无胆道重建肝切除术后胆漏危险因素的Meta分析
DOI: 10.3969/j.issn.1001-5256.2022.03.019
Risk factors for bile leakage after hepatectomy without biliary reconstruction: A Meta - analysis
-
摘要:
目的 系统探讨无胆道重建肝切除术后胆漏的危险因素。 方法 计算机检索中国知网、万方、维普、PubMed、Embase、Web of Science、Cochrane Library等数据库,收集从建库至2021年4月国内外关于无胆道重建肝切除术后胆漏相关危险因素的研究报道,检索语言仅限于中文和英文。按照Cochrane系统评价方法筛选文献、提取资料并运用纽卡斯尔-渥太华量表进行质量评价。应用RevMan 5.4软件对提取的数据进行Meta分析。 结果 共纳入16篇文献,其中英文13篇,中文3篇,总病例数16 036例。Meta分析结果显示,性别(OR=1.27,95%CI:1.09~1.48,P=0.003)、糖尿病(OR=1.23,95%CI:1.07~1.41,P=0.003)、既往肝脏手术史(OR=2.50,95%CI:1.74~3.59,P < 0.001)、解剖性肝切除(OR=1.58,95%CI:1.09~2.30,P=0.02)、Ⅰ段肝切除(OR=2.56,95%CI:1.50~4.40,P < 0.001)、中央肝切除(S4、S5、S8)(OR=3.51,95%CI:2.80~4.40,P < 0.001)、左三肝切除(OR=3.53,95%CI:2.32~5.36,P < 0.001)、术中输血(OR=2.64,95%CI:1.93~3.60,P < 0.001)为肝切除术后胆漏的危险因素。肝硬化、术前肝功能分级、术前化疗、左/右半肝切除不是胆漏的危险因素(P值均>0.05)。 结论 影响肝切除术后胆漏的因素较复杂,除性别、糖尿病、既往肝脏手术史等患者自身因素外,术式、切肝范围、术中输血等术中因素也是肝切除术后发生胆漏的危险因素,术者应进行充分的术前评估,术中谨慎操作,以尽可能降低术后胆漏的发生。 -
关键词:
- 肝切除术 /
- 胆漏 /
- 危险因素 /
- Meta分析(主题)
Abstract:Objective To investigate the risk factors for bile leakage after hepatectomy without biliary reconstruction. Methods CNKI, Wanfang Data, VIP, PubMed, Embase, Web of Science, and The Cochrane Library were searched for English and Chinese study reports on the risk factors for bile leakage after hepatectomy without biliary reconstruction published up to April 2021. The method of Cochrane systematic review was used for literature screening and data extraction, and Newcastle-Ottawa Scale was used for quality assessment. RevMan 5.4 software was used to perform a meta-analysis of the extracted data. Results A total of 16 articles (13 in English and 3 in Chinese) were included in this study, with a total of 16036 cases. The meta-analysis showed that sex (odds ratio [OR]=1.27, 95%CI: 1.09-1.48, P=0.003), diabetes (OR=1.23, 95%CI: 1.07-1.41, P=0.003), past history of liver surgery (OR=2.50, 95%CI: 1.74-3.59, P < 0.001), anatomic hepatectomy (OR=1.58, 95%CI: 1.09-2.30, P=0.02), segment I hepatectomy (OR=2.56, 95%CI: 1.50-4.40, P < 0.001), central hepatectomy (S4, S5, S8) (OR=3.51, 95%CI: 2.80-4.40, P < 0.001), left third hepatectomy (OR=3.53, 95%CI: 2.32-5.36, P < 0.001), and intraoperative blood transfusion (OR=2.64, 95%CI: 1.93-3.60, P < 0.001) were the risk factors for bile leakage after hepatectomy. Liver cirrhosis, preoperative liver function grade, preoperative chemotherapy, and left/right hemihepatectomy were not the risk factors for bile leakage. Conclusion There are complex influencing factors for bile leakage after hepatectomy, and in addition to the patient's own factors such as sex, diabetes, and past history of liver surgery, intraoperative factors, such as surgical procedures, extent of hepatectomy, and intraoperative blood transfusion, are also risk factors for bile leakage after hepatectomy. The surgeon should conduct adequate preoperative assessment and perform careful operation during surgery to reduce the incidence rate of postoperative bile leakage. -
Key words:
- Hepatectomy /
- Bile Leakage /
- Risk Factors /
- Meta-Analysis as Topic
-
目前肝切除术已成为肝脏良恶性疾病的主要治疗方式之一,尽管肝切除术后并发症的发生率明显降低,但胆漏的发生率未见明显改变[1-3]。胆漏可造成腹腔感染、膈下脓肿甚至肝衰竭等严重并发症,造成患者住院时间延长甚至死亡,是肝切除术后主要并发症之一[4-5]。但对肝切除术后胆漏的诊疗仍缺乏规范统一的方法,常常延误最佳治疗时机,加重患者病情[6],因而明确胆漏的危险因素,从预防入手,尽可能的降低术后胆漏的发生显得尤为重要。
本研究运用Meta分析的方法进一步明确无胆道重建肝切除术后胆漏的相关危险因素,旨在为临床防治胆漏提供参考。
1. 资料与方法
1.1 文献检索
计算机检索中国知网、万方、维普、PubMed、Embase、Web of Science、Cochrane Library等数据库,收集从建库至2021年4月国内外关于无胆道重建肝切除术后胆漏相关危险因素的研究报道。检索过程由2名研究者独立完成,如有分歧则通过协商解决,必要时与第三人协商。中文检索词包括:“肝切除”“胆漏”“危险因素”等,英文检索词包括:“hepatectomy”“liver resection”“bile leakage”“biliary leakage”“risk factor”等。对所有纳入文献的参考文献进行手动检索以扩大检索范围。
1.2 纳入与排除标准
1.2.1 纳入标准
(1) 治疗方式为肝切除术,不限疾病种类和研究类型;(2)研究目的为分析肝切除术后胆漏危险因素的研究报道;(3)语言仅限于中文和英文;(4)提供了胆漏组和未发生胆漏组病例数量,且对相关因素进行了比较;(5)资料完整,数据详实,纳入及排除标准类似。
1.2.2 排除标准
(1) 研究中纳入了肝切除伴有胆道重建的病例;(2)缺乏对照组的研究;(3)会议论文、重复报道、病例报告、综述等;(4)信息缺失、质量严重不足;(5)研究内容与本研究不符。
1.3 文献筛选与资料提取
文献筛选和资料提取均由2名研究者独立完成,过程中所产生的分歧通过协商解决,必要时由第三方裁定。检索所得文献均通过阅读“题目-摘要”进行初步筛选,通过初筛的文献逐一仔细阅读全文予以进一步筛选。一般资料包括:第一作者、发表年份、国家、样本量、患者的性别、年龄以及胆漏和未发生胆漏的例数等。
1.4 文献质量评价
使用纽卡斯尔-渥太华量表(the Newcastle-Ottawa scale,NOS)进行文献质量评价,分别从患者选择、试验组的可比性及结果评估3个方面进行文献质量评分,总分9分,评分≥5分认为是高质量研究[7]。
1.5 统计学方法
应用RevMan 5.4软件对数据进行Meta分析。采用I2统计量法和Q检验法进行异质性检验(P < 0.1或I2>50%考虑存在异质性),根据异质性检验结果选用固定效应模型或随机效应模型合并数据,计算OR及95%CI,P < 0.05为差异有统计学意义。当存在显著异质性时,进行敏感性分析,即通过每次剔除单项研究来评估该研究对于合成效应量的影响变化,比较剔除前后有无显著差异性,以寻找敏感性的来源并评估研究的稳定性。采用Egger检验法进行发表性偏倚分析,P>0.1提示不存在发表偏倚。
2. 结果
2.1 文献筛选流程与纳入文献基本特征
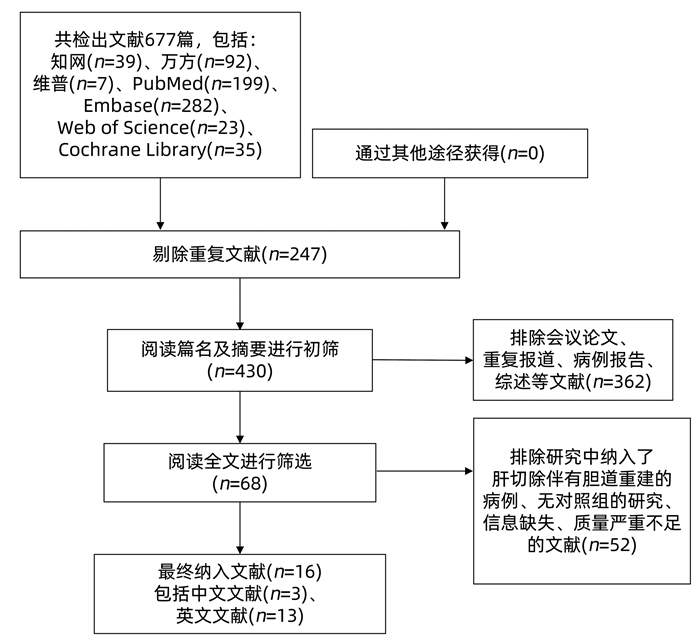
通过检索获得文献677篇,根据纳入及排除标准进行剔除,再经质量评价,最终纳入16篇文献[2, 8-22]。其中3篇为中文文献,13篇为英文文献,均为回顾性研究。总病例数16 036例,其中胆漏组1330例,未胆漏组14 706例,胆漏总发生率为9%。文献筛选流程详见图 1。纳入文献的基本特征及质量评价见表 1。
表 1 纳入研究的基本特征及质量评价作者 年份 国家 样本量(例) 男/女(例) 年龄(岁) 结果(漏/未漏,例) 质量评价(分) Yamashita等[2] 2021 日本 10 102 8039/2063 726/9376 7 Sakamoto等[8] 2016 日本 334 242/92 32~87 30/304 6 Sadamori等[9] 2013 日本 359 292/67 32~89 46/313 6 Panaro等[10] 2016 法国 411 240/171 18~84 42/369 7 Nakano等[11] 2018 日本 556 445/111 28/528 7 Capussotti等[12] 2006 意大利 610 369/241 2~86 22/588 5 Donadon等[13] 2016 意大利 475 326/149 23~85 72/403 6 Erdogan等[14] 2008 荷兰 234 113/121 16/218 6 Guillaud等[15] 2013 法国 1001 683/318 16~90 80/921 6 Harimoto等[16] 2020 日本 270 195/75 28~89 11/259 5 Sadamori等[17] 2010 日本 293 238/55 32~89 38/255 5 Ishii等[18] 2011 日本 247 158/89 26/221 5 Kajiwara等[19] 2016 日本 518 364/154 20~84 81/437 6 吕孟斐等[20] 2015 中国 201 159/42 1~70 42/159 5 邓仲鸣等[21] 2016 中国 109 74/35 22~73 23/86 5 翟中山[22] 2015 中国 316 179/137 20~74 47/269 6 通过全文阅读和资料归纳提取后,选取了13项指标进行Meta分析,分别为:性别、肝硬化、糖尿病、术前肝功能(Child-Pugh A/B分级)、解剖性肝切除、半肝切除(左/右)、Ⅰ段切除、中央肝切除(S4、S5、S8)、左三肝切除、术中输血、术前化疗、既往肝脏手术史。
2.2 Meta分析结果
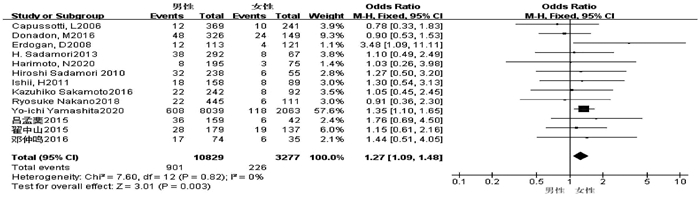
2.2.1 性别
共13篇文献[2, 8-9, 11-14, 16-18, 20-22]研究因素涉及性别。试验组为男性,对照组为女性。各研究之间无异质性(I2=0,P=0.82),采用固定效应模型进行合并分析,结果显示,两组比较差异具有统计学意义(OR=1.27,95%CI:1.09~1.48,P=0.003)(图 2)。
2.2.2 肝硬化
共8篇文献[8, 12-14, 16, 20-22]研究因素涉及肝硬化。试验组为有肝硬化,对照组为无肝硬化。各研究之间存在显著异质性(I2=82%,P < 0.001),运用排除法进行敏感性分析,对纳入文献进行逐一剔除后,结果未发生实质性变化。采用随机效应模型进行合并分析,结果显示,两组比较差异无统计学意义(OR=0.79,95%CI:0.36~1.73,P=0.55)(图 3)。
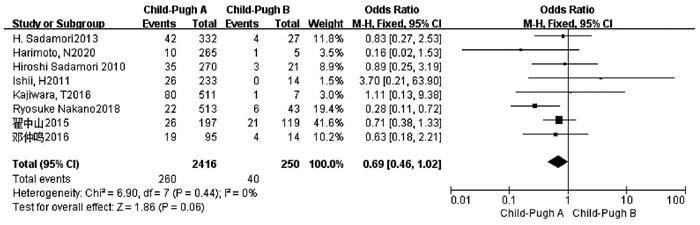
2.2.3 术前肝功能Child-Pugh A/B
共有8篇文献[9, 11, 16-19, 21-22]研究因素涉及术前肝功能Child-Pugh A/B分级,且所有文献均排除了术前Child-Pugh C级患者。试验组为Child-Pugh A级患者,对照组为Child-Pugh B级患者。各研究之间无异质性(I2=0,P=0.44),采用固定效应模型进行合并分析,结果显示,两组比较差异无统计学意义(OR=0.69,95%CI:0.46~1.02,P=0.06)(图 4)。
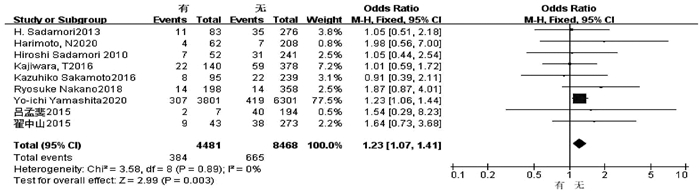
2.2.4 糖尿病
共9篇文献[2, 8-9, 11, 16-17, 19, 20, 22]研究因素涉及糖尿病。试验组为有糖尿病,对照组为无糖尿病。各研究之间无异质性(I2=0,P=0.89),采用固定效应模型进行合并分析,结果显示,两组比较差异有统计学意义(OR=1.23,95%CI:1.07~1.41,P=0.003)(图 5)。
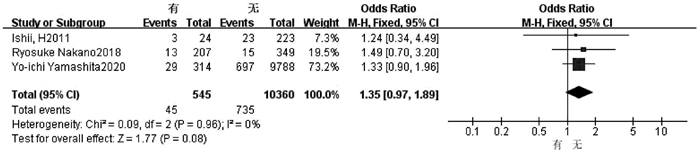
2.2.5 术前化疗
3篇文献[2, 11, 18]研究因素涉及术前化疗。试验组为术前有化疗史,对照组为术前无化疗史。各研究之间无异质性(I2=0,P=0.96),采用固定效应模型进行合并分析,结果显示,两组比较差异无统计学意义(OR=1.35,95%CI:0.97~1.89,P=0.08)(图 6)。
2.2.6 既往肝脏手术史
共5篇文献[8, 14-15, 17, 22]研究因素涉及既往肝脏手术史。试验组为既往有手术史,对照组为既往无手术史。各研究之间无异质性(I2=34%,P=0.20),采用固定效应模型进行合并分析,结果显示,两组比较差异有统计学意义(OR=2.50,95%CI:1.74~3.59,P < 0.001)(图 7)。
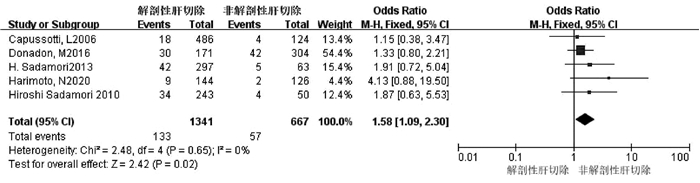
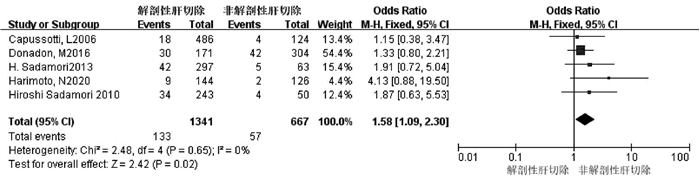
2.2.7 解剖性肝切除
共5篇文献[9, 12-13, 16-17]研究因素涉及解剖性/非解剖性肝切除因素。试验组为解剖性肝切除,对照组为非解剖性肝切除。各研究之间无异质性(I2=0,P=0.65),采用固定效应模型进行合并分析,结果显示,两组比较差异有统计学意义(OR=1.58,95%CI:1.09~2.30,P=0.02)(图 8)。
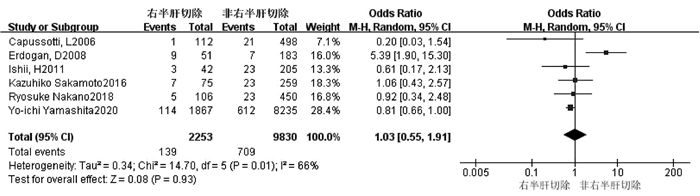
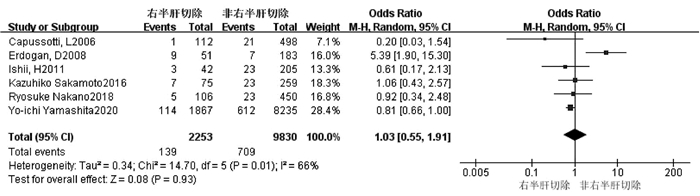
2.2.8 右半肝切除
共6篇文献[2, 8, 11-12, 14, 18]研究因素涉及右半肝切除。试验组为右半肝切除,对照组为非右半肝切除。各研究之间存在轻度异质性(I2=66%,P=0.01),运用排除法进行敏感性分析,对纳入文献进行逐一剔除后,结果未发生实质性变化。采用随机效应模型进行合并分析,结果显示,两组比较差异无统计学意义(OR=1.03,95%CI:0.55~1.91,P=0.93)(图 9)。
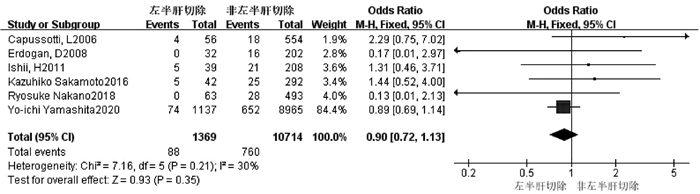
2.2.9 左半肝切除
共6篇文献[2, 8, 11-12, 14, 18]研究因素涉及左半肝切除。试验组为左半肝切除,对照组为非左半肝切除。各研究之间无异质性(I2=30%,P=0.21),采用固定效应模型进行合并分析,结果显示,两组比较差异无统计学意义(OR=0.90,95%CI:0.72~1.13,P=0.35)(图 10)。
2.2.10 Ⅰ段肝切除
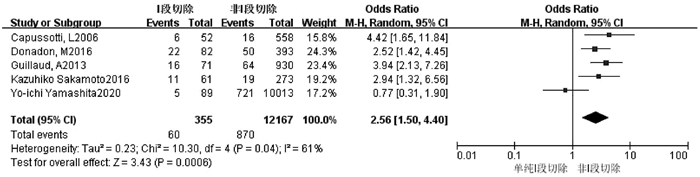
共5篇文献[2, 8, 12-13, 15]研究因素涉及Ⅰ段切除。试验组为Ⅰ段肝切除,对照组为非Ⅰ段肝切除。各研究之间存在轻度异质性(I2=61%,P=0.04),运用排除法进行敏感性分析,对纳入文献进行逐一剔除后,结果未发生实质性变化。采用随机效应模型进行合并分析,结果显示,两组比较差异有统计学意义(OR=2.56,95%CI:1.50~4.40,P < 0.001)(图 11)。
2.2.11 中央肝切除(S4、S5、S8)
共5篇文献[2, 11-12, 15, 18]研究因素涉及中央肝切除。试验组为中央肝切除,对照组为非中央肝切除。各研究之间无异质性(I2=21%,P=0.28),采用固定效应模型进行合并分析,结果显示,两组比较差异有统计学意义(OR=3.51,95%CI:2.80~4.40,P < 0.001)(图 12)。
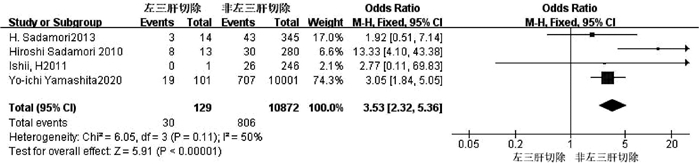
2.2.12 左三肝切除
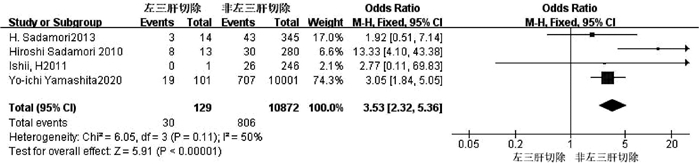
共4篇文献[2, 9, 17, 18]研究因素涉及左三肝切除。试验组为左三肝切除,对照组为非左三肝切除。各研究之间异质性较小(I2=50%,P=0.11),采用固定效应模型进行合并分析,结果显示,两组比较差异有统计学意义(OR=3.53,95%CI:2.32~5.36,P < 0.001)(图 13)。
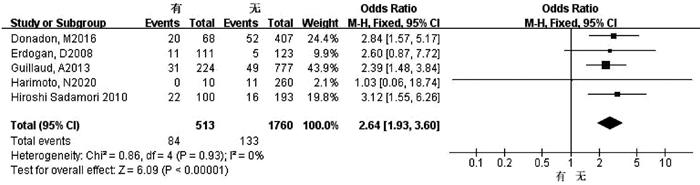
2.2.13 术中输血
共5篇文献[13-17]研究因素涉及术中输血。试验组为有术中输血,对照组为无术中输血。各研究之间无异质性(I2=0,P=0.93),采用固定效应模型进行合并分析,结果显示,两组比较差异有统计学意义(OR=2.64,95%CI:1.93~3.60,P < 0.001)(图 14)。
2.3 偏倚分析
Egger检验结果显示,解剖性肝切除(P=0.158)、Child-Pugh A/B(P=0.777)、右半肝切除(P=0.680)、左半肝切除(P=0.964)、Ⅰ段肝切除(P=0.742)、中央肝切除(P=0.796)、左三肝切除(P=0.892)、性别(P=0.545)、术中输血(P=0.515)、糖尿病(P= 0.759)、既往手术史(P=0.529)、术前化疗(P=0.901)、肝硬化(P=0.944)均不存在发表偏倚。
3. 讨论
胆漏是肝切除术后的常见并发症,严重影响患者预后。有报道[23]显示肝切除术后胆漏的发生率为3.1%~28.0%,这与以往的研究[2-3, 24]结果相似。在本研究中,总体胆漏率约为9%,表明随着肝脏外科的发展,胆漏依然是一个十分棘手的问题。尽管近年来对于肝切除术后胆漏相关危险因素的研究已经从单纯对手术因素的讨论扩展至整个围手术期,但众多研究之间对于胆漏危险因素的认识仍存在较大争议[2, 25-27]。
本Meta分析结果表明男性、糖尿病、既往肝脏手术史、术中输血是肝切除术后胆漏的高危因素,且解剖性肝切除相较于非解剖性肝切除更容易发生术后胆漏,中央肝切除、Ⅰ段肝切除、左三肝切除相对于其他手术方式具有更高的胆漏风险。而肝硬化、术前肝功能分级、术前化疗史不是术后胆漏的危险因素,左/右半肝切除术相较于非左/右半肝切除术胆漏的风险并未明显增加。
既往研究[28-29]多认为性别并不是胆漏的危险因素,但本研究分析显示男性更容易发生胆漏,这可能受BMI的影响[30],然而笔者未能提取到相关数据进一步分析。既往肝脏手术造成肝周粘连、肝脏解剖结构紊乱等,使得术中组织辨别困难,手术难度增加,易发生术后胆漏[27, 31],因而对于有肝脏手术史的患者,术者应加强围手术期管理,术中仔细操作,必要时可运用胆漏试验(即逆行胆管灌注脂肪乳、水、亚甲蓝等特异性物质, 观察创面有无渗出,检查有无胆漏)等多种方法,以预防术后胆漏的发生。虽然糖尿病被认为是外科手术并发症的高危因素[32-34],但糖尿病是否会增加肝切除术后胆漏的发生率一直颇具争议[32-38]。本研究表明糖尿病患者术后更容易发生胆漏。肝切除的类型与胆漏的关系仍不明确,是目前讨论的焦点问题。研究[4, 39-41]多认为胆漏与肝切除位置(如中央肝切除)和切面面积大小(切面面积越大,胆漏风险越高)有关。但还需更多的更高质量的研究进一步明确,以尽可能地降低术后胆漏的发生率。
本研究中,肝硬化、术前肝功能分级、术前化疗并不是胆漏的危险因素,这与以往的研究[1, 42-44]存在差异。笔者认为随着对围手术期管理的重视与规范化,尤其是肝切除术后越来越重视患者的营养支持与肝功能的改善[45],使得术前营养水平、肝功能情况等已不再是影响术后胆漏的主要因素。但对于术前化疗应引起足够的重视。因为随着肝切除适应证的拓宽,越来越多的肿瘤患者,诸如结肠癌肝转移的患者,多在应用全身化疗后有机会进行手术治疗[46],故术前化疗是否会增加术后胆漏的发生这一问题亟需解决。尽管本研究分析结果显示术前化疗不是胆漏的危险因素,但纳入文献仅3篇,因而降低了证据力度,未来还需更多的研究论证该问题。同时由于笔者没有提取到相应的数据分析对于不同性质肝脏疾病是否会影响胆漏的发生,此问题亦需更多的研究探讨。
本研究也存在诸多不足。首先,研究时间跨度大,可能存在文章检索不全,造成资料收集不全面。同时,因胆漏的诊断缺乏统一的标准,纳入文献采用的诊断标准并不统一,可能会对结果造成影响,降低证据力度。其次,因各研究报道中纳入的因素较多,本研究只提取了部分可进行合并的指标,尤其是对于手术相关指标相对缺乏,导致结果不全面。最后,结局指标中肝硬化、Ⅰ段肝切除与右半肝切除的各研究之间存在异质性,敏感性分析并未找到异质性来源,同时也未能获得更多的数据进行亚组分析,采用随机效应模型进行合并,使得证据力度降低。
综上所述,男性、糖尿病、既往肝脏手术史、解剖性肝切除、中央肝切除、Ⅰ段肝切除、左三肝切除、术中输血是肝切除术后发生胆漏的危险因素,对于此类患者,术者应更加重视对于术后胆漏的预防。
-
表 1 纳入研究的基本特征及质量评价
作者 年份 国家 样本量(例) 男/女(例) 年龄(岁) 结果(漏/未漏,例) 质量评价(分) Yamashita等[2] 2021 日本 10 102 8039/2063 726/9376 7 Sakamoto等[8] 2016 日本 334 242/92 32~87 30/304 6 Sadamori等[9] 2013 日本 359 292/67 32~89 46/313 6 Panaro等[10] 2016 法国 411 240/171 18~84 42/369 7 Nakano等[11] 2018 日本 556 445/111 28/528 7 Capussotti等[12] 2006 意大利 610 369/241 2~86 22/588 5 Donadon等[13] 2016 意大利 475 326/149 23~85 72/403 6 Erdogan等[14] 2008 荷兰 234 113/121 16/218 6 Guillaud等[15] 2013 法国 1001 683/318 16~90 80/921 6 Harimoto等[16] 2020 日本 270 195/75 28~89 11/259 5 Sadamori等[17] 2010 日本 293 238/55 32~89 38/255 5 Ishii等[18] 2011 日本 247 158/89 26/221 5 Kajiwara等[19] 2016 日本 518 364/154 20~84 81/437 6 吕孟斐等[20] 2015 中国 201 159/42 1~70 42/159 5 邓仲鸣等[21] 2016 中国 109 74/35 22~73 23/86 5 翟中山[22] 2015 中国 316 179/137 20~74 47/269 6 -
[1] CHEN X, LI K, WU YZ, et al. Multivariate analysis for risk factors of bile leakage after hepatectomy[J]. Chin J Gen Surg, 2013, 28(11): 850-853. DOI: 10.3760/cma.j.issn.1007-631X.2013.11.011.程翔, 李科, 吴雨哲, 等. 肝切除术后胆漏危险因素的多元回归分析[J]. 中华普通外科杂志, 2013, 28(11): 850-853. DOI: 10.3760/cma.j.issn.1007-631X.2013.11.011. [2] YAMASHITA YI, YAMAMOTO H, MIYATA H, et al. Risk factors for bile leakage: Latest analysis of 10 102 hepatectomies for hepatocellular carcinoma from the Japanese national clinical database[J]. J Hepatobiliary Pancreat Sci, 2021, 28(7): 556-562. DOI: 10.1002/jhbp.827. [3] MIURA F, YAMAMOTO M, GOTOH M, et al. Validation of the board certification system for expert surgeons (hepato-biliary-pancreatic field) using the data of the National Clinical Database of Japan: Part 1 - Hepatectomy of more than one segment[J]. J Hepatobiliary Pancreat Sci, 2016, 23(6): 313-323. DOI: 10.1002/jhbp.344. [4] YUE SQ. Diagnosis and treatment of biliary leakage after hepatectomy[J/CD]. Chin J Hepat Surg (Electronic Edition), 2013, 2(2): 128-130. DOI: 10.3877/cma.j.issn.2095-3232.2013.02.013.岳树强. 肝切除术后胆漏的诊断与治疗[J/CD]. 中华肝脏外科手术学电子杂志, 2013, 2(2): 128-130. DOI: 10.3877/cma.j.issn.2095-3232.2013.02.013. [5] WEN Y, MIAO XY, HUANG SF, et al. The prevention and treatment of bile leakage after the hepatectomy[J]. J Clin Surg, 2005, 13(10): 639-640. DOI: 10.3969/j.issn.1005-6483.2005.10.021.文宇, 苗雄鹰, 黄生福, 等. 肝切除术后胆漏的预防与处理[J]. 临床外科杂志, 2005, 13(10): 639-640. DOI: 10.3969/j.issn.1005-6483.2005.10.021. [6] GUO B, XU XL, HAN JW, et al. Research progress on the bile leakage after hepatectomy[J]. Hebei Med J, 2020, 42(23): 3639-3644. DOI: 10.3969/j.issn.1002-7386.2020.23.031.郭兵, 许晓磊, 韩军伟, 等. 肝切除术后胆漏研究进展[J]. 河北医药, 2020, 42(23): 3639-3644. DOI: 10.3969/j.issn.1002-7386.2020.23.031. [7] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25(9): 603-605. DOI: 10.1007/s10654-010-9491-z. [8] SAKAMOTO K, TAMESA T, YUKIO T, et al. Risk factors and managements of bile leakage after hepatectomy[J]. World J Surg, 2016, 40(1): 182-189. DOI: 10.1007/s00268-015-3156-8. [9] SADAMORI H, YAGI T, SHINOURA S, et al. Risk factors for major morbidity after liver resection for hepatocellular carcinoma[J]. Br J Surg, 2013, 100(1): 122-129. DOI: 10.1002/bjs.8957. [10] PANARO F, HACINA L, BOUYABRINE H, et al. Risk factors for postoperative bile leakage: A retrospective single-center analysis of 411 hepatectomies[J]. Hepatobiliary Pancreat Dis Int, 2016, 15(1): 81-86. DOI: 10.1016/s1499-3872(15)60424-6. [11] NAKANO R, OHIRA M, KOBAYASHI T, et al. Independent risk factors that predict bile leakage after hepatectomy for hepatocellular carcinoma: Cohort study[J]. Int J Surg, 2018, 57: 1-7. DOI: 10.1016/j.ijsu.2018.07.005. [12] CAPUSSOTTI L, FERRERO A, VIGANÔ L, et al. Bile leakage and liver resection: Where is the risk?[J]. Arch Surg, 2006, 141(7): 690-694; discussion 695. DOI: 10.1001/archsurg.141.7.690. [13] DONADON M, COSTA G, CIMINO M, et al. Diagnosis and management of bile leaks after hepatectomy: Resultsof a prospective analysis of 475 hepatectomies[J]. World J Surg, 2016, 40(1): 172-181. DOI: 10.1007/s00268-015-3143-0. [14] ERDOGAN D, BUSCH OR, van DELDEN OM, et al. Incidence and management of bile leakage after partial liver resection[J]. Dig Surg, 2008, 25(1): 60-66. DOI: 10.1159/000118024. [15] GUILLAUD A, PERY C, CAMPILLO B, et al. Incidence and predictive factors of clinically relevant bile leakage in the modern era of liver resections[J]. HPB (Oxford), 2013, 15(3): 224-229. DOI: 10.1111/j.1477-2574.2012.00580.x. [16] HARIMOTO N, MURANUSHI R, HOSHINO K, et al. Albumin-Indocyanine Green Evaluation (ALICE) grade predicts bile leakage after hepatic resection[J]. Surg Today, 2020, 50(8): 849-854. DOI: 10.1007/s00595-020-01955-2. [17] SADAMORI H, YAGI T, MATSUDA H, et al. Risk factors for major morbidity after hepatectomy for hepatocellular carcinoma in 293 recent cases[J]. J Hepatobiliary Pancreat Sci, 2010, 17(5): 709-718. DOI: 10.1007/s00534-010-0275-3. [18] ISHⅡ H, OCHIAI T, MURAYAMA Y, et al. Risk factors and management of postoperative bile leakage after hepatectomy without bilioenteric anastomosis[J]. Dig Surg, 2011, 28(3): 198-204. DOI: 10.1159/000324042. [19] KAJIWARA T, MIDORIKAWA Y, YAMAZAKI S, et al. Clinical score to predict the risk of bile leakage after liver resection[J]. BMC Surg, 2016, 16(1): 30. DOI: 10.1186/s12893-016-0147-0. [20] LYU MF, GUO YM, WANG JG, et al. Analysis of risk factors for bile leakage after hepatectomy[J]. Hebei Med J, 2015, 37(16): 2442-2444. DOI: 10.3969/j.issn.1002-7386.2015.16.012.吕孟斐, 国义民, 王建国, 等. 肝切除术后胆漏的危险因素分析[J]. 河北医药, 2015, 37(16): 2442-2444. DOI: 10.3969/j.issn.1002-7386.2015.16.012. [21] DENG ZM, SUN Q. Risk factors and measures of prevention and treatment for bile leakage after hepatectomy[J]. Chin J Clin Res, 2016, 29(2): 204-206. DOI: 10.13429/j.cnki.cjcr.2016.02.015.邓仲鸣, 孙权. 肝切除术后并发胆漏危险因素及防治措施分析[J]. 中国临床研究, 2016, 29(2): 204-206. DOI: 10.13429/j.cnki.cjcr.2016.02.015. [22] ZHAI ZS. Multivariate regression analysis of risk factors for biliary leakage after hepatic R0 resection[J]. Chin Hepatol, 2015, 20(5): 404-407. DOI: 10.3969/j.issn.1008-1704.2015.05.017.翟中山. 肝R0切除术后发生胆漏危险因素的多元回归分析[J]. 肝脏, 2015, 20(5): 404-407. DOI: 10.3969/j.issn.1008-1704.2015.05.017. [23] KUBO N, SHIRABE K. Treatment strategy for isolated bile leakage after hepatectomy: Literature review[J]. Ann Gastroenterol Surg, 2020, 4(1): 47-55. DOI: 10.1002/ags3.12303. [24] LIU ZY, JIN H, LIU M, et al. Role of bile leakage test in preventing bile leakage during partial liver resection[J]. Chin J Gen Pract, 2014, 13(2): 139-141. DOI: 10.3760/cma.j.issn.1671-7368.2014.02.021.刘志毅, 金虎, 刘明, 等. 胆漏试验在肝部分切除术中预防胆漏的作用[J]. 中华全科医师杂志, 2014, 13(2): 139-141. DOI: 10.3760/cma.j.issn.1671-7368.2014.02.021. [25] LO CM, FAN ST, LIU CL, et al. Biliary complications after hepatic resection: Risk factors, management, and outcome[J]. Arch Surg, 1998, 133(2): 156-161. DOI: 10.1001/archsurg.133.2.156. [26] WU ZW. Analysis of related factors of bile leakage after hepatobiliary surgery[J]. Chin J Modern Operative Surg, 2014, 18(4): 260-262. DOI: 10.16260/j.cnki.1009-2188.2014.04.008.吴忠卫. 肝胆手术后胆漏的相关因素分析[J]. 中国现代手术学杂志, 2014, 18(4): 260-262. DOI: 10.16260/j.cnki.1009-2188.2014.04.008. [27] CHEN XP, PENG SY. Causes and treatment of bile leakage (a report of 22 cases)[J]. Chin J Pract Surg, 2001, 21(2): 102-104. DOI: 10.3321/j.issn:1005-2208.2001.02.020.陈晓鹏, 彭淑牖. 胆漏的原因及防治(附22例报告)[J]. 中国实用外科杂志, 2001, 21(2): 102-104. DOI: 10.3321/j.issn:1005-2208.2001.02.020. [28] ZHENG SM, LI H, LI GC, et al. Risk factors, treatment and impact on outcomes of bile leakage after hemihepatectomy[J]. ANZ J Surg, 2017, 87(7-8): e26-e31. DOI: 10.1111/ans.13073. [29] RAHBARI NN, ELBERS H, KOCH M, et al. Bilirubin level in the drainage fluid is an early and independent predictor of clinically relevant bile leakage after hepatic resection[J]. Surgery, 2012, 152(5): 821-831. DOI: 10.1016/j.surg.2012.03.012. [30] CHEN L, LI Y. The risk factors and prediction systems for posthepatectomy complications[J]. J Clin Hepatol, 2019, 35(1): 217-221. DOI: 10.3969/j.issn.1001-5256.2019.01.048.陈龙, 李钺. 肝切除术后并发症的危险因素及预测评分系统[J]. 临床肝胆病杂志, 2019, 35(1): 217-221. DOI: 10.3969/j.issn.1001-5256.2019.01.048. [31] YANG JM. Attention should be paid to surgical treatment of recurrent primary liver cancer[J]. J Clin Surg, 2005, 13(3): 129-130. DOI: 10.3969/j.issn.1005-6483.2005.03.001.杨甲梅. 重视复发性原发性肝癌的外科治疗[J]. 临床外科杂志, 2005, 13(3): 129-130. DOI: 10.3969/j.issn.1005-6483.2005.03.001. [32] BAGDADE JD, STEWART M, WALTERS E. Impaired granulocyte adherence. A reversible defect in host defense in patients with poorly controlled diabetes[J]. Diabetes, 1978, 27(6): 677-681. DOI: 10.2337/diab.27.6.677. [33] LI Q, WANG Y, MA T, et al. Clinical outcomes of patients with and without diabetes mellitus after hepatectomy: A systematic review and meta-analysis[J]. PLoS One, 2017, 12(2): e0171129. DOI: 10.1371/journal.pone.0171129. [34] INOUE Y, SUZUKI Y, YOKOHAMA K, et al. Diabetes mellitus does not influence results of hepatectomy in hepatocellular carcinoma: Case control study[J]. Contemp Oncol (Pozn), 2020, 24(4): 211-215. DOI: 10.5114/wo.2020.102825. [35] YAMAMOTO K, TAKADA Y, FUJIMOTO Y, et al. Nonalcoholic steatohepatitis in donors for living donor liver transplantation[J]. Transplantation, 2007, 83(3): 257-262. DOI: 10.1097/01.tp.0000250671.06456.3f. [36] FISCHER A, FUCHS J, STRAVODIMOS C, et al. Influence of diabetes on short-term outcome after major hepatectomy: An underestimated risk?[J]. BMC Surg, 2020, 20(1): 305. DOI: 10.1186/s12893-020-00971-w. [37] INOUE Y, SUZUKI Y, YOKOHAMA K, et al. Diabetes mellitus does not influence results of hepatectomy in hepatocellular carcinoma: Case control study[J]. Contemp Oncol (Pozn), 2020, 24(4): 211-215. DOI: 10.5114/wo.2020.102825. [38] LIANG J, ARⅡZUMI SI, NAKANO M, et al. Diabetes mellitus and/or nonalcoholic steatohepatitis-related hepatocellular carcinoma showed favorable surgical outcomes after hepatectomy[J]. Anticancer Res, 2019, 39(10): 5639-5643. DOI: 10.21873/anticanres.13760. [39] YAMASHITA Y, HAMATSU T, RIKIMARU T, et al. Bile leakage after hepatic resection[J]. Ann Surg, 2001, 233(1): 45-50. DOI: 10.1097/00000658-200101000-00008. [40] QIAO O, SUN ZW. Biliary leakage after hepatectomy[J]. J Hepatobiliary Surg, 2003, 11(2): 132-133. DOI: 10.3969/j.issn.1006-4761.2003.02.024.乔鸥, 孙志为. 肝切除术后胆漏[J]. 肝胆外科杂志, 2003, 11(2): 132-133. DOI: 10.3969/j.issn.1006-4761.2003.02.024. [41] NAGANO Y, TOGO S, TANAKA K, et al. Risk factors and management of bile leakage after hepatic resection[J]. World J Surg, 2003, 27(6): 695-698. DOI: 10.1007/s00268-003-6907-x. [42] FRVHLING P, HELLBERG K, EJDER P, et al. The prognostic value of C-reactive protein and albumin in patients undergoing resection of colorectal liver metastases. A retrospective cohort study[J]. HPB (Oxford), 2021, 23(6): 970-978. DOI: 10.1016/j.hpb.2020.10.019. [43] MA B, TANG GY, WANG L, et al. Prediction of independent risk factors for biliary leakage after hepatectomy for hepatocellular carcinoma[J]. Medical Diet and Health, 2018, 12: 72.马斌, 汤光耀, 王麟, 等. 预测肝细胞癌肝切除术后胆漏的独立危险因素[J]. 医学食疗与健康, 2018, 12: 72. [44] SPETZLER VN, SCHEPERS M, PINNSCHMIDT HO, et al. The incidence and severity of post-hepatectomy bile leaks is affected by surgical indications, preoperative chemotherapy, and surgical procedures[J]. Hepatobiliary Surg Nutr, 2019, 8(2): 101-110. DOI: 10.21037/hbsn.2019.02.06. [45] Chinese expert consensus and path management guideline for accelerated rehabilitation surgery (2018): Hepatobiliary surgery[J]. Chin J Anesthesiol, 2018, 38(1): 13-18. DOI: 10.3760/cma.j.issn.0254-1416.2018.01.101.加速康复外科中国专家共识暨路径管理指南(2018): 肝胆手术部分[J]. 中华麻醉学杂志, 2018, 38(1): 13-18. DOI: 10.3760/cma.j.issn.0254-1416.2018.01.101. [46] COSTA G, DONADON M, TORZILLI G. Post-hepatectomy biliary fistula: From risk factors to the role of drain placement and management-still a lot to be answered[J]. Hepatobiliary Surg Nutr, 2019, 8(4): 417-418. DOI: 10.21037/hbsn.2019.06.10. 期刊类型引用(3)
1. 李小归,吴意,卢嘉胤,李浩,汪新天. 肝胆管结石病外科治疗方法疗效的临床研究. 湖南师范大学学报(医学版). 2024(01): 75-80 .  百度学术
百度学术2. 莫书天,彭涛. 肝癌切除术后胆汁漏并发症的预防及彭氏经胆囊测漏技术的应用. 中国普外基础与临床杂志. 2023(06): 641-645 .  百度学术
百度学术3. 杨景瑞,肖瑞,王璐,王家兴,刘少杰,张小冬,王泽锋,冯学敏,靳君华,任建军. 胰十二指肠切除改良胆肠吻合术临床疗效及术后胆漏的影响因素分析. 中华消化外科杂志. 2023(05): 642-649 .  百度学术
百度学术其他类型引用(1)
-




 PDF下载 ( 3488 KB)
PDF下载 ( 3488 KB)


 下载:
下载:













 下载:
下载:





 百度学术
百度学术