肝动脉化疗栓塞治疗间隔长短对近期肝功能影响的比较[J]. 介入放射学杂志, 2020, 29(11): 1126-1130. DOI: 10.3969/j.issn.1008-794X. 2020.11.014. [29] XIE XK, WANG ZY, CHEN XX, et al. Value of four scoring systems in predicting liver failure after transcatheter arterial che-moembolization in patients with hepatocellular carcinoma[J]. Chin J Clin Oncol, 2020, 47(12): 614-620. DOI: 10.3969/j.issn.1000-8179. 2020.12.347.谢雪焜, 王宗玉, 陈欣欣, 等. 4种评分系统预测肝细胞癌患者经肝动脉化疗栓塞术后肝衰竭的价值[J]. 中国肿瘤临床, 2020, 47(12): 614-620. DOI: 10.3969/j.issn.1000-8179.2020.12.347. [30] MOHAMMED M, KHALAF MH, LIANG T, et al. Albumin-bilirubin score: An accurate predictor of hepatic decompensation in high-risk patients undergoing transarterial chemoembolization for hepatocellular carcinoma[J]. J Vasc Interv Radiol, 2018, 29(11): 1527-1534. e1. DOI: 10.1016/j.jvir.2018.06.016. [31] de LOPE CR, TREMOSINI S, FORNER A, et al. Management of HCC[J]. J Hepatol, 2012, 56(Suppl 1): s75-s87. DOI: 10.1016/S0168-8278(12)60009-9. [32] BRUIX J, SHERMAN M. Management of hepatocellular carcinoma: An update[J]. Hepatology, 2011, 53(3): 1020-1022. DOI: 10.1002/hep.24199. [33] CHILD CG, TURCOTTE JG. Surgery and portal hypertension[J]. Major Probl Clin Surg, 1964, 1: 1-85. [34] PUGH RN, MURRAY-LYON IM, DAWSON JL, et al. Transection of the oesophagus for bleeding oesophageal varices[J]. Br J Surg, 1973, 60(8): 646-649. DOI: 10.1002/bjs.1800600817. [35] JOHNSON PJ, WILLIAMS R. Cirrhosis and the aetiology of hepatocellular carcinoma[J]. J Hepatol, 1987, 4(1): 140-147. DOI: 10.1016/s0168-8278(87)80021-1. [36] DURAND F, VALLA D. Assessment of prognosis of cirrhosis[J]. Semin Liver Dis, 2008, 28(1): 110-122. DOI: 10.1055/s-2008-1040325. [37] BAǦIRSAKÇI E, ŞAHIN E, ATABEY N, et al. Role of albumin in growth inhibition in hepatocellular carcinoma[J]. Oncology, 2017, 93(2): 136-142. DOI: 10.1159/000471807. [38] CHAN AW, CHONG CC, MO FK, et al. Incorporating albumin-bilirubin grade into the cancer of the liver Italian program system for hepatocellular carcinoma[J]. J Gastroenterol Hepatol, 2017, 32(1): 221-228. DOI: 10.1111/jgh.13457. [39] CHAN AW, CHONG CC, MO FK, et al. Applicability of albumin-bilirubin-based Japan integrated staging score in hepatitis B-associated hepatocellular carcinoma[J]. J Gastroenterol Hepatol, 2016, 31(10): 1766-1772. DOI: 10.1111/jgh.13339. [40] CHAN AW, KUMADA T, TOYODA H, et al. Integration of albumin-bilirubin (ALBI) score into Barcelona Clinic Liver Cancer (BCLC) system for hepatocellular carcinoma[J]. J Gastroenterol Hepatol, 2016, 31(7): 1300-1306. DOI: 10.1111/jgh.13291. [41] SHAO YY, LIU TH, LEE YH, et al. Modified CLIP with objective liver reserve assessment retains prognosis prediction for patients with advanced hepatocellular carcinoma[J]. J Gastroenterol Hepatol, 2016, 31(7): 1336-1341. DOI: 10.1111/jgh.13312. [42] LAU WY, LAI ECH. Loco-regional intervention for hepatocellular carcinoma[J]. J Intervent Med, 2019, 2(2): 43-46. DOI: 10.1016/jJimed.2019.07.001. [43] WANG JC, LAO XM. Research progress on HBV DNA and liver function changes after TACE of HBV-induced hepatocellular carcinoma[J]. New Chin Med, 2016, 47(5): 290-294. DOI: 10.3969/j.issn.0253-9802.2016.05.003.王骏成, 劳向明. HBV相关肝癌TACE术后HBV-DNA及肝功能变化的研究进展[J]. 新医学, 2016, 47(5): 290-294. DOI: 10.3969/j.issn.0253-9802.2016.05.003. [44] LENCIONI R, de BAERE T, SOULEN MC, et al. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: A systematic review of efficacy and safety data[J]. Hepatology, 2016, 64(1): 106-116. DOI: 10.1002/hep.28453. [45] ZHANG CJ, HE SC, TENG GJ, et al. Analysis of related factors affecting liver function for hepatocellular carcinoma after transcatheter arterial chemoembolization[J]. J Southe Univ (Med Sci Edi), 2013, 32(1): 18-22. DOI: 10.3969/j.issn.1671-6264.2013.01.005.张成佳, 何仕诚, 滕皋军, 等. TACE治疗原发性肝癌对肝功能影响的相关因素分析[J]. 东南大学学报(医学版), 2013, 32(1): 18-22. DOI: 10.3969/j.issn.1671-6264.2013.01.005. [46] ARIZUMI T, MINAMI T, CHISHINA H, et al. Time to transcatheter arterial chemoembolization refractoriness in patients with hepatocellular carcinoma in Kinki Criteria Stages B1 and B2[J]. Dig Dis, 2017, 35(6): 589-597. DOI: 10.1159/000480208. [47] PECK-RADOSAVLJEVIC M, RAOUL JL, LEE HC, et al. OPTIMIS: An international observational study to assess the use of sorafenib after transarterial chemoembolization (TACE) in patients with hepatocellular carcinoma (HCC) [J]. J Clin Oncol, 2014, 32(15): TPS4155. DOI: 10.1200/jco.2014.32.15_suppl.tps4155. [48] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [49] HERNAEZ R, SOLÀ E, MOREAU R, et al. Acute-on-chronic liver failure: An update[J]. Gut, 2017, 66(3): 541-553. DOI: 10.1136/gutjnl-2016-312670. [50] HSIN IF, HSU CY, HUANG HC, et al. Liver failure after transarterial chemoembolization for patients with hepatocellular carcinoma and ascites: Incidence, risk factors, and prognostic prediction[J]. J Clin Gastroenterol, 2011, 45(6): 556-562. DOI: 10.1097/MCG.0b013e318210ff17. [51] CHAN AW, CHAN RC, WONG GL, et al. New simple prognostic score for primary biliary cirrhosis: Albumin-bilirubin score[J]. J Gastroenterol Hepatol, 2015, 30(9): 1391-1396. DOI: 10.1111/jgh.12938. [52] LIU PH, HSU CY, HSIA CY, et al. ALBI and PALBI grade predict survival for HCC across treatment modalities and BCLC stages in the MELD Era[J]. J Gastroenterol Hepatol, 2017, 32(4): 879-886. DOI: 10.1111/jgh.13608. -



 PDF下载 ( 3075 KB)
PDF下载 ( 3075 KB)


 下载:
下载: