人工肝支持系统治疗慢加急性肝衰竭效果的网状Meta分析
DOI: 10.3969/j.issn.1001-5256.2022.01.021
利益冲突声明:本研究不存在研究者、伦理委员会成员、受试者监护人以及与公开研究成果有关的利益冲突。
作者贡献声明:甘亮亮、张金周负责课题设计,资料分析,撰写论文;汤雪梅、傅彩虹、苏佳参与文献筛选,收集数据,修改论文;王贤东负责拟定写作思路,指导撰写文章并最后定稿。
Efficacy of artificial liver support system in treatment of acute-on-chronic liver failure: A network Meta-analysis
-
摘要:
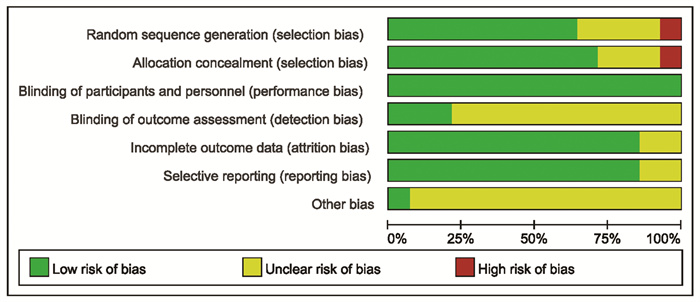
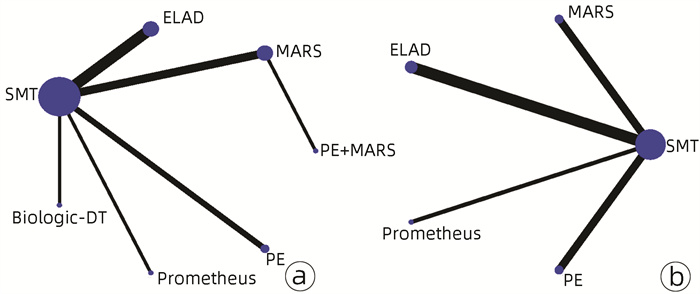
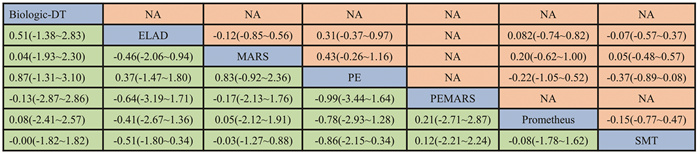
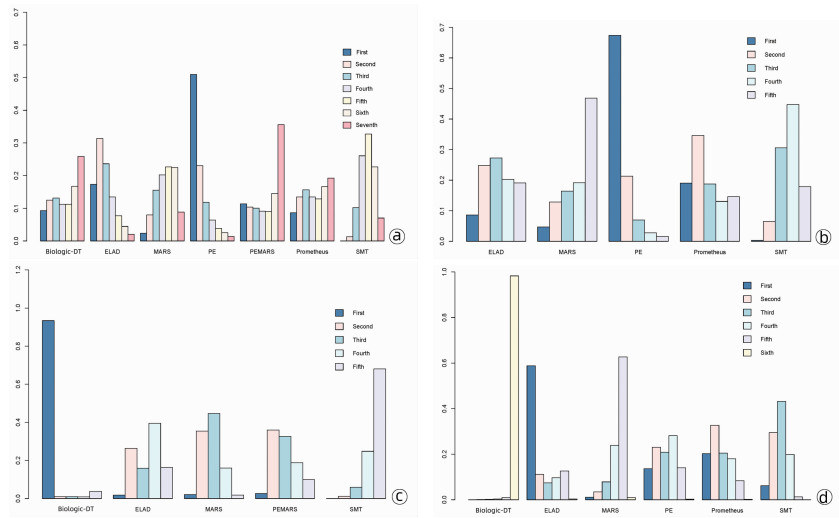
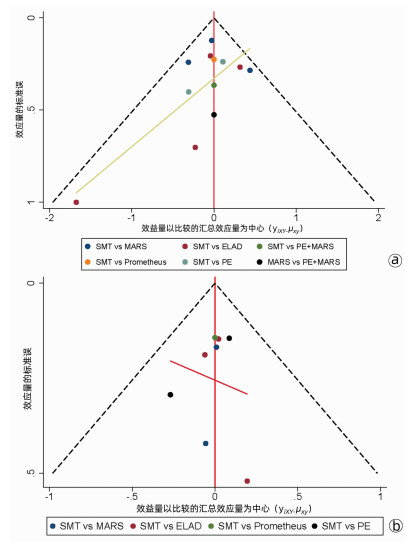
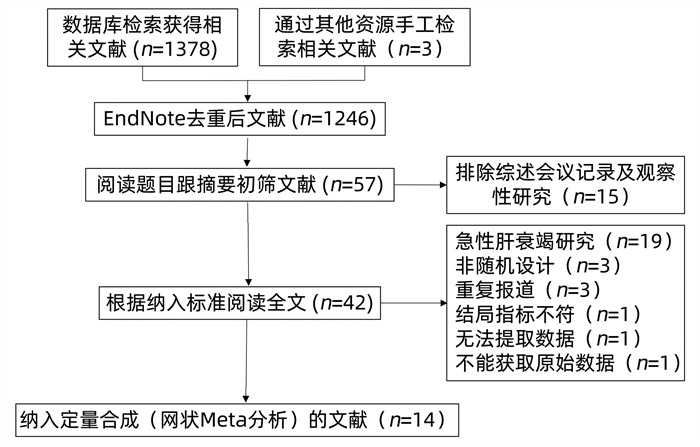
目的 采用网状Meta分析系统评价不同人工肝支持系统治疗慢加急性肝衰竭(ACLF)的疗效。 方法 计算机检索PubMed、EMBASE、Cochrane library、Clinical Trial、CNKI、SinoMed和万方数据库中关于不同形式人工肝治疗ACLF患者的随机对照试验。根据纳入排除标准进行文献筛选、资料提取及方法学质量评价,采用Stata15.1及R4.1.0软件进行网状Meta分析。 结果 共纳入14篇文献,共计1141例患者。网状Meta分析结果显示:不同干预方式交叉对比降低病死率差异均无统计学意义(P值均>0.05),排序概率图显示降低30 d病死率血浆置换(PE)最优,其他依次为体外细胞疗法(ELAD)、分级血浆分离吸附(Prometheus)、分子吸附再循环系统(MARS)、Biologic-DT肝脏透析设备、PE+MARS。降低90 d病死率PE最优,其他依次为Prometheus、ELAD、MARS。改善肝性脑病方面,Biologic-DT最优,其他依次为MARS、PE+MARS、ELAD。出血风险最低者为ELAD,与标准医学治疗(SMT)相比Biologic-DT可能增加出血风险(RR=1.9×108,95%CI: 4.6~6.2×1027)。 结论 PE可能是降低ACLF患者30 d及90 d病死率的最优选择。Biologic-DT可能在改善肝性脑病方面效果较好,但有可能增加出血风险。 -
关键词:
- 慢加急性肝功能衰竭 /
- 肝, 人工 /
- Meta分析(主题)
Abstract:Objective To systematically review the efficacy of different artificial liver support systems in the treatment of acute-on-chronic liver failure (ACLF) using a network Meta-analysis. Methods PubMed, Embase, the Cochrane library, Clinical Trial, CNKI, SinoMed, and Wanfang Data were searched for randomized controlled trials (RCTs) on different artificial liver support systems in the treatment of ACLF. Literature screening, data extraction, and method ological quality assessment were performed according to inclusion and exclusion criteria, and Stata15.1 software and R4.1.0 software were used to perform a network Meta-analysis. Results A total of 14 RCTs were included, with 1141 patients in total. The network meta-analysis showed different intervention methods had no significant difference in reducing mortality rate based on cross comparison (all P > 0.05). The probability ranking diagram showed that plasma exchange (PE) showed the best effect in reducing 30-day mortality rate, followed by extracorporeal liver assist device (ELAD), fractionated plasma separation and adsorption with Prometheus system, molecular adsorbent recirculating system (MARS), Biologic-DT liver dialysis device, and PE+MARS. PE showed the best effect in reducing 90-day mortality rate, followed by Prometheus, ELAD, and MARS. Biologic-DT showed the best effect in improving hepatic encephalopathy, followed by MARS, PE+MARS, and ELAD. Patients undergoing ELAD had the lowest risk of bleeding, and compared with standard medical treatment, Biologic-DT might increase the risk of bleeding [risk ratio=1.9×108, 95% confidence interval: (4.6-6.2)×1027]. Conclusion PE might be the best option for reducing 30- and 90-day mortality rates in ACLF patients. Biologic-DT has a better effect in improving hepatic encephalopathy, but it may increase the risk of bleeding. -
表 1 纳入研究的基本特质
研究 年份 国家 人群 病因 MELD Bañares R[13] 2013 欧洲 急性失代偿肝硬化 酒精、病毒、自身免疫、药物等 24.9 Duan Z[14] 2018 中国 慢性重型肝炎 HBV、酒精、自身免疫、药物等 29.4 Hassanein TI[15] 2007 美国 肝硬化失代偿并肝性脑病 酒精、病毒、自身免疫、药物等 30.5 Heemann U[16] 2002 德国 急性失代偿肝硬化 酒精、病毒、自身免疫、中毒 - Hillebrand DJ[17] 2010 美国 急性失代偿肝硬化 - 37.6 Huang YK[18] 2012 中国 慢性重型乙型肝炎合并肝性脑病 HBV - Kramer L[19] 2001 奥地利 肝硬化并肝性脑病 酒精、病毒、自身免疫、隐源性 - Kribben A[20] 2012 欧洲 急性失代偿慢性肝病 酒精、病毒、其他 27.5 Laleman W[21] 2006 比利时 酒精性肝硬化并酒精性肝炎 酒精 25.6 Mitzner SR[22] 2000 德国 急性失代偿肝硬化 酒精、病毒、自身免疫、布加病 - Qin G[23] 2014 中国 慢性重型乙型肝炎急性加重 HBV 29.1 Sen S[24] 2004 英国 急性失代偿酒精性肝病 酒精 18 Thompson J[25] 2018 美国、英国 重症酒精性肝炎 酒精 27.4 周锐[12] 2012 中国 慢性重型乙型肝炎 HBV 30.8 研究 例数 平均年龄(岁) 男性(%) 干预方式 干预情况 随访时间 Bañares R[13] 179 50.9 68.7 MARS vs SMT 6.8 h,6.5次 91 d Duan Z[14] 49 39.4 93.9 ELAD vs SMT 持续68.1 h 5年 Hassanein TI[15] 70 52.5 51.4 MARS vs SMT 4 h,2.7次 180 d Heemann U[16] 24 52.5 45.8 ELAD vs SMT 6 h,3~10次 6个月 Hillebrand DJ[17] 18 - - ELAD vs SMT 持续122.8 h 90 d Huang YK[18] 120 42.5 76.7 MARS vs PE+MARS MARS 2.1次 30 d Kramer L[19] 20 55.5 65 Biologic-DT vs SMT 6 h 30 d Kribben A[20] 145 50.5 63.4 Prometheus vs SMT 5.7 h,8.1次 90 d Laleman W[21] 18 51.2 66.7 MARS vs Prometheus vs SMT 6 h,3次 7 d Mitzner SR[22] 13 46.7 38.5 MARS vs SMT 6~8 h,5.25次 30 d Qin G[23] 234 46.4 76.9 PE vs SMT 2.1 h,2次 5~10年 Sen S[24] 18 44.5 72.2 MARS vs SMT 8 h,4次 90 d Thompson J[25] 203 45.7 47.8 ELAD vs SMT 持续0~120 h 91 d 周锐[12] 30 40.5 76.7 PE vs SMT 2.5~4 h,2~7次 6~24个月 注:MARS,分子吸附在循环系统;ELAD,体外细胞疗法;Prometheus,分级血浆分离吸附;PE,血浆置换。 -
[1] SARIN SK, CHOUDHURY A, SHARMA MK, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific association for the study of the liver (APASL): An update[J]. Hepatol Int, 2019, 13(4): 353-390. DOI: 10.1007/s12072-019-09946-3. [2] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association, Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure (2018)[J]. J Clin Hepatol, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [3] ARROYO V, MOREAU R, JALAN R. Acute-on-chronic liver failure[J]. N Engl J Med, 2020, 382(22): 2137-2145. DOI: 10.1056/NEJMra1914900. [4] ARTRU F, LOUVET A, RUIZ I, et al. Liver transplantation in the most severely ill cirrhotic patients: A multicenter study in acute-on-chronic liver failure grade 3[J]. J Hepatol, 2017, 67(4): 708-715. DOI: 10.1016/j.jhep.2017.06.009. [5] OLIVO R, GUARRERA JV, PYRSOPOULOS NT. Liver transplantation for acute liver failure[J]. Clin Liver Dis, 2018, 22(2): 409-417. DOI: 10.1016/j.cld.2018.01.014. [6] ALSHAMSI F, ALSHAMMARI K, BELLEY-COTE E, et al. Extracorporeal liver support in patients with liver failure: A systematic review and meta-analysis of randomized trials[J]. Intensive Care Med, 2020, 46(1): 1-16. DOI: 10.1007/s00134-019-05783-y. [7] KHUROO MS, KHUROO MS, FARAHAT KL. Molecular adsorbent recirculating system for acute and acute-on-chronic liver failure: A meta-analysis[J]. Liver Transpl, 2004, 10(9): 1099-1106. DOI: 10.1002/lt.20139. [8] STUTCHFIELD BM, SIMPSON K, WIGMORE SJ. Systematic review and meta-analysis of survival following extracorporeal liver support[J]. Br J Surg, 2011, 98(5): 623-631. DOI: 10.1002/bjs.7418. [9] KJAERGARD LL, LIU J, ALS-NIELSEN B, et al. Artificial and bioartificial support systems for acute and acute-on-chronic liver failure: A systematic review[J]. JAMA, 2003, 289(2): 217-222. DOI: 10.1001/jama.289.2.217. [10] VAID A, CHWEICH H, BALK EM, et al. Molecular adsorbent recirculating system as artificial support therapy for liver failure: A meta-analysis[J]. ASAIO J, 2012, 58(1): 51-59. DOI: 10.1097/MAT.0b013e31823fd077. [11] STERNE J, SAVOVI C ' J, PAGE MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials[J]. BMJ, 2019, 366: l4898. DOI: 10.1136/bmj.l4898. [12] ZHOU R, GAN QR, ZHENG CX, et al. Analysis on the effects of artificial liver support system on prognosis of patients with later period of chronic severe hepatitis B and selection of proper analytical method[J/CD]. Chin J Exp Clin Infect Dis(Electronic Edition), 2012, 6(3): 186-190. DOI: 10.3877/cma.j.issn.1674-1358.2012.03.003.周锐, 甘巧蓉, 郑彩霞, 等. 人工肝对晚期慢性乙型重型肝炎预后影响及分析方法的选择[J/CD]. 中华实验和临床感染病杂志(电子版), 2012, 6(3): 186-190. DOI: 10.3877/cma.j.issn.1674-1358.2012.03.003. [13] BAÑARES R, NEVENS F, LARSEN FS, et al. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: The RELIEF trial[J]. Hepatology, 2013, 57(3): 1153-1162. DOI: 10.1002/hep.26185. [14] DUAN Z, XIN S, ZHANG J, et al. Comparison of extracorporeal cellular therapy (ELAD(®)) vs standard of care in a randomized controlled clinical trial in treating Chinese subjects with acute-on-chronic liver failure[J]. Hepat Med, 2018, 10: 139-152. DOI: 10.2147/HMER.S180246. [15] HASSANEIN TI, TOFTENG F, BROWN RS Jr, et al. Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis[J]. Hepatology, 2007, 46(6): 1853-1862. DOI: 10.1002/hep.21930. [16] HEEMANN U, TREICHEL U, LOOCK J, et al. Albumin dialysis in cirrhosis with superimposed acute liver injury: A prospective, controlled study[J]. Hepatology, 2002, 36(4 Pt 1): 949-958. DOI: 10.1053/jhep.2002.36130. [17] HILLEBRAND DJ, FREDERICK RT, WILLIAMS WW, et al. Safety and efficacy of the Extracorporeal Liver Assist Device (ELAD®) in patients with acute on chronic liver failure[J]. J Hepatol, 2010, 52: s323-s324. DOI: 10.1016/S0168-8278(10)60830-6. [18] HUANG YK, TAN DM, XIE YT, et al. Randomized controlled study of plasma exchange combined with molecular adsorbent re-circulating system for the treatment of liver failure complicated with hepatic encephalopathy[J]. Hepatogastroenterology, 2012, 59(117): 1323-1326. DOI: 10.5754/hge12203. [19] KRAMER L, GENDO A, MADL C, et al. A controlled study of sorbent suspension dialysis in chronic liver disease and hepatic encephalopathy[J]. Int J Artif Organs, 2001, 24(7): 434-442. http://www.onacademic.com/detail/journal_1000041651484399_80ae.html [20] KRIBBEN A, GERKEN G, HAAG S, et al. Effects of fractionated plasma separation and adsorption on survival in patients with acute-on-chronic liver failure[J]. Gastroenterology, 2012, 142(4): 782-789. e3. DOI: 10.1053/j.gastro.2011.12.056. [21] LALEMAN W, WILMER A, EVENEPOEL P, et al. Effect of the molecular adsorbent recirculating system and Prometheus devices on systemic haemodynamics and vasoactive agents in patients with acute-on-chronic alcoholic liver failure[J]. Crit Care, 2006, 10(4): R108. DOI: 10.1186/cc4985. [22] MITZNER SR, STANGE J, KLAMMT S, et al. Improvement of hepatorenal syndrome with extracorporeal albumin dialysis MARS: Results of a prospective, randomized, controlled clinical trial[J]. Liver Transpl, 2000, 6(3): 277-286. DOI: 10.1002/lt.500060326. [23] QIN G, SHAO JG, WANG B, et al. Artificial liver support system improves short- and long-term outcomes of patients with HBV-associated acute-on-chronic liver failure: A single-center experience[J]. Medicine (Baltimore), 2014, 93(28): e338. DOI: 10.1097/MD.0000000000000338. [24] SEN S, DAVIES NA, MOOKERJEE RP, et al. Pathophysiological effects of albumin dialysis in acute-on-chronic liver failure: A randomized controlled study[J]. Liver Transpl, 2004, 10(9): 1109-1119. DOI: 10.1002/lt.20236. [25] THOMPSON J, JONES N, AL-KHAFAJI A, et al. Extracorporeal cellular therapy (ELAD) in severe alcoholic hepatitis: A multinational, prospective, controlled, randomized trial[J]. Liver Transpl, 2018, 24(3): 380-393. DOI: 10.1002/lt.24986. [26] TOFT N, INNOCENT GT, GETTINBY G, et al. Assessing the convergence of Markov Chain Monte Carlo methods: An example from evaluation of diagnostic tests in absence of a gold standard[J]. Prev Vet Med, 2007, 79(2-4): 244-256. DOI: 10.1016/j.prevetmed.2007.01.003. [27] MEZZANO G, JUANOLA A, CARDENAS A, et al. Global burden of disease: Acute-on-chronic liver failure, a systematic review and meta-analysis[J]. Gut, 2021. DOI: 10.1136/gutjnl-2020-322161.[Epub ahead of print]. [28] MEDZHITOV R. Inflammation 2010: New adventures of an old flame[J]. Cell, 2010, 140(6): 771-776. DOI: 10.1016/j.cell.2010.03.006. [29] SARIN SK, CHOUDHURY A. Acute-on-chronic liver failure: Terminology, mechanisms and management[J]. Nat Rev Gastroenterol Hepatol, 2016, 13(3): 131-149. DOI: 10.1038/nrgastro.2015.219. [30] GARCÍA MARTÍNEZ JJ, BENDJELID K. Artificial liver support systems: What is new over the last decade?[J]. Ann Intensive Care, 2018, 8(1): 109. DOI: 10.1186/s13613-018-0453-z. [31] TAN EX, WANG MX, PANG J, et al. Plasma exchange in patients with acute and acute-on-chronic liver failure: A systematic review[J]. World J Gastroenterol, 2020, 26(2): 219-245. DOI: 10.3748/wjg.v26.i2.219. -



 PDF下载 ( 4674 KB)
PDF下载 ( 4674 KB)

 下载:
下载: