腹腔镜胆囊切除术中吲哚菁绿胆道造影精准识别胆总管的应用
DOI: 10.3969/j.issn.1001-5256.2022.01.025
Application of indocyanine green cholangiography in accurate identification of the common bile duct in laparoscopic cholecystectomy
-
摘要:
目的 胆总管损伤是腹腔镜胆囊切除术(LC)中的常见并发症。采用吲哚菁绿(ICG)术中显影的方法精准识别胆总管,以期降低腹腔镜胆囊切除术中胆总管损伤的发生率。 方法 纳入珠海市人民医院2021年4月— 6月行LC患者68例,其中行常规LC患者56例,ICG胆道造影引导下LC患者12例。常规LC组患者用腹腔镜白光、ICG胆道造影组用近红外光检查胆总管、胆囊管和胆囊。采用倾向评分匹配法对两组术前数据进行平衡。采用t检验和χ2检验比较两组术中出血量、手术时间、术后住院时间及胆总管损伤发生率。 结果 胆道造影组术中出血量、手术时间、术后住院时间及并发症发生率分别为(3.1±0.9)mL,(20.2±1.6)min,(1.2± 0.3)d和0;明显低于常规组的(10.8±2.3)mL,(48.3±5.1)min,(2.3±0.8)d和8.3%(t值分别为-22.709、-19.856、-19.507,χ2=1.287,P值均<0.05)。 结论 ICG胆道造影是LC术中鉴别胆总管和胆囊管的有效方法,可有效预防胆总管的损伤。方法胆道辨识度更高、起效时间长、可重复使用、操作方便,并可联合术中导航设备,在应用于胆囊结石患者的治疗中具有明显优势。 -
关键词:
- 胆囊切除术, 腹腔镜 /
- 胆管造影术 /
- 吲哚花青绿
Abstract:Objective To investigate the application of intraoperative indocyanine green (ICG) cholangiography in the accurate identification of the common bile duct since common bile duct injury is a common complication of laparoscopic cholecystectomy (LC), and to reduce the incidence rate of common bile duct injury during LC. Methods A total of 68 patients who underwent LC in Zhuhai People's Hospital from April 2021 to Jane 2021 were enrolled, among whom 56 patients underwent conventional LC and 12 patients underwent LC under the guidance of ICG cholangiography. The common bile duct, cystic duct, and gallbladder were examined by white light laparoscopy for the conventional LC group and near-infrared laparoscopy for the ICG cholangiography group. The propensity score matching method was used to balance the preoperative data between the two groups. The t-test and the chi-square test were used for comparison of intraoperative blood loss, time of operation, length of postoperative hospital stay, and incidence rate of common bile duct injury between the two groups. Results Compared with the conventional LC group, the ICG cholangiography group had significantly lower intraoperative blood loss 3.1±0.9 mL vs 10.8±2.3 mL, t=-22.709, P < 0.05), significantly shorter time of operation (20.2±1.6 min vs 48.3±5.1 min, t=-19.856, P < 0.05) and length of postoperative hospital stay (1.2±0.3 days vs 2.3±0.8 days, t=-19.507, P < 0.05), and a significantly lower incidence rate of complications (0 vs 8.3%, χ2=1.287, P < 0.05). Conclusion ICG cholangiography is an effective method to differentiate between the common bile duct and the cystic duct during LC and can prevent common bile duct injury. This method has great advantages in the treatment of patients with gallstones due to its high degree of identification of the biliary tract, long onset time, repeated application, convenient operation, and ability to be combined with intraoperative navigation device. -
Key words:
- Cholecystectomy, Laparoscopic /
- Cholangiography /
- Indocyanine Green
-
第1例腹腔镜胆囊切除术(laparoscopic cholecystectomy,LC)于20世纪80年代末被报道,其具有手术创伤小、术后恢复快、疗效好等优点,目前在世界范围内得到了广泛应用;而胆总管损伤是LC的常见并发症,发生率为0.4%~0.6%[1-6],可导致严重后果。如胆管壁损伤需要胆管缝合或T管引流,而胆总管横断伤则需要胆总管空肠吻合术或Roux-en-Y吻合术。而这些补救措施往往需要将LC中转为开放手术,极大地增加患者的经济负担和身体疼痛。考虑到胆总管损伤的严重性和普遍性,有效预防胆总管损伤的方法亟待应用。
引起胆总管损伤的原因多样,包括胆道解剖变异、胆囊炎反复发作引起胆总管变形、操作人员经验不足及器械不当等[7-12]。可以认为,准确识别胆总管是预防胆总管损伤的有效方法。因而从20世纪80年代至今,人们为准确识别胆总管和胆囊管做出了巨大努力;尝试过的方法如术中X线造影,但不易操作,且X线会给患者和操作者带来辐射风险[13];而术中超声成像也不易用于胆总管的识别。
近红外造影术于近年来兴起,其中吲哚菁绿(indocyanine green, ICG)造影术最为简便[14],被广泛应用于各类外科手术,包括肿瘤边界识别、甲状旁腺保护、肝段切除、乳腺癌前哨淋巴结活检等[15]。与其他方法相比,ICG造影安全性高。据报道[16],仅0.001 67%的患者对ICG发生过敏反应。且ICG使用方便,可于术前经静脉注射,如于术前24 h予ICG 25 mg以显影肝癌边界;术前50 s给予7.5 mg ICG以鉴别甲状旁腺;术前10 min予ICG 1 mg协助乳腺癌前哨淋巴结活检[15];离断操作前3 min予ICG 5 mg行肠血运灌注评估等[17]。
此前已有研究[18-19]对术中ICG胆道造影鉴别胆总管和胆囊管方法的有效性和安全性进行了评估,但此法的长期效果仍需进一步确认。本研究首次应用倾向评分匹配法比较了ICG胆道造影组和常规LC组患者中胆总管损伤的发生率,探讨ICG胆道造影的应用效果。
1. 资料和方法
1.1 研究对象
选取珠海市人民医院2021年4月—6月行LC患者。纳入标准:经超声、CT或MRI检查并结合病史确诊为胆囊良性疾病需行LC的患者。排除标准:急性胆囊炎、胰腺炎、血管性胆囊炎和胆总管结石;胆囊穿刺引流,引流管未拔出者;有心脏、肺部等基础疾病,不宜手术者;美国麻醉师学会评分≥2分。
将同意接受ICG胆道造影的患者纳入ICG胆道造影组,其余纳入常规LC对照组。常规LC组患者用腹腔镜白光,ICG胆道造影组用近红外光检查胆总管、胆囊管和胆囊。采用倾向评分匹配法对两组患者进行基线指标的平衡。
1.2 术前评估
所有患者术前均行心电图、胸部X线检查、超声、CT、血型、血常规、凝血功能、感染性疾病筛查、肝肾功能检查等。所有检查结果正常的患者可安排手术。有其他基础疾病的患者,需经相关专科和麻醉科会诊确认可耐受全麻。对所有患者术前均进行LC围手术期注意事项的宣教;另对ICG胆道造影组患者进行ICG胆道造影知识宣教;其他术前准备按上腹部手术常规进行。
1.3 手术方式
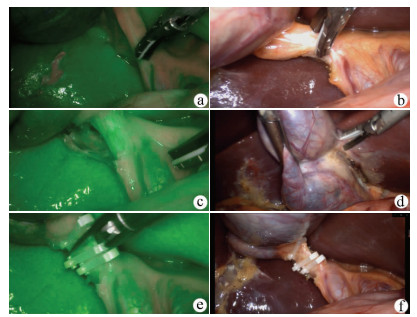
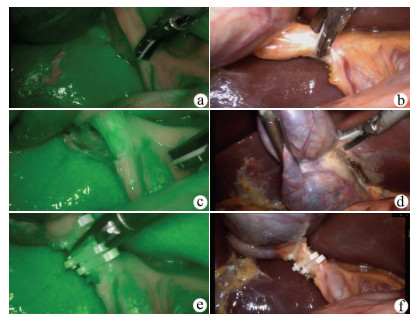
两组患者均行LC。患者头部抬高30°,身体左倾30°。全麻后建立静脉通路,用插入式Veress针头向腹腔内注入CO2。于脐下行一1 cm切口。经脐下套管针导入腹腔镜。在胆囊的体表投影处行一0.5 cm切口,于剑突下行一1 cm切口。将腹腔镜器械置入腹腔,解剖Calot三角。夹闭切断胆囊管和胆囊动脉。取胆囊送病理检查。关闭皮肤切口,视情况放置腹腔引流管(图 1)。
1.4 ICG的注射
对ICG胆道造影组患者于术前30 min(切皮前60 min)静脉注射ICG (瑞度,丹东医药)0.4 mg·kg-1·mL-1(基于ICG在血液中浓度于2 h达到最大值的原理确定此给药时间)。
1.5 荧光成像系统
荧光成像系统由近红外光源、控制手柄、腹腔镜、脚踏开关、设备摄像机和显示屏组成。该系统可作为常规腹腔镜手术系统呈现全彩色图像,并可在操作者踩下脚踏开关后发出波长约800 nm的近红外光用于ICG胆道造影;专门设计的腹腔镜可传输近红外光;通过操作控制手柄,术者可拍摄术中ICG胆道造影的照片或视频。
1.6 ICG胆道造影中胆管的识别
ICG胆道造影组在夹闭胆囊管前后,应用ICG胆道造影排除异位胆管的存在,并区分胆总管和胆囊管。所有的手术操作完成后,2名术者需用ICG胆道造影2次检查胆囊管残端,确保胆总管完好。比较2组术中出血量、手术时间、术后住院时间及胆总管损伤发生率。
1.7 伦理学审查
本研究方案经由珠海市人民医院伦理委员会审批,批号:2019-02;并在中国临床试验注册中心注册,注册号:ChiCTR1900024594。
1.8 统计学方法
采用SPSS 25.0进行统计分析。正态分布的计量资料采用x±s表示,2组间比较采用t检验;计数资料2组间比较采用χ2检验。多元逻辑回归模型评估每位受试者的倾向性得分。协变量包括以下基线特征:年龄、性别、复杂性胆结石等。P<0.05为差异有统计学意义。
2. 结果
2.1 基线特征
共纳入68例行LC患者,其中ICG胆道造影组12例,常规LC组56例,患者基线特征如表 1所示。行倾向评分匹配后,获得12对患者。匹配后,两组患者的基线变量差异被有效校正,两组患者特征比较,差异均无统计学意义(P值均>0.05)。
表 1 ICG胆道造影组和常规LC组患者匹配前后基线特征比较项目 匹配前 匹配后 常规LC组(n=56) ICG胆道造影组(n=12) 标准化差异(%) P值 常规LC组(n=12) ICG胆道造影组(n=12) 标准化差异(%) P值 年龄(岁) 53.2±6.5 63.7±5.1 19.7 0.001 57.1±8.3 57.2±9.6 0.18 0.372 男/女(例) 39/27 8/4 28.3 0.001 8/4 8/4 0 >0.05 复杂性胆结石(例) 21 3 33.3 0.006 3 3 0 >0.05 2.2 治疗结果
ICG胆道造影组和常规LC组治疗结果见表 2,ICG胆道造影组术中出血量、手术时间、术后住院时间、胆总管损伤发生率与常规LC组比较,差异均有统计学意义(P值均<0.05)。常规组出现胆总管周围组织出血1例(8.3%),患者进行了止血药保守处理后于术后1周内康复。所有切除的胆囊均显示良性病理结果。
表 2 ICG胆道造影组和常规LC组患者的手术效果比较项目 ICG胆道造影组(n=12) 常规LC组(n=12) 统计值 P值 手术时间(min) 20.2±1.6 48.3±5.1 t=-19.856 <0.01 术中出血量(mL) 3.1±0.9 10.8±2.3 t=-22.709 <0.01 胆总管相关损伤[例(%)] 0 1(8.3) χ2=1.287 0.013 住院时间(d) 1.2±0.3 2.3±0.8 t=-19.507 <0.01 3. 讨论
常规LC在手术过程中有发生胆总管损伤的风险,而胆总管的医源性损伤主要与外科医师对胆道的认识不准确有关。ICG胆道造影可通过显示胆囊管和胆总管的结构来预防术中胆总管损伤;本项研究表明,在LC中,ICG胆道造影可确保对胆总管和胆囊管的准确识别,有效区分胆总管与胆囊管的结构,准确解剖Calot三角,从而有效保护胆总管。
ICG过敏反应是最严重的并发症,但发生率极低;Perry等[16]研究显示,ICG过敏反应仅为1/80 000,并且术前碘过敏实验可预测及预防ICG过敏的发生。
本研究结果显示,ICG胆道造影组中无患者发生胆总管损伤;常规组出现胆总管周围组织出血1例,患者进行了止血保守处理后于术后1周内康复。且两组在术中手术时间、术中出血量、术后住院时间等方面均有显著性差异。究其原因,常规LC常需剥离胆管周围组织以显示其形态及结构,此过程将不可避免造成失血,并延长手术时间;而ICG胆道造影可直接显示胆总管及胆囊管结构,无需剥离周围组织,从而避免术中出血,并缩短手术时间,显示出ICG胆道造影在LC中的显著优势。
本研究为ICG胆道造影预防LC术中胆总管损伤的有效性和安全性提供了依据。由于ICG胆道造影具有效果好、精密性和准确性高、安全性强、可对狭窄胆道进行显影等优点,有望成为LC治疗胆囊结石时重要的辅助方法。然而本研究的样本量较少,需在未来招募更多患者、增加病例数量以更进一步的深入研究。
-
表 1 ICG胆道造影组和常规LC组患者匹配前后基线特征比较
项目 匹配前 匹配后 常规LC组(n=56) ICG胆道造影组(n=12) 标准化差异(%) P值 常规LC组(n=12) ICG胆道造影组(n=12) 标准化差异(%) P值 年龄(岁) 53.2±6.5 63.7±5.1 19.7 0.001 57.1±8.3 57.2±9.6 0.18 0.372 男/女(例) 39/27 8/4 28.3 0.001 8/4 8/4 0 >0.05 复杂性胆结石(例) 21 3 33.3 0.006 3 3 0 >0.05 表 2 ICG胆道造影组和常规LC组患者的手术效果比较
项目 ICG胆道造影组(n=12) 常规LC组(n=12) 统计值 P值 手术时间(min) 20.2±1.6 48.3±5.1 t=-19.856 <0.01 术中出血量(mL) 3.1±0.9 10.8±2.3 t=-22.709 <0.01 胆总管相关损伤[例(%)] 0 1(8.3) χ2=1.287 0.013 住院时间(d) 1.2±0.3 2.3±0.8 t=-19.507 <0.01 -
[1] ISMAEL HN, COX S, COOPER A, et al. The morbidity and mortality of hepaticojejunostomies for complex bile duct injuries: A multi-institutional analysis of risk factors and outcomes using NSQIP[J]. HPB (Oxford), 2017, 19(4): 352-358. DOI: 10.1016/j.hpb.2016.12.004. [2] HALBERT C, PAGKRATIS S, YANG J, et al. Beyond the learning curve: Incidence of bile duct injuries following laparoscopic cholecystectomy normalize to open in the modern era[J]. Surg Endosc, 2016, 30(6): 2239-2243. DOI: 10.1007/s00464-015-4485-2. [3] FONG ZV, PITT HA, STRASBERG SM, et al. Diminished survival in patients with bile leak and ductal injury: Management strategy and outcomes[J]. J Am Coll Surg, 2018, 226(4): 568-576. e1. DOI: 10.1016/j.jamcollsurg.2017.12.023. [4] BARRETT M, ASBUN HJ, CHIEN HL, et al. Bile duct injury and morbidity following cholecystectomy: A need for improvement[J]. Surg Endosc, 2018, 32(4): 1683-1688. DOI: 10.1007/s00464-017-5847-8. [5] MURRAY AC, MARKAR S, MACKENZIE H, et al. An observational study of the timing of surgery, use of laparoscopy and outcomes for acute cholecystitis in the USA and UK[J]. Surg Endosc, 2018, 32(7): 3055-3063. DOI: 10.1007/s00464-017-6016-9. [6] KIM SS, DONAHUE TR. Laparoscopic cholecystectomy[J]. JAMA, 2018, 319(17): 1834. DOI: 10.1001/jama.2018.3438. [7] TÖRNQVIST B, STRÖMBERG C, AKRE O, et al. Selective intraoperative cholangiography and risk of bile duct injury during cholecystectomy[J]. Br J Surg, 2015, 102(8): 952-958. DOI: 10.1002/bjs.9832. [8] MARTINEZ-LOPEZ S, UPASANI V, PANDANABOYANA S, et al. Delayed referral to specialist centre increases morbidity in patients with bile duct injury (BDI) after laparoscopic cholecystectomy (LC)[J]. Int J Surg, 2017, 44: 82-86. DOI: 10.1016/j.ijsu.2017.06.042. [9] AYLOO S, SCHWARTZMAN J. Robot-assisted repair of e1 biliary ductal injury with Roux-en-Y hepaticojejunostomy[J]. J Laparoendosc Adv Surg Tech A, 2019, 29(6): 817-819. DOI: 10.1089/lap.2018.0664. [10] BOOIJ K, de REUVER PR, van DIEREN S, et al. Long-term impact of bile duct injury on morbidity, mortality, quality of life, and work related limitations[J]. Ann Surg, 2018, 268(1): 143-150. DOI: 10.1097/SLA.0000000000002258. [11] DOMINGUEZ-ROSADO I, SANFORD DE, LIU J, et al. Timing of surgical repair after bile duct injury impacts postoperative complications but not anastomotic patency[J]. Ann Surg, 2016, 264(3): 544-553. DOI: 10.1097/SLA.0000000000001868. [12] GIULIANOTTI PC, QUADRI P, DURGAM S, et al. Reconstruction/repair of iatrogenic biliary injuries: Is the robot offering a new option? Short clinical report[J]. Ann Surg, 2018, 267(1): e7-e9. DOI: 10.1097/SLA.0000000000002343. [13] WYSOCKI AP. Population-based studies should not be used to justify a policy of routine cholangiography to prevent major bile duct injury during laparoscopic cholecystectomy[J]. World J Surg, 2017, 41(1): 82-89. DOI: 10.1007/s00268-016-3665-0. [14] JIN H, DONG Q, HE Z, et al. Research on indocyanine green angiography for predicting postoperative hypoparathyroidism[J]. Clin Endocrinol (Oxf), 2019, 90(3): 487-493. DOI: 10.1111/cen.13925. [15] JIN H, CUI M. New advances of ICG angiography in parathyroid identification[J]. Endocr Metab Immune Disord Drug Targets, 2019, 19(7): 936-940. DOI: 10.2174/1871530319666190206212456. [16] PERRY D, BHARARA M, ARMSTRONG DG, et al. Intraoperative fluorescence vascular angiography: During tibial bypass[J]. J Diabetes Sci Technol, 2012, 6(1): 204-208. DOI: 10.1177/193229681200600125. [17] KAWADA K, HASEGAWA S, WADA T, et al. Evaluation of intestinal perfusion by ICG fluorescence imaging in laparoscopic colorectal surgery with DST anastomosis[J]. Surg Endosc, 2017, 31(3): 1061-1069. DOI: 10.1007/s00464-016-5064-x. [18] ISHIZAWA T, BANDAI Y, IJICHI M, et al. Fluorescent cholangiography illuminating the biliary tree during laparoscopic cholecystectomy[J]. Br J Surg, 2010, 97(9): 1369-1377. DOI: 10.1002/bjs.7125. [19] LIU YY, LIAO CH, DIANA M, et al. Near-infrared cholecystocholangiography with direct intragallbladder indocyanine green injection: Preliminary clinical results[J]. Surg Endosc, 2018, 32(3): 1506-1514. DOI: 10.1007/s00464-017-5838-9. 期刊类型引用(12)
1. 徐元,章波. 吲哚青绿近红外荧光胆道造影指导腹腔镜胆囊切除术治疗胆囊结石患者疗效研究. 实用肝脏病杂志. 2024(01): 141-144 .  百度学术
百度学术2. 杨铁健,李文奇,张开明,张俊杰. 吲哚菁绿荧光成像技术指导难治性胆囊切除术的前瞻性研究. 肝胆外科杂志. 2024(01): 35-39 .  百度学术
百度学术3. 李昌旭,李学民,梁占强,段希斌,杨鹏生. 吲哚菁绿荧光导航在老年急性胆囊炎患者经皮经肝胆囊穿刺引流术后腹腔镜胆囊切除术中的应用. 临床肝胆病杂志. 2023(04): 885-891 .  本站查看
本站查看4. 陈镜宇,李达,徐鹏,林家嘉,佟德明,石三宝,张成. 小野寺预后营养指数对腹腔镜下直肠癌根治术后并发症预测价值研究. 临床军医杂志. 2023(04): 357-361 .  百度学术
百度学术5. 姬文超,韩瑞,牛莉莉,程少华. 吲哚菁绿荧光成像技术在腹腔镜胆囊切除术中的应用效果. 中国医学创新. 2023(16): 163-166 .  百度学术
百度学术6. 施舒鹏,常久翔,曾陶飞,何浩,尹大龙. 基于Cite Space文献计量法肝癌微创治疗的可视化分析. 中华消化外科杂志. 2023(09): 1139-1146 .  百度学术
百度学术7. 汪鑫,杨云,汪越,詹锐,张晓琴,崔巍. 不同方式给予右美托咪定在腹腔镜胆囊切除术应用效果比较. 临床军医杂志. 2023(12): 1258-1260 .  百度学术
百度学术8. 陆乔友,寸冬云,虞弘,郭鹏恒,田大广. ICG荧光胆道造影在胆囊结石合并胆囊炎患者LC术中的应用. 中华肝脏外科手术学电子杂志. 2023(03): 284-288 .  百度学术
百度学术9. 张建康,李涛,秦锡虎,吴宝强. 吲哚菁绿荧光胆道成像技术辅助腹腔镜残余胆囊结石切除:1例报道. 手术电子杂志. 2023(06): 76-77 .  百度学术
百度学术10. 舒杰,张昊翔,李建伟,李林,常清春,索朗旦增,曾继峰,郑芳芳,曹利,郑树国. 西藏高海拔地区急性结石性胆囊炎的临床特征及手术疗效分析. 中华消化外科杂志. 2022(07): 917-922 .  百度学术
百度学术11. 李敬东,黄徐建. 腹腔镜肝切除术中医源性胆道损伤的病因及防治策略. 中华肝脏外科手术学电子杂志. 2022(04): 335-337 .  百度学术
百度学术12. 王超群,宋清怡,姜启哲,崔云凡,殷保兵. ICG荧光显像技术引导下精准肝肿瘤切除术的现状与未来. 中华肝脏外科手术学电子杂志. 2022(04): 342-346 .  百度学术
百度学术其他类型引用(5)
-




 PDF下载 ( 2140 KB)
PDF下载 ( 2140 KB)


 下载:
下载:
 下载:
下载:
 百度学术
百度学术