肝脏驻留自然杀伤细胞在肝细胞癌发生发展中的作用
DOI: 10.3969/j.issn.1001-5256.2022.02.041
利益冲突声明:所有作者均声明不存在利益冲突。
作者贡献声明:王俊旗、徐锋负责课题设计,收集数据,资料分析,撰写论文并最后定稿。
Role of liver-resident natural killer cells in the development and progression of hepatocellular carcinoma
-
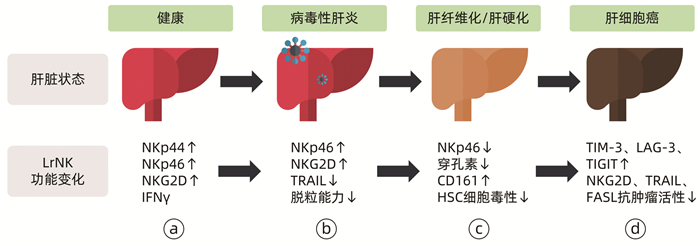
摘要: 肝脏驻留自然杀伤(LrNK)细胞作为新近发现的组织驻留性自然杀伤细胞,具有较强的免疫杀伤功能。在肝细胞癌(HCC)的发生发展过程中,LrNK细胞功能受损,且可能通过上调相关免疫检查点的表达促进HCC进展。基于最新的相关研究,综述了LrNK细胞的免疫功能及其在HCC发生发展过程中的作用,以期探究该细胞在HCC免疫治疗中的应用前景。Abstract: Liver-resident natural killer (LrNK) cells, as a type of newly discovered tissue-resident natural killer cells, have a strong immune killing function. During the development and progression of hepatocellular carcinoma (HCC), the function of LrNK cells is impaired and such cells may promote the progression of HCC by upregulating the expression of related immune checkpoints. Based on the latest research, this article reviews the immune function of LrNK cells and their role in the development and progression of HCC, in order to explore the application prospect of these cells in HCC immunotherapy.
-
Key words:
- Carcinoma, Hepatocellular /
- Killer Cells, Natural /
- Immunotherapy
-
[1] SUNG H, FERLAY J, SIEGEL RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. DOI: 10.3322/caac.21660. [2] KOLE C, CHARALAMPAKIS N, TSAKATIKAS S, et al. Immunotherapy for hepatocellular carcinoma: A 2021 update[J]. Cancers (Basel), 2020, 12(10): 2859. DOI: 10.3390/cancers12102859. [3] FU YZ, XU L. Advances in multimodality therapy for hepatocellular carcinoma[J]. J Clin Hepatol, 2020, 36(10): 2179-2183. DOI: 10.3969/j.issn.1001-5256.2020.10.004.傅毅振, 徐立. 肝细胞癌综合治疗进展[J]. 临床肝胆病杂志, 2020, 36(10): 2179-2183. DOI: 10.3969/j.issn.1001-5256.2020.10.004. [4] RUF B, HEINRICH B, GRETEN TF. Immunobiology and immunotherapy of HCC: Spotlight on innate and innate-like immune cells[J]. Cell Mol Immunol, 2021, 18(1): 112-127. DOI: 10.1038/s41423-020-00572-w. [5] HUDSPETH K, DONADON M, CIMINO M, et al. Human liver-resident CD56(bright)/CD16(neg) NK cells are retained within hepatic sinusoids via the engagement of CCR5 and CXCR6 pathways[J]. J Autoimmun, 2016, 66: 40-50. DOI: 10.1016/j.jaut.2015.08.011. [6] SIVORI S, PENDE D, QUATRINI L, et al. NK cells and ILCs in tumor immunotherapy[J]. Mol Aspects Med, 2021, 80: 100870. DOI: 10.1016/j.mam.2020.100870. [7] PENG H, SUN R. Liver-resident NK cells and their potential functions[J]. Cell Mol Immunol, 2017, 14(11): 890-894. DOI: 10.1038/cmi.2017.72. [8] PENG H, TIAN ZG. Liver-specific natural killer cells: Discovery, validation, and functions[J]. Scientia Sinica(Vitae), 2017, 47(1): 43-51. DOI: 10.1360/n052016-00337.彭慧, 田志刚. 肝脏特有NK细胞的发现、验证与功能[J]. 中国科学: 生命科学, 2017, 47(1): 43-51. DOI: 10.1360/n052016-00337. [9] LUO DZ, VERMIJLEN D, AHISHALI B, et al. On the cell biology of pit cells, the liver-specific NK cells[J]. World J Gastroenterol, 2000, 6(1): 1-11. DOI: 10.3748/wjg.v6.i1.1. [10] PENG H, JIANG X, CHEN Y, et al. Liver-resident NK cells confer adaptive immunity in skin-contact inflammation[J]. J Clin Invest, 2013, 123(4): 1444-1456. DOI: 10.1172/JCI66381. [11] LI JR, TIAN ZG, PENG H. Development and ontogeny of liver-resident NK cells[J]. Chin J Immunol, 2020, 36(8): 897-904. DOI: 10.3969/j.issn.1000-484X.2020.08.001.李佳瑞, 田志刚, 彭慧. 肝脏驻留NK细胞的发育分化及其个体发生[J]. 中国免疫学杂志, 2020, 36(8): 897-904. DOI: 10.3969/j.issn.1000-484X.2020.08.001. [12] HYDES T, ABUHILAL M, ARMSTRONG T, et al. Natural killer cell maturation markers in the human liver and expansion of an NKG2C+KIR+ population[J]. Lancet, 2015, 385 (Suppl 1): S45. DOI: 10.1016/S0140-6736(15)60360-9. [13] HARMON C, ROBINSON MW, FAHEY R, et al. Tissue-resident Eomes(hi) T-bet(lo) CD56(bright) NK cells with reduced proinflammatory potential are enriched in the adult human liver[J]. Eur J Immunol, 2016, 46(9): 2111-2120. DOI: 10.1002/eji.201646559. [14] MALE V. Liver-resident NK cells: The human factor[J]. Trends Immunol, 2017, 38(5): 307-309. DOI: 10.1016/j.it.2017.02.008. [15] WANG X, TIAN Z, PENG H. Tissue-resident memory-like ILCs: Innate counterparts of T(RM) cells[J]. Protein Cell, 2020, 11(2): 85-96. DOI: 10.1007/s13238-019-0647-7. [16] WANG XW, TIAN ZG. Immunological memory of innate lymphoid cells[J]. Chin J Immunol, 2019, 35(7): 769-775. DOI: 10.3969/j.issn.1000-484X.2019.07.001.王宪伟, 田志刚. 记忆性ILCs研究进展[J]. 中国免疫学杂志, 2019, 35(7): 769-775. DOI: 10.3969/j.issn.1000-484X.2019.07.001. [17] ZHANG LH, SHIN JH, HAGGADONE MD, et al. The aryl hydrocarbon receptor is required for the maintenance of liver-resident natural killer cells[J]. J Exp Med, 2016, 213(11): 2249-2257. DOI: 10.1084/jem.20151998. [18] MARQUARDT N, BÉZIAT V, NYSTRÖM S, et al. Cutting edge: Identification and characterization of human intrahepatic CD49a+ NK cells[J]. J Immunol, 2015, 194(6): 2467-2471. DOI: 10.4049/jimmunol.1402756. [19] BAI L, PENG H, HAO X, et al. CD8(+) T cells promote maturation of liver-resident NK cells through the CD70-CD27 axis[J]. Hepatology, 2019, 70(5): 1804-1815. DOI: 10.1002/hep.30757. [20] ZHOU J, PENG H, LI K, et al. Liver-resident NK cells control antiviral activity of hepatic T cells via the PD-1-PD-L1 axis[J]. Immunity, 2019, 50(2): 403-417. e4. DOI: 10.1016/j.immuni.2018.12.024. [21] BAI L. The effect of liver microenvironment on development of liver resident NK cells[D]. Hefei: University of Science and Technology of China, 2018.白璐. 肝脏微环境对肝脏驻留NK细胞发育的调控[D]. 合肥: 中国科学技术大学, 2018. [22] ZHAO ZB, LU FT, MA HD, et al. Liver-resident NK cells suppress autoimmune cholangitis and limit the proliferation of CD4(+) T cells[J]. Cell Mol Immunol, 2020, 17(2): 178-189. DOI: 10.1038/s41423-019-0199-z. [23] CHENG M, SUN R, TIAN ZG, et al. Human liver NK cells and liver diseases[J]. Chin J Immunol, 2020, 36(11): 1281-1290. DOI: 10.3969/j.issn.1000-484X.2020.11.001.程明, 孙汭, 田志刚, 等. 人类肝脏NK细胞与肝脏疾病[J]. 中国免疫学杂志, 2020, 36(11): 1281-1290. DOI: 10.3969/j.issn.1000-484X.2020.11.001. [24] KALATHIL SG, THANAVALA Y. Natural killer cells and T cells in hepatocellular carcinoma and viral hepatitis: Current status and perspectives for future immunotherapeutic approaches[J]. Cells, 2021, 10(6): 1332. DOI: 10.3390/cells10061332. [25] ZHENG M, SUN R, WEI H, et al. NK cells help induce anti-hepatitis B virus CD8+ T cell immunity in mice[J]. J Immunol, 2016, 196(10): 4122-4131. DOI: 10.4049/jimmunol.1500846. [26] DONG S, GENG L, SHEN MD, et al. Natural killer cell activating receptor NKG2D is involved in the immunosuppressive effects of mycophenolate mofetil and hepatitis B virus infection[J]. Am J Med Sci, 2015, 349(5): 432-437. DOI: 10.1097/MAJ.0000000000000442. [27] VARCHETTA S, MELE D, MANTOVANI S, et al. Impaired intrahepatic natural killer cell cytotoxic function in chronic hepatitis C virus infection[J]. Hepatology, 2012, 56(3): 841-849. DOI: 10.1002/hep.25723. [28] LIU M, HU Y, YUAN Y, et al. γδT cells suppress liver fibrosis via strong cytolysis and enhanced NK cell-mediated cytotoxicity against hepatic stellate cells[J]. Front Immunol, 2019, 10: 477. DOI: 10.3389/fimmu.2019.00477. [29] FASBENDER F, WIDERA A, HENGSTLER JG, et al. Natural killer cells and liver fibrosis[J]. Front Immunol, 2016, 7: 19. DOI: 10.3389/fimmu.2016.00019. [30] LI X, ZHANG M, LIU J, et al. Intrahepatic NK cells function suppressed in advanced liver fibrosis[J]. Eur J Clin Invest, 2016, 46(10): 864-872. DOI: 10.1111/eci.12669. [31] JAMESON G, ROBINSON MW. Insights into human intrahepatic NK cell function from single cell RNA sequencing datasets[J]. Front Immunol, 2021, 12: 649311. DOI: 10.3389/fimmu.2021.649311. [32] DODARD G, TATA A, ERICK TK, et al. Inflammation-induced lactate leads to rapid loss of hepatic tissue-resident NK cells[J]. Cell Rep, 2020, 32(1): 107855. DOI: 10.1016/j.celrep.2020.107855. [33] SUN H, LIU L, HUANG Q, et al. Accumulation of tumor-infiltrating CD49a(+) NK cells correlates with poor prognosis for human hepatocellular carcinoma[J]. Cancer Immunol Res, 2019, 7(9): 1535-1546. DOI: 10.1158/2326-6066.CIR-18-0757. [34] HWANG S, HAN J, BAEK JS, et al. Cytotoxicity of human hepatic intrasinusoidal CD56(bright) natural killer cells against hepatocellular carcinoma cells[J]. Int J Mol Sci, 2019, 20(7): 1564. DOI: 10.3390/ijms20071564. [35] SUN C, SUN HY, XIAO WH, et al. Natural killer cell dysfunction in hepatocellular carcinoma and NK cell-based immunotherapy[J]. Acta Pharmacol Sin, 2015, 36(10): 1191-1199. DOI: 10.1038/aps.2015.41. [36] PIÑEIRO FERNÁNDEZ J, LUDDY KA, HARMON C, et al. Hepatic tumor microenvironments and effects on NK cell phenotype and function[J]. Int J Mol Sci, 2019, 20(17): 4131. DOI: 10.3390/ijms20174131. [37] SHEN X, LI N, LI H, et al. Increased prevalence of regulatory T cells in the tumor microenvironment and its correlation with TNM stage of hepatocellular carcinoma[J]. J Cancer Res Clin Oncol, 2010, 136(11): 1745-1754. DOI: 10.1007/s00432-010-0833-8. [38] PINATO DJ, GUERRA N, FESSAS P, et al. Immune-based therapies for hepatocellular carcinoma[J]. Oncogene, 2020, 39(18): 3620-3637. DOI: 10.1038/s41388-020-1249-9. [39] TAN S, XU Y, WANG Z, et al. Tim-3 hampers tumor surveillance of liver-resident and conventional NK cells by disrupting PI3K signaling[J]. Cancer Res, 2020, 80(5): 1130-1142. DOI: 10.1158/0008-5472.CAN-19-2332. [40] AW YEANG HX, PIERSMA SJ, LIN Y, et al. Cutting edge: Human CD49e- NK cells are tissue resident in the liver[J]. J Immunol, 2017, 198(4): 1417-1422. DOI: 10.4049/jimmunol.1601818. [41] WANG Y, ZHANG C. The roles of liver-resident lymphocytes in liver diseases[J]. Front Immunol, 2019, 10: 1582. DOI: 10.3389/fimmu.2019.01582. -



 PDF下载 ( 2117 KB)
PDF下载 ( 2117 KB)

 下载:
下载:


