不同Child-Pugh分级肝硬化患者糖化白蛋白的测定及其应用价值
DOI: 10.3969/j.issn.1001-5256.2022.02.018
Measurement of glycosylated albumin and its application value in liver cirrhosis patients with different Child-Pugh classes
-
摘要:
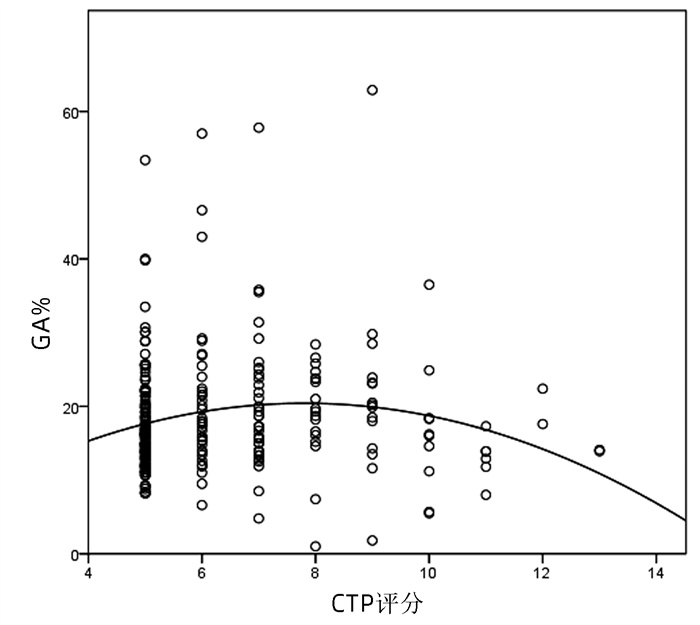
目的 探讨不同Child-Pugh分级肝硬化患者糖化白蛋白(GA)水平及其在预测肝功能方面的应用价值。 方法 纳入2019年1月1日—12月31日于天津市第三中心医院住院治疗的肝硬化患者486例,其中肝硬化未合并糖尿病患者227例,肝硬化合并糖尿病患者259例。按照Child-Turcotte-Pugh(CTP)评分进行分组,测定空腹血糖、糖化血红蛋白、糖化白蛋白百分比(GA%)。非正态分布的计量资料3组间比较采用Kruskal-Wallis H检验,进一步两两比较采用Dwass-Steel-Critchlow-Fligner检验。绘制CTP评分与GA%之间的散点图和拟合曲线,评估二者的关系,并计算cut-off值。 结果 肝硬化未合并糖尿病患者不同Child-Pugh分级之间GA%(χ2=24.809,P<0.001)、空腹血糖(χ2=11.899,P=0.003)、糖化血红蛋白(χ2=13.607,P=0.001)比较差异均有统计学意义,进一步两两比较显示,Child-Pugh A级、B级肝硬化未合并糖尿病患者与C级相比,GA%差异均有统计学意义(P值均<0.05);Child-Pugh A级患者空腹血糖水平明显高于Child-Pugh B级患者(P<0.05);Child-Pugh A级患者糖化血红蛋白水平明显高于Child-Pugh B级和C级患者(P值均<0.05)。肝硬化合并糖尿病患者不同Child-Pugh分级之间GA%(χ2=10.734,P=0.005)、空腹血糖(χ2=16.295,P<0.001)比较差异均有统计学意义,进一步两两比较显示,Child-Pugh C级肝硬化合并糖尿病患者GA%明显低于A级和B级(P值均<0.05);Child-Pugh A级患者空腹血糖水平低于B级患者(P<0.05)。拟合曲线结果显示,肝硬化未合并糖尿病患者随着CTP评分升高,GA%升高,在评分为6.5分时GA%最高,然后开始下降,评分为11.5分时GA%最低,呈曲线关系;肝硬化合并糖尿病患者的GA%随CTP评分增加呈现先升高后降低曲线,cut-off值为8分。 结论 随着肝硬化病情进展,GA%出现先升高后降低的变化。不同Child-Pugh分级肝硬化患者GA水平差异明显,提示GA的降低与终末期肝硬化肝功能失代偿密切相关。 Abstract:Objective To investigate the level of glycosylated albumin (GA) in liver cirrhosis patients with different Child-Pugh classes and its application value in predicting liver function. Methods A total of 486 patients with liver cirrhosis who were hospitalized in Tianjin Third Central Hospital from January 1 to December 31, 2019, were enrolled, among whom 227 patients had liver cirrhosis without diabetes and 259 patients had liver cirrhosis with diabetes. The patients were divided into groups according to Child-Turcotte-Pugh (CTP) score, and fasting blood glucose, glycosylated hemoglobin, and percentage of GA (GA%) were measured. The Kruskal-Wallis H test was used for comparison of non-normally distributed continuous data between three groups, and the Dwass-Steel-Critchlow-Fligner test was used for further comparison between two groups. Scatter plots and fitting curves were plotted for CTP score and GA% to evaluate the association between them and calculate the cut-off value. Results For the cirrhosis patients without diabetes, there were significant differences between the patients with different Child-Pugh classes in GA% (χ2=24.809, P< 0.001), fasting blood glucose (χ2=11.899, P=0.003), and glycosylated hemoglobin (χ2=13.607, P=0.001); further pairwise comparison showed that there was a significant difference in GA% between Child-Pugh class A/B liver cirrhosis patients without diabetes and Child-Pugh class C liver cirrhosis patients (P < 0.05), Child-Pugh class A patients had a significantly higher level of fasting blood glucose than Child-Pugh class B patients (P < 0.05), and Child-Pugh class A patients had a significantly higher level of glycosylated hemoglobin than Child-Pugh class B/C patients (P < 0.05). For the patients with liver cirrhosis and diabetes, there were significant differences between the patients with different Child-Pugh classes in GA% (χ2=10.734, P=0.005) and fasting blood glucose (χ2=16.295, P < 0.001); further pairwise comparison showed that Child-Pugh class C liver cirrhosis patients with diabetes had a significantly lower GA% than Child-Pugh class A/B patients (P < 0.05) and Child-Pugh class A patients had a significantly lower fasting blood glucose level than Child-Pugh class B patients (P < 0.05). The fitting curve showed that GA% increased with the increase in CTP score in the liver cirrhosis patients without diabetes, reached the highest value at the CTP score of 6.5, and then started to decrease, with the lower value at the CTP score of 11.5, which showed a curvilinear relationship; in the liver cirrhosis patients with diabetes, GA% first increased and then decreased with the increase in CTP score, with a cut-off value of 8. Conclusion GA% first increases and then decreases along with the progression of liver cirrhosis. There is a significant difference in GA between liver cirrhosis patients with different Child-Pugh classes, suggesting that the reduction in GA is closely associated with liver function decompensation in end-stage liver cirrhosis. -
Key words:
- Liver Cirrhosis /
- Glycosylated Albumin /
- Diagnosis
-
表 1 纳入患者一般资料
指标 肝硬化未合并糖尿病组(n=227) 肝硬化合并糖尿病组(n=259) 男/女(例) 145/82 168/91 年龄(岁) 60(53~67) 62(55~68) 肝硬化病因[例(%)] 丙型肝炎肝硬化 24(10.6) 30(11.6) 酒精性肝硬化 31(13.7) 62(23.9) 乙型肝炎肝硬化 123(54.2) 107(41.3) 自身免疫性肝硬化 49(21.6) 60(23.2) Child-Pugh分级[例(%)] A级 167(73.6) 168(64.9) B级 43(18.9) 71(27.4) C级 17(7.5) 20(7.7) 表 2 肝硬化未合并糖尿病患者不同Child-Pugh分级GA%、血糖、糖化血红蛋白比较
指标 Child-Pugh分级 χ2值 P值 A级(n=167) B级(n=43) C级(n=17) GA% 12.9(11.2~15.4) 14.8(11.0~17.4) 5.2(4.2~11.4)1)2) 24.809 <0.001 血糖(mmol/L) 5.2(4.9~5.6) 5.0(4.5~5.4)1) 4.8(4.3~5.4) 11.899 0.003 糖化血红蛋白(%) 5.3(5.0~5.6) 5.0(4.5~5.3)1) 4.9(4.0~5.4)1) 13.607 0.001 注:与Child-Pugh A级比较,1)P<0.05;与Child-Pugh B级比较,2)P<0.05。 表 3 肝硬化合并糖尿病患者不同CTP分级GA%、血糖、糖化血红蛋白的比较
指标 Child-Pugh分级 χ2值 P值 A级(n=168) B级(n=71) C级(n=20) GA% 17.3(13.4~21.1) 19.3(15.0~23.8) 14.4(12.4~18.0)1)2) 10.734 0.005 血糖(mmol/L) 7.2(6.5~8.8) 8.3(7.0~10.3)1) 8.2(6.5~9.8) 16.295 <0.001 糖化血红蛋白(%) 6.0(5.5~6.8) 5.6(5.0~7.3) 5.4(4.8~6.4) 6.567 0.058 注:与Child-Pugh A级比较,1)P<0.05;与Child-Pugh B级比较,2)P<0.05。 -
[1] WU MC, MENG QH. Nutritional assessment and clinical management of patients with acute-on-chronic liver failure[J]. J Clin Hepatol, 2021, 37(4): 770-774. DOI: 10.3969/j.issn.1001-5256.2021.04.006.吴牧晨, 孟庆华. 慢加急性肝衰竭患者的营养评估及临床管理[J]. 临床肝胆病杂志, 2021, 37(4): 770-774. DOI: 10.3969/j.issn.1001-5256.2021.04.006. [2] BAR-DAYAN Y, WAINSTEIN J, SCHORR L, et al. Hypoglycemia- simplifying the ways to predict an old problem in the general ward[J]. Eur J Intern Med, 2019, 60: 13-17. DOI: 10.1016/j.ejim.2018.10.007. [3] LEE WG, WELLS CI, MCCALL JL, et al. Prevalence of diabetes in liver cirrhosis: A systematic review and meta-analysis[J]. Diabetes Metab Res Rev, 2019, 35(6): e3157. DOI: 10.1002/dmrr.3157. [4] DOZIO E, DI GAETANO N, FINDEISEN P, et al. Glycated albumin: From biochemistry and laboratory medicine to clinical practice[J]. Endocrine, 2017, 55(3): 682-690. DOI: 10.1007/s12020-016-1091-6. [5] KOUZUMA T, UEMASTU Y, USAMI T, et al. Study of glycated amino acid elimination reaction for an improved enzymatic glycated albumin measurement method[J]. Clin Chim Acta, 2004, 346(2): 135-143. DOI: 10.1016/j.cccn.2004.02.019. [6] LIN XF, WANG HN, HONG TP. The clinical application of glycated albumin[J]. Chin J Diabetes, 2020, 28(1): 77-80. DOI: 10.3969/j.issn.1006-6187.2020.01.016.林夏舫, 王海宁, 洪天配. 糖化白蛋白的临床应用价值[J]. 中国糖尿病杂志, 2020, 28(1): 77-80. DOI: 10.3969/j.issn.1006-6187.2020.01.016. [7] ZUO H, WANG SJ, FENG J, et al. The relationship between serum total bilirubin, glycated albumin, glycated hemoglobin and diabetic vascular complications[J]. Chin J Arteriosclerosis, 2019, 27(9): 787-790. https://www.cnki.com.cn/Article/CJFDTOTAL-KDYZ201909011.htm左红, 王述进, 冯佳, 等. 血清总胆红素、糖化白蛋白、糖化血红蛋白与糖尿病血管并发症的关系[J]. 中国动脉硬化杂志, 2019, 27(9): 787-790. https://www.cnki.com.cn/Article/CJFDTOTAL-KDYZ201909011.htm [8] UEDA Y, MATSUMOTO H. Recent topics in chemical and clinical research on glycated albumin[J]. J Diabetes Sci Technol, 2015, 9(2): 177-182. DOI: 10.1177/1932296814567225. [9] GUNDLING F, SEIDL H, STRASSEN I, et al. Clinical manifestations and treatment options in patients with cirrhosis and diabetes mellitus[J]. Digestion, 2013, 87(2): 75-84. DOI: 10.1159/000343458. [10] KONISHI I, HIASA Y, SHIGEMATSU S, et al. Diabetes pattern on the 75 g oral glucose tolerance test is a risk factor for hepatocellular carcinoma in patients with hepatitis C virus[J]. Liver Int, 2009, 29(8): 1194-1201. DOI: 10.1111/j.1478-3231.2009.02043.x. [11] Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006.中华医学会肝病学分会. 肝硬化诊治指南[J]. 临床肝胆病杂志, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. [12] Chinese Diabetes Society. Guidelines for the prevention and control of type 2 diabetes in China (2017 Edition)[J]. Chin J Pract Intern Med, 2018, 38(4): 292-344. DOI: 10.19538/j.nk2018040108.中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2017年版)[J]. 中国实用内科杂志, 2018, 38(4): 292-344. DOI: 10.19538/j.nk2018040108. [13] LI DZ, LI J, GUO XL. Value of albumin-bilirubin score in predicting the prognosis of patients with liver cirrhosis and esophagogastric variceal bleeding[J]. J Clin Hepatol, 2021, 37(5): 1085-1090. DOI: 10.3969/j.issn.1001-5256.2021.05.022.李德钊, 李健, 郭晓林. 白蛋白-胆红素评分对肝硬化食管胃静脉曲张出血患者预后的预测价值[J]. 临床肝胆病杂志, 2021, 37(5): 1085-1090. DOI: 10.3969/j.issn.1001-5256.2021.05.022. [14] KOGA M, KASAYAMA S. Clinical impact of glycated albumin as another glycemic control marker[J]. Endocr J, 2010, 57(9): 751-762. DOI: 10.1507/endocrj.k10e-138. [15] ATCHISON EA, GRIDLEY G, CARREON JD, et al. Risk of cancer in a large cohort of U.S. veterans with diabetes[J]. Int J Cancer, 2011, 128(3): 635-643. DOI: 10.1002/ijc.25362. [16] NIE LF, SHU JC, ZHANG WR, et al. Variation tendency of the level of fasting plasma glucose in patients with decompensated liver cirrhosis[J]. Chin J Gastroenterol Hepatol, 2014, 23(7): 813-815. DOI: 10.3969/j.issn.1006-5709.2014.07.026.聂丽芬, 舒建昌, 张文茹, 等. 肝硬化失代偿期空腹血糖变化观察[J]. 胃肠病学和肝病学杂志, 2014, 23(7): 813-815. DOI: 10.3969/j.issn.1006-5709.2014.07.026. [17] PETERSEN KF, KRSSAK M, NAVARRO V, et al. Contributions of net hepatic glycogenolysis and gluconeogenesis to glucose production in cirrhosis[J]. Am J Physiol, 1999, 276(3): e529-e535. DOI: 10.1152/ajpendo.1999.276.3.E529. [18] KRÄHENBVHL L, LANG C, LVDES S, et al. Reduced hepatic glycogen stores in patients with liver cirrhosis[J]. Liver Int, 2003, 23(2): 101-109. DOI: 10.1034/j.1600-0676.2003.00805.x. [19] LIU P. Detection of glycated albumin in patients with type 2 diabetes and diabetes complicated with cirrhosis and clinical significance[J]. J Medical Forum, 2016, 37(2): 41-42.刘沛. 2型糖尿病和糖尿病并发肝硬化患者糖化白蛋白水平的检测及其意义[J]. 医药论坛杂志, 2016, 37(2): 41-42. [20] JIANG XJ, SUN XS, HUANG YQ, et al. The clinical significance of glycated albumin for patients with liver cirrhosis[J]. Lab Med, 2012, 27(11): 948-950.江筱炯, 孙先胜, 黄亦青, 等. 糖化白蛋白在肝硬化患者中的临床意义[J]. 检验医学杂志, 2012, 27(11): 948-950. -



 PDF下载 ( 2048 KB)
PDF下载 ( 2048 KB)


 下载:
下载: