Effectiveness and safety of two-step percutaneous transhepatic choledochoscopic lithotomy in treatment of complex hepatolithiasis
-
摘要:
目的 探讨两步法经皮肝穿刺胆道镜取石术(PTCSL)治疗复杂肝胆管结石的效果。 方法 回顾性分析2018年1月—2020年6月西安交通大学医学部附属三二〇一医院收治的118例复杂肝胆管结石患者的临床资料,按手术方式分为PTCSL组(n=60)及手术组(n=58), 术后两组患者通过电话及门诊随访0.5~3年。对比分析两组一般资料、围术期指标(包括手术时间、术中出血量、切口长度、术后肛门恢复排气排便时间、腹腔引流管拔除时间、住院时间),肝功能及炎性指标变化情况,术后并发症(胆漏、急性胆管炎、伤口感染、下肢静脉血栓形成)发生情况,结石清除率及复发率,生活质量等指标。计量资料两组间比较采用两独立样本t检验;组内不同时间段间比较采用配对t检验,计数资料两组间比较采用χ2检验。 结果 PTCSL组在手术时间、术中出血量、切口长度、术后肛门恢复排气排便时间、腹腔引流管拔除时间均少于手术组(P值均<0.05)。术后第1天,PTCSL组及手术组患者ALT水平均低于术前(P值均<0.05),AST水平低于术前(P值均<0.05),WBC水平高于术前(P值均<0.05);PTCSL组患者术后第1天ALT、AST、WBC水平均明显低于外科手术组(P值均<0.05)。PTCSL组在术后胆漏(5.0% vs 17.2%)、急性胆管炎(3.3% vs 13.8%)、伤口感染(1.7% vs 10.3%)、下肢静脉血栓发生率(1.7% vs 12.1%)均低于外科手术组(P值均<0.05)。PTCSL组结石清除率高于外科手术组(58.3% vs 37.9%),PTCSL组远期结石复发率(10.0% vs 20.7%)低于手术组(P值均<0.05)。PTCSL组术后各生存质量评分均高于手术组(P值均<0.05)。 结论 针对复杂肝胆管结石,两步法PTCSL可有效清除结石,术后康复快,复发率及并发症发生率低,预后生活质量高,是一种有效的可供选择的手术方式。 -
关键词:
- 胆石 /
- 两步法经皮肝穿刺胆道镜取石术 /
- 最小侵入性外科手术
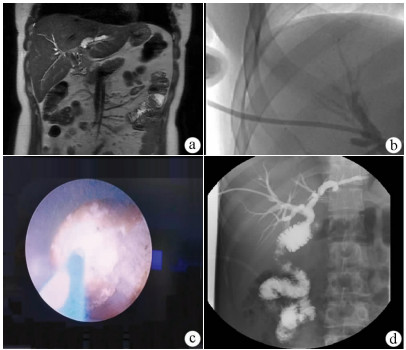
Abstract:Objective To investigate the clinical effect of two-step percutaneous transhepatic choledochoscopic lithotomy (PTCSL) in the treatment of complex hepatolithiasis. Methods A retrospective analysis was performed for the clinical data of 118 patients with complex hepatolithiasis who were admitted to 3201 Hospital of Xi'an Jiaotong University Health Science Center from January 2018 to June 2020, and according to the surgical procedure, they were divided into PTCSL group with 60 patients and surgery group with 58 patients. All patients were followed up for half a year to 3 years via telephone and outpatient service. The two groups were compared in terms of general information, perioperative indicators (including time of operation, intraoperative blood loss, incision length, time to first flatus and time to first defecation after surgery, time to extraction of abdominal drainage tube, and length of hospital stay), changes in liver function and inflammatory indicators, postoperative complications (bile leakage, acute cholangitis, wound infection, and venous thrombosis of lower extremities), stone clearance rate and recurrence rate, and quality of life. The two-independent-samples t-test was used for comparison of continuous data between two groups; the paired t-test was used for comparison between different periods of time within group; the chi-square test was used for comparison of categorical data between two groups. Results Compared with the surgery group, the PTCSL group had significantly shorter time of operation, time to first flatus and time to first defecation after surgery, and time to extraction of abdominal drainage tube, a significantly lower intraoperative blood loss, and a significantly shorter incision length (all P < 0.05). On day 1 after surgery, both groups had significant reductions in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) (P < 0.05) and a significant increase in white blood cell count (WBC) (P < 0.05), and the PTCSL group had significantly lower levels of ALT, AST, and WBC than the surgery group (all P < 0.05). Compared with the surgery group, the PTCSL group had significantly lower incidence rates of postoperative bile leakage (5.0% vs 17.2%, P < 0.05), acute cholangitis (3.3% vs 13.8%, P < 0.05), wound infection (1.7% vs 10.3%, P < 0.05), and venous thrombosis of lower extremities (1.7% vs 12.1%, P < 0.05). Compared with the surgery group, the PTCSL group had a significantly higher stone clearance rate (58.3% vs 37.9%, P < 0.05) and a significantly lower long-term stone recurrence rate (10.0% vs 20.7%, P < 0.05). The PTCSL group had significantly higher quality of life scores than the surgery group (all P < 0.05). Conclusion For the treatment of complex hepatolithiasis, two-step PTCSL can effectively remove stones, with the advantages of fast postoperative recovery, low recurrence rate and incidence rate of complications, and high quality of life, and therefore, it is an effective alternative surgical procedure. -
表 1 两组患者一般资料比较
项目 PTCSL组(n=60) 手术组(n=58) 统计值 P值 男/女(例) 32/28 29/29 χ2=0.131 0.717 年龄(岁) 60.75±14.54 60.95±16.01 t=-0.070 0.944 伴有慢性病[例(%)] 17(28.3) 16(27.6) χ2=0.008 0.928 美国麻醉师协会评分Ⅲ级[例(%)] 2(3.3) 2(3.4) χ2=0.001 0.972 表 2 两组患者围术期指标比较
项目 PTCSL组(n=60) 手术组(n=58) t值 P值 手术时间(min) 95.33±20.56 150.21±21.43 -14.195 <0.001 术中出血量(mL) 50.07±14.76 205.72±16.06 -54.850 <0.001 切口长度(cm) 1.83±0.46 8.02±2.32 -19.923 <0.001 术后肛门恢复排气排便时间(d) 0.97±0.37 1.91±0.35 -14.302 <0.001 腹腔引流管拔除时间(d) 4.48±0.59 6.81±0.62 -21.045 <0.001 住院时间(d) 12.63±2.48 12.24±3.96 0.642 0.522 表 3 两组患者围术期肝功能及炎性指标变化情况比较
项目 PTCSL组(n=60) 手术组(n=58) t值 P值 ALT(U/L) 术前 169.32±67.74 175.80±68.31 -0.517 0.606 术后第1天 67.63±24.741) 84.90±40.531) -2.805 0.006 AST(U/L) 术前 127.97±54.45 120.60±61.21 0.691 0.491 术后第1天 51.58±18.201) 82.93±44.411) -4.987 <0.001 WBC(×109/L) 术前 8.96±3.78 9.08±4.28 -0.169 0.866 术后第1天 10.77±3.851) 13.74±4.611) -3.809 <0.001 注:与同组术前比较,1)P<0.05。 表 4 两组患者术后并发症发生情况比较
术后并发症 PTCSL(n=60) 手术组(n=58) χ2值 P值 胆漏[例(%)] 3(5.0) 10(17.2) 4.508 0.034 急性胆管炎[例(%)] 2(3.3) 8(13.8) 4.160 0.041 伤口感染[例(%)] 1(1.7) 6(10.3) 3.980 0.046 下肢静脉血栓[例(%)] 1(1.7) 7(12.1) 5.049 0.025 表 5 两组患者结石清除率及远期复发率比较
结石清除率及复发率 PTCSL(n=60) 手术组(n=58) χ2值 P值 结石清除[例(%)] 35(58.3) 22(37.9) 10.92 <0.001 结石复发[例(%)] 6(10.0) 12(20.7) 7.84 <0.001 表 6 两组患者术后生存质量评分比较
评分 PTCSL(n=60) 手术组(n=58) t值 P值 总分(分) 术前 83.85±7.29 83.36±6.22 0.391 0.697 术后 129.07±9.901) 110.74±8.071) 11.003 <0.001 生理功能(分) 术前 8.70±2.14 8.33±1.888 1.003 0.318 术后 18.30±3.871) 15.12±3.261) 4.819 <0.001 社会活动(分) 术前 13.15±2.70 12.66±3.01 0.942 0.348 术后 16.53±4.351) 14.48±4.421) 2.541 0.012 主观症状(分) 术前 51.42±4.50 51.95±5.09 -0.602 0.548 术后 74.47±6.931) 65.93±6.451) 6.920 <0.001 心理情绪(分) 术前 10.58±3.00 10.43±3.00 0.276 0.783 术后 19.77±3.961) 15.21±3.761) 6.408 <0.001 注:与同组术前比较,1)P<0.05。 -
[1] DA COSTA AC, SANTA-CRUZ F, SENA BF, et al. Dedifferentiated liposarcoma of the gallbladder: First reported case[J]. World J Surg Oncol, 2018, 16(1): 221. DOI: 10.1186/s12957-018-1520-5. [2] LIU XW, CHENG Y, GONG JP. Value of percutaneous transhepatic lithotripsy in treatment of hepatolithiasis[J]. J Clin Hepatol, 2019, 35(7): 1640-1643. DOI: 10.3969/j.issn.1001-5256.2019.07.048.刘新文, 程瑶, 龚建平. 经皮经肝胆道镜碎石取石术治疗肝胆管结石的价值[J]. 临床肝胆病杂志, 2019, 35(7): 1640-1643. DOI: 10.3969/j.issn.1001-5256.2019.07.048. [3] LU H, YANG H, WU L, et al. A novel prognostic model for diagnosing atypical bile duct hyperplasia in patients with intrahepatic lithiasis[J]. Medicine (Baltimore), 2019, 98(17): e15364. DOI: 10.1097/MD.0000000000015364. [4] LI H, ZHENG J, CAI JY, et al. Laparoscopic VS open hepatectomy for hepatolithiasis: An updated systematic review and meta-analysis[J]. World J Gastroenterol, 2017, 23(43): 7791-7806. DOI: 10.3748/wjg.v23.i43.7791. [5] CHEN CH, LIN CL, KAO CH. Association between inflammatory bowel disease and cholelithiasis: A nationwide population-based cohort study[J]. Int J Environ Res Public Health, 2018, 15(3): 513. DOI: 10.3390/ijerph15030513. [6] Biliary Tract Group, Chinese Society of Surgery, Chinese Medical Association. The 2011 Chinese guidelines for the diagnosis and treatment of hepatolithiasis[M]. Beijing: People's Medical Publishing House(PMPH), 2011.中华医学会外科学分会胆道外科学组. 2011中国肝胆管结石病诊断治疗指南[M]. 北京: 人民卫生出版社, 2011. [7] XIA L, XIA YJ, ZHANG L, et al. Diagnosis and treatment of intrahepatic cholangiocarcinoma: Current status and thoughts[J]. J Clin Hepatol, 2020, 36(10): 2380-2385. DOI: 10.3969/j.issn.1001-5256.2020.10.048.夏龙, 夏医君, 张磊, 等. 肝内胆管细胞癌的诊疗现状与思考[J]. 临床肝胆病杂志, 2020, 36(10): 2380-2385. DOI: 10.3969/j.issn.1001-5256.2020.10.048. [8] CHEN ZS, TANG CW, TANG CH, et al. Research advances in the clinical diagnosis of intrahepatic cholangiocarcinoma[J]. J Clin Hepatol, 2019, 35(12): 2638-2643. DOI: 10.3969/j.issn.1001-5256.2019.12.005.陈志升, 唐陈伟, 汤朝晖, 等. 肝内胆管癌的临床诊断策略[J]. 临床肝胆病杂志, 2019, 35(12): 2638-2643. DOI: 10.3969/j.issn.1001-5256.2019.12.005. [9] WANG ZC. Curative effect of ERCP on senile patients with choledocholithiasis and its effect on serum inflammatory factors[J]. Traum Crit Med, 2019, 7(4): 233-235. DOI: 10.16048/j.issn.2095-5561.2019.04.12.王超智. 内镜下逆行胆胰管造影术对老年胆总管结石患者疗效研究[J]. 创伤与急危重病医学, 2019, 7(4): 233-235. DOI: 10.16048/j.issn.2095-5561.2019.04.12. [10] TIAN J, LI JW, CHEN J, et al. Laparoscopic hepatectomy with bile duct exploration for the treatment of hepatolithiasis: An experience of 116 cases[J]. Dig Liver Dis, 2013, 45(6): 493-498. DOI: 10.1016/j.dld.2013.01.003. [11] WANG P, SUN B, HUANG B, et al. Comparison between percutaneous transhepatic rigid cholangioscopic lithotripsy and conventional percutaneous transhepatic cholangioscopic surgery for hepatolithiasis treatment[J]. Surg Laparosc Endosc Percutan Tech, 2016, 26(1): 54-59. DOI: 10.1097/SLE.0000000000000222. [12] LU GS, WEN HQ, LIU YM. A experimental study on formation of fistula after percutaneous transhepatic cholangiodrainage (PTCD)[J]. China J Endosc, 2004, 10(11): 44-46, 50. DOI: 10.3969/j.issn.1007-1989.2004.11.016.陆光生, 文辉清, 刘衍民. 经皮肝穿刺胆道引流管周瘘道形成的实验研究[J]. 中国内镜杂志, 2004, 10(11): 44-46, 50. DOI: 10.3969/j.issn.1007-1989.2004.11.016. [13] HAN ZM, SHENG YH, ZHANG FK. Comparison of clinical effects between two different paths of percutaneous transhepatic cholangioscopy in treating complicated intrahepatic and extrahepatic bile duct stones[J]. J Hepatobiliary Surg, 2016, 24(6): 422-425. DOI: 10.3969/j.issn.1006-4761.2016.06.007.韩志敏, 盛银行, 张风奎. 经皮肝胆道镜术两种不同路径治疗复杂肝内外胆管结石的临床疗效比较[J]. 肝胆外科杂志, 2016, 24(6): 422-425. DOI: 10.3969/j.issn.1006-4761.2016.06.007. [14] JIANG XF, ZHANG DW, LU HW, et al. Clinical effective analysis of percutaneous transhepatic cholangioscopic lithotrip by rigid choledochoscopy for 194 patients with intrahepatic stones[J]. Chin J Pract Surg, 2017, 37(8): 896-899. DOI: 10.19538/j.cjps.issn1005-2208.2017.08.16.蒋小峰, 张大伟, 卢海武, 等. 经皮经肝胆道镜硬镜碎石术治疗肝内胆管结石194例临床疗效分析[J]. 中国实用外科杂志, 2017, 37(8): 896-899. DOI: 10.19538/j.cjps.issn1005-2208.2017.08.16. [15] LIU XY, LIU XM, ZHI XT. Comparative effect analysis on hepatolith patients by two different path percutaneous transhepatic cholangioscopic lithotripsy[J]. Chin J Curr Adv Gen Surg, 2015, 18(7): 530-532. DOI: 10.3969/j.issn.1009-9905.2015.07.009.刘晓洋, 刘晓明, 智绪亭. 两种不同PTCSL路径治疗肝胆管结石的临床效果比较[J]. 中国现代普通外科进展, 2015, 18(7): 530-532. DOI: 10.3969/j.issn.1009-9905.2015.07.009. [16] TAO HS, WANG P, SUN BW, et al. One-Step multichannel percutaneous transhepatic cholangioscopic lithotripsy applied in bilateral hepatolithiasis[J]. World J Surg, 2020, 44(5): 1586-1594. DOI: 10.1007/s00268-020-05368-7. [17] WU C, YOU W, ZHANG L, et al. Clinical efficacy of percutaneous transhepatic lithotripsy with one-step biliary fistulation for the treatment of hepatolithiasis[J]. Clin J Dig Surg, 2020, 19(8): 843-848. DOI: 10.3760/cma.j.cn115610-20200603-00416.吴琛, 游伟, 张龙, 等. Ⅰ期经皮经肝胆道造瘘胆道镜取石术治疗肝胆管结石病的临床疗效[J]. 中华消化外科杂志, 2020, 19(8): 843-848. DOI: 10.3760/cma.j.cn115610-20200603-00416. 期刊类型引用(4)
1. 徐萌,张磊. 基于科学知识图谱的职务犯罪文献计量应用. 数字技术与应用. 2022(02): 7-9 .  百度学术
百度学术2. 孙明珠. 院前急救气道管理的研究现状与前景可视化分析. 岭南急诊医学杂志. 2022(06): 550-553 .  百度学术
百度学术3. 李灵敏,李博,刘晓峰. 基于CiteSpace和VOSviewer的肠道菌群研究热点可视化分析. 现代消化及介入诊疗. 2021(08): 984-989 .  百度学术
百度学术4. 刘珊珊,王聪,杨智博,陈玉珍,雷常彬,蒋艳. 中心静脉导管相关性血流感染研究现状及热点的可视化分析. 护理研究. 2021(24): 4478-4483 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 1978 KB)
PDF下载 ( 1978 KB)

 下载:
下载:
 百度学术
百度学术

