国际标准化比值/血小板比值指数对原发性胆汁性胆管炎相关肝纤维化的诊断价值
DOI: 10.3969/j.issn.1001-5256.2022.03.012
Value of international normalized ratio-to-platelet ratio in the diagnosis of liver fibrosis in patients with primary biliary cholangitis
-
摘要:
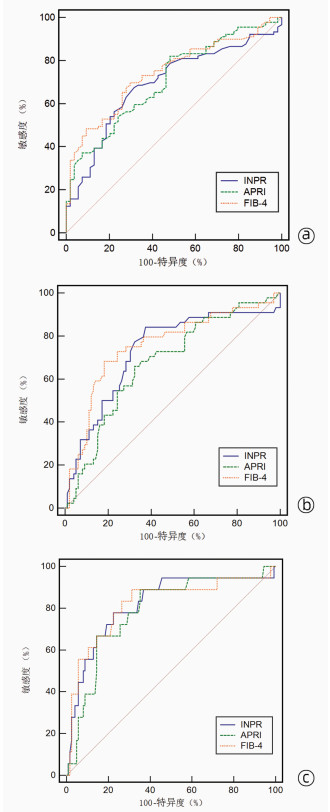
目的 探究国际标准化比值/PLT比值指数(INPR)对原发性胆汁性胆管炎(PBC)患者肝纤维化程度的诊断价值,并与AST/PLT比值指数(ARRI)和肝纤维化4因子指数(FIB- 4)进行比较。 方法 回顾性纳入2013年10月—2021年3月在郑州大学第一附属医院行肝穿刺活检明确诊断为PBC的患者。采用Scheuer评分系统评估肝纤维化程度,分为S0~S4期。根据肝穿刺病理结果将患者的肝纤维化程度分为显著肝纤维化(≥S2)、进展期肝纤维化(≥S3)和肝硬化(S4)。收集患者一般资料、肝功能、血常规、血凝等指标,利用公式计算血清学无创模型INPR、APRI及FIB-4。计量资料多组间比较采用Kruskal-Wallis H秩和检验;计数资料多组间比较采用χ2检验。采用Spearman相关分析评估无创模型与肝纤维化分期的相关性,应用受试者工作特征曲线(ROC曲线)评估血清学无创模型对肝纤维化程度的诊断效能,ROC曲线下面积(AUC)的比较采用DeLong法。 结果 共纳入143例PBC患者,其中肝纤维化S0、S1、S2、S3和S4期分别为4、50、46、26和17例。INPR评分在不同肝纤维化程度PBC患者间差异显著(χ2=27.347,P<0.001)。随着肝纤维化程度加重,INPR评分逐渐升高,INPR与肝纤维化程度呈正相关(r=0.419,P<0.01)。ROC曲线分析显示,INPR、APRI、FIB-4用于诊断PBC显著肝纤维化(≥S2)的AUC分别为0.691、0.706、0.742,对应的cut-off值分别为0.63、0.59、2.68。INPR、APRI、FIB-4用于诊断PBC进展期肝纤维化(≥S3)的AUC分别为0.731、0.675、0.756,对应的cut-off值分别为0.64、1.23、4.63。INPR、APRI、FIB-4用于诊断PBC肝硬化(S4)的AUC分别为0.820、0.786、0.818,对应的cut-off值分别为0.95、1.26、4.63。在评估显著肝纤维化、进展期肝纤维化和肝硬化方面,INPR的AUC与APRI和FIB-4比较,差异均无统计学意义(P值均>0.05)。 结论 INPR是一种简单、准确的肝纤维化无创评估模型,对PBC肝纤维化有一定的诊断价值。 Abstract:Objective To investigate the value of international standardized ratio-to-platelet ratio (INPR) versus aspartate aminotransferase-to-platelet ratio index (APRI) and fibrosis-4 (FIB-4) in the diagnosis of liver fibrosis in patients with primary cholangitis (PBC). Methods A retrospective analysis was performed for the patients who underwent liver biopsy and were diagnosed with PBC in The First Affiliated Hospital of Zhengzhou University from October 2013 to March 2021. Scheuer score was used to systematically evaluate the degree of liver fibrosis (S0-S4 stage). According to the results of liver biopsy, the degree of liver fibrosis was classified as significant liver fibrosis (≥S2), progressive liver fibrosis (≥S3), and liver cirrhosis (S4). Related data including general information, liver function, routine blood test results, and blood coagulation were collected, and related formulas were used to calculate the values of the noninvasive serological models INPR, APRI, and FIB-4. The Kruskal-Wallis H test was used for comparison of continuous data between multiple groups, and the chi-square test was used for comparison of categorical data between multiple groups. A Spearman correlation analysis was used to evaluate the correlation between noninvasive models and liver fibrosis stage. The receiver operating characteristic (ROC) curve was used to evaluate the efficacy of the noninvasive serological models in the diagnosis of liver fibrosis degree, and the DeLong method was used for comparison of the area under the ROC curve (AUC). Results A total of 143 patients with PBC were enrolled in the study, among whom 4 had stage S0 liver fibrosis, 50 had stage S1 liver fibrosis, 46 had stage S2 liver fibrosis, 26 had stage S3 liver fibrosis, and 17 had stage S4 liver fibrosis. There was a significant difference in INPR value between the PBC patients with different liver fibrosis degrees (χ2=27.347, P < 0.001). INPR value gradually increased with the aggravation of liver fibrosis degree, and INPR was positively correlated with liver fibrosis degree (r=0.419, P < 0.01). The ROC curve analysis showed that INPR, APRI, and FIB-4 had an AUC of 0.691, 0.706, and 0.742, respectively, in the diagnosis of significant liver fibrosis (≥S2) in PBC patients, at the corresponding cut-off values of 0.63, 0.59, and 2.68, respectively. INPR, APRI, and FIB-4 had an AUC of 0.731, 0.675, and 0.756, respectively, in the diagnosis of progressive hepatic fibrosis (≥S3) in PBC patients, at the corresponding cut-off values of 0.64, 1.23, and 4.63, respectively. INPR, APRI, and FIB-4 had an AUC of 0.820, 0.786, and 0.818, respectively, in the diagnosis of liver cirrhosis (S4) in PBC patients, at the corresponding cut-off values of 0.95, 1.26, and 4.63, respectively. In the evaluation of significant liver fibrosis, progressive liver fibrosis, and liver cirrhosis, there was no significant difference in AUC between INPR and APRI/FIB-4 (all P > 0.05). Conclusion INPR is a simple and accurate noninvasive model for the evaluation of liver fibrosis and has a certain value in the diagnosis of liver fibrosis in PBC. -
Key words:
- Liver Cirrhosis /
- Cholangitis /
- Diagnosis
-
表 1 不同肝纤维化分期患者的临床资料比较
指标 S0(n=4) S1(n=50) S2(n=46) S3(n=26) S4(n=17) χ2值 P值 男/女(例) 0/4 6/44 7/39 1/25 1/16 2.485 0.640 年龄(岁) 54.0(49.3~64.8) 55.0(44.8~62.0) 52.0(47.0~63.0) 60.5(50.3~65.0) 54.0(49.5~65.5) 4.761 0.313 INPR 0.39(0.33~1.02) 0.52(0.43~0.69) 0.64(0.46~1.02) 0.81(0.63~1.18)2) 1.39(0.81~1.78)1)2)3) 27.347 <0.001 APRI 0.34(0.20~0.71) 0.64(0.37~1.32) 1.06(0.69~2.50) 1.30(0.72~1.71) 2.19(1.28~3.81)1)2) 23.942 <0.001 FIB-4 1.40(1.02~2.36) 2.02(1.19~3.76) 3.09(1.88~5.19) 5.00(2.48~6.01)2) 7.89(4.98~10.30)1)2)3) 34.211 <0.001 INR 0.96(0.90~1.02) 0.95(0.90~1.00) 0.99(0.94~1.04) 0.96(0.91~1.04) 1.11(0.96~1.22) 15.843 0.003 PLT(×109/L) 248.0(121.3~289.3) 172.0(145.3~225.0) 158.0(102.5~223.0) 116.0(85.8~156.5) 88.0(67.5~107.5) 24.518 <0.001 ALT(U/L) 29.0(21.3~38.3) 46.5(24.0~91.0) 59.0(35.8~101.2) 39.5(23.2~62.0) 63.0(29.5~96.0) 7.308 0.120 AST(U/L) 24.0(23.0~40.0) 45.5(24.0~70.5) 61.5(34.5~114.2) 55.5(33.0~70.2) 69.0(38.0~110.5) 13.626 0.009 GGT(U/L) 102.5(46.8~418.5) 140.5(47.5~311.5) 163.5(76.5~379.3) 243.0(115.5~386.8) 178.0(78.0~261.5) 4.826 0.306 ALP(U/L) 151.5(77.0~229.0) 151.0(97.5~232.8) 223.0(121.8~359.5) 229.0(103.0~315.3) 202.0(152.0~371.0) 7.420 0.115 Alb(g/L) 43.6(40.5~46.7) 39.8(38.5~42.3) 38.5(34.6~41.3) 38.4(34.3~42.4) 34.6(29.5~38.7) 21.543 <0.001 RDW(%) 13.5(12.8~14.7) 13.5(12.7~15.0) 14.5(13.3~16.1) 14.2(13.6~16.8) 16.5(14.9~16.8) 20.972 <0.001 TBil(μmol/L) 12.4(10.6~13.7) 10.7(7.7~18.0) 12.9(9.1~34.2) 15.3(12.3~19.2) 25.0(12.9~70.1) 13.120 0.011 DBil(μmol/L) 5.5(4.2~7.7) 5.0(3.5~9.0) 7.0(4.8~29.9) 9.1(5.9~13.2) 14.4(7.2~50.1) 14.498 0.006 IBil(μmol/L) 6.4(5.7~7.2) 4.9(3.5~8.0) 5.4(4.1~7.0) 5.6(4.2~7.0) 6.2(4.8~9.0) 5.126 0.275 注:与S0分期比较,1)P<0.05;与S1分期比较,2)P<0.05;与S2分期比较,3)P<0.05。 表 2 INPR、APRI及FIB-4对PBC显著肝纤维化的诊断价值
指标 AUC P值 95%CI cut-off值 敏感度(%) 特异度(%) 准确度(%) INPR 0.691 <0.001 0.609~0.766 0.63 67.42 68.52 67.80 APRI 0.706 <0.001 0.625~0.780 0.59 82.02 51.85 70.60 FIB-4 0.742 <0.001 0.662~0.811 2.68 69.66 70.37 69.20 表 3 INPR、APRI及FIB-4对PBC进展期肝纤维化的诊断价值
指标 AUC P值 95%CI cut-off值 敏感度(%) 特异度(%) 准确度(%) INPR 0.731 <0.001 0.650~0.801 0.64 84.09 62.63 69.90 APRI 0.675 0.0003 0.591~0.751 1.23 65.91 67.68 66.40 FIB-4 0.756 <0.001 0.677~0.824 4.63 68.18 81.82 76.90 表 4 INPR、APRI及FIB-4对PBC肝硬化的诊断价值
指标 AUC P值 95%CI cut-off值 敏感度(%) 特异度(%) 准确度(%) INPR 0.820 <0.001 0.747~0.879 0.95 77.78 77.60 77.60 APRI 0.786 <0.001 0.709~0.850 1.26 88.89 64.80 66.40 FIB-4 0.818 <0.001 0.745~0.878 4.63 88.89 68.80 74.80 -
[1] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Consensus on the diagnosis and management of primary biliary cirrhosis (cholangitis)(2015)[J]. J Clin Hepatol, 2015, 31(12): 1980-1988. DOI: 10.3969/j.issn.1001-5256.2015.12.004.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会感染病学分会. 原发性胆汁性肝硬化(又名原发性胆汁性胆管炎)诊断和治疗共识(2015)[J]. 临床肝胆病杂志, 2015, 31(12): 1980-1988. DOI: 10.3969/j.issn.1001-5256.2015.12.004. [2] LIU X, LIU YP, GAO XS, et al. Progress on dyslipidemia in primary biliary cholangitis[J/CD]. Chin J Liver Dis (Electronic Version), 2020, 12(3): 17-22. DOI: 10.3969/j.issn.1674-7380.2020.03.004.刘晓, 刘亚平, 高学松, 等. 原发性胆汁性胆管炎合并血脂异常研究进展[J/CD]. 中国肝脏病杂志(电子版), 2020, 12(3): 17-22. DOI: 10.3969/j.issn.1674-7380.2020.03.004. [3] CORPECHOT C. Utility of noninvasive markers of fibrosis in cholestatic liver diseases[J]. Clin Liver Dis, 2016, 20(1): 143-158. DOI: 10.1016/j.cld.2015.08.013. [4] JIANG M, YAN X, SONG X, et al. Total bile acid to platelet ratio: A noninvasive index for predicting liver fibrosis in primary biliary cholangitis[J]. Medicine (Baltimore), 2020, 99(22): e20502. DOI: 10.1097/MD.0000000000020502. [5] TAKAKI S, KAWAKAMI Y, MIYAKI D, et al. Non-invasive liver fibrosis score calculated by combination of virtual touch tissue quantification and serum liver functional tests in chronic hepatitis C patients[J]. Hepatol Res, 2014, 44(3): 280-287. DOI: 10.1111/hepr.12129. [6] DING R, ZHENG J, HUANG D, et al. INR-to-platelet ratio (INPR) as a novel noninvasive index for predicting liver fibrosis in chronic hepatitis B[J]. Int J Med Sci, 2021, 18(5): 1159-1166. DOI: 10.7150/ijms.51799. [7] LINDOR KD, BOWLUS CL, BOYER J, et al. Primary biliary cholangitis: 2018 Practice Guidance from the American Association for the Study of Liver Diseases[J]. Hepatology, 2019, 69(1): 394-419. DOI: 10.1002/hep.30145. [8] ROLL J, BOYER JL, BARRY D, et al. The prognostic importance of clinical and histologic features in asymptomatic and symptomatic primary biliary cirrhosis[J]. N Engl J Med, 1983, 308(1): 1-7. DOI: 10.1056/NEJM198301063080101. [9] CHRISTENSEN E, NEUBERGER J, CROWE J, et al. Beneficial effect of azathioprine and prediction of prognosis in primary biliary cirrhosis. Final results of an international trial[J]. Gastroenterology, 1985, 89(5): 1084-1091. DOI: 10.1016/0016-5085(85)90213-6. [10] LAMMERS WJ, KOWDLEY KV, van BUUREN HR. Predicting outcome in primary biliary cirrhosis[J]. Ann Hepatol, 2014, 13(4): 316-326. [11] MEHTA SH, LAU B, AFDHAL NH, et al. Exceeding the limits of liver histology markers[J]. J Hepatol, 2009, 50(1): 36-41. DOI: 10.1016/j.jhep.2008.07.039. [12] SCHLICHTING P, HØLUND B, POULSEN H. Liver biopsy in chronic aggressive hepatitis. Diagnostic reproducibility in relation to size of specimen[J]. Scand J Gastroenterol, 1983, 18(1): 27-32. DOI: 10.3109/00365528309181554. [13] CHENG DY, LI B, JI SB, et al. Application of transient elastography in noninvasive diagnosis of liver fibrosis[J/CD]. Chin J Liver Dis: Electronic Edition, 2021, 13(4): 9-13. DOI: 10.3969/j.issn.1674-7380.2021.04.003.程丹颖, 李贲, 纪世博, 等. 瞬时弹性成像技术在肝纤维化无创诊断中的应用[J/CD]. 中国肝脏病杂志(电子版), 2021, 13(4): 9-13. DOI: 10.3969/j.issn.1674-7380.2021.04.003. [14] QIU LX, LIANG S, FAN ZP, et al. Value of FibroScan in the diagnosis of progressive liver fibrosis in patients with chronic hepatitis C and related influencing factors[J]. J Clin Hepatol, 2019, 35(9): 1950-1953. DOI: 10.3969/j.issn.1001-5256.2019.09.013.仇丽霞, 梁珊, 范作鹏, 等. FibroScan对慢性丙型肝炎进展期肝纤维化的诊断价值及其影响因素[J]. 临床肝胆病杂志, 2019, 35(9): 1950-1953. DOI: 10.3969/j.issn.1001-5256.2019.09.013. [15] BASHOUR FN, TERAN JC, MULLEN KD. Prevalence of peripheral blood cytopenias (hypersplenism) in patients with nonalcoholic chronic liver disease[J]. Am J Gastroenterol, 2000, 95(10): 2936-2939. DOI: 10.1111/j.1572-0241.2000.02325.x. [16] WRIGHT M, GOLDIN R, FABRE A, et al. Measurement and determinants of the natural history of liver fibrosis in hepatitis C virus infection: A cross sectional and longitudinal study[J]. Gut, 2003, 52(4): 574-579. DOI: 10.1136/gut.52.4.574. [17] LIANG XE, DAI L, YANG SL, et al. Combining routine markers improves the accuracy of transient elastography for hepatitis B cirrhosis detection[J]. Dig Liver Dis, 2016, 48(5): 512-518. DOI: 10.1016/j.dld.2016.02.002. [18] WANG H, XU H, WANG X, et al. Red blood cell distribution width to platelet ratio is related to histologic severity of primary biliary cirrhosis[J]. Medicine (Baltimore), 2016, 95(11): e3114. DOI: 10.1097/MD.0000000000003114. [19] MA JL, WANG R, ZHANG FK, et al. A noninvasive diagnostic model of liver fibrosis using serum markers in primary biliary cirrhosis[J]. Chin J Intern Med, 2012, 51(8): 618-622. DOI: 10.3760/cma.j.issn.0578-1426.2012.08.011.马佳丽, 王蕊, 张福奎, 等. 原发性胆汁性肝硬化无创性肝纤维化诊断模型的建立[J]. 中华内科杂志, 2012, 51(8): 618-622. DOI: 10.3760/cma.j.issn.0578-1426.2012.08.011. [20] JOSHITA S, UMEMURA T, OTA M, et al. AST/platelet ratio index associates with progression to hepatic failure and correlates with histological fibrosis stage in Japanese patients with primary biliary cirrhosis[J]. J Hepatol, 2014, 61(6): 1443-1445. DOI: 10.1016/j.jhep.2014.07.036. 期刊类型引用(5)
1. 吴昊,郑欣,朱磊,杨冬. 以肝损害为主要表现的嗜酸粒细胞增多症1例报告. 临床肝胆病杂志. 2022(04): 883-885 .  本站查看
本站查看2. 范松松,张芳,杨立鹏,曹学峰,卢艳敏,张兴元. 慢性胆管炎伴间质黏液变性误诊为胆管癌1例报告. 临床肝胆病杂志. 2022(07): 1626-1628 .  本站查看
本站查看3. 麻芝英,杨显文. 16例IgG_4相关硬化性胆管炎患者的临床特点及诊治分析. 内科. 2022(03): 322-324 .  百度学术
百度学术4. 杨显文,麻芝英. 以黄疸为首发表现不伴AIP的IgG4相关硬化性胆管炎1例. 中国医药导报. 2022(24): 175-178 .  百度学术
百度学术5. 龚沁,张红星,陆敏丹,宛传丹,浦晓红. 血清免疫球蛋白G4在相关疾病中的分布特征与诊断价值. 实用检验医师杂志. 2022(04): 412-415 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 2505 KB)
PDF下载 ( 2505 KB)

 下载:
下载:
 百度学术
百度学术

