多囊卵巢综合征合并非酒精性脂肪性肝病的机制与治疗
DOI: 10.3969/j.issn.1001-5256.2022.03.035
利益冲突声明:所有作者均声明不存在利益冲突。
作者贡献声明:秦婷婷、温晓玉负责拟定写作思路;秦婷婷、魏晓东、张瑞华、邵玥明、张雨负责检索文献,资料分析;秦婷婷负责撰写文章;温晓玉负责修改文章并最终定稿。
Mechanism and treatment of polycystic ovary syndrome with nonalcoholic fatty liver disease
-
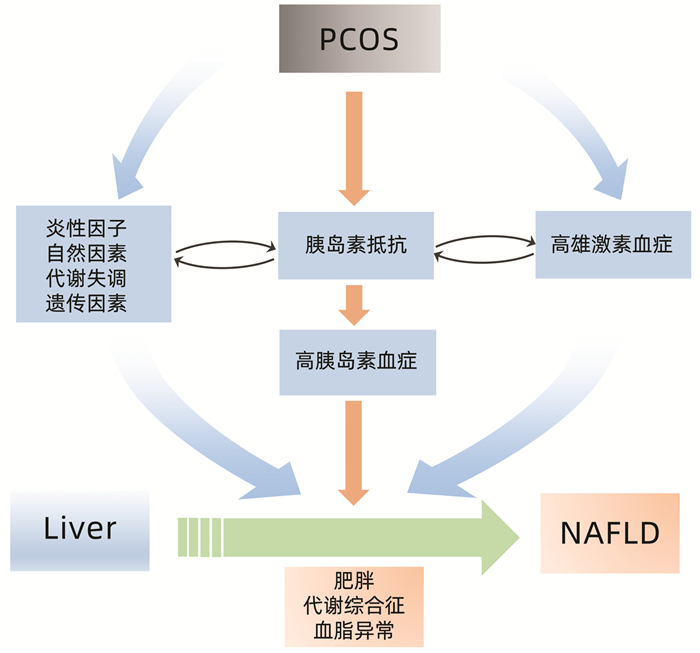
摘要: 多囊卵巢综合征(PCOS)是育龄妇女中最常见的内分泌疾病,临床常表现为月经稀发或闭经、高雄激素血症、排卵障碍性不孕等,可伴有肥胖、胰岛素抵抗、高胰岛素血症、糖脂代谢紊乱等代谢异常。PCOS人群常伴发非酒精性脂肪性肝病(NAFLD)等代谢相关性疾病,PCOS与NAFLD在发病机理及治疗上均有关联。本文总结了近年来PCO合并NAFLD相关研究进展。Abstract: Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of childbearing age, with the clinical manifestations of oligomenorrhea or amenorrhea, hyperandrogenism, and anovulatory infertility, and it is often accompanied by metabolic disorders such as obesity, insulin resistance, hyperinsulinemia, and glucose and lipid metabolism disorders. Women with PCOS often have nonalcoholic fatty liver disease (NAFLD) and other metabolic-associated diseases, and PCOS and NAFLD are related in terms of pathogenesis and treatment. This article reviews the research advances in PCOS with NAFLD in recent years.
-
[1] LI R, ZHANG Q, YANG D, et al. Prevalence of polycystic ovary syndrome in women in China: A large community-based study[J]. Hum Reprod, 2013, 28(9): 2562-2569. DOI: 10.1093/humrep/det262. [2] AZZIZ R, CARMINA E, CHEN Z, et al. Polycystic ovary syndrome[J]. Nat Rev Dis Primers, 2016, 2: 16057. DOI: 10.1038/nrdp.2016.57. [3] National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34(5): 947-957. DOI: 10.3969/j.issn.1001-5256.2018.05.007中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34(5): 947-957. DOI: 10.3969/j.issn.1001-5256.2018.05.007 [4] ZENG J, FAN JG. Clinical significance of renaming nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2020, 36(6): 1205-1207. DOI: 10.3969/j.issn.1001-5256.2020.06.002.曾静, 范建高. 非酒精性脂肪性肝病更名的临床意义[J]. 临床肝胆病杂志, 2020, 36(6): 1205-1207. DOI: 10.3969/j.issn.1001-5256.2020.06.002. [5] PASCHOU SA, POLYZOS SA, ANAGNOSTIS P, et al. Nonalcoholic fatty liver disease in women with polycystic ovary syndrome[J]. Endocrine, 2020, 67(1): 1-8. DOI: 10.1007/s12020-019-02085-7. [6] QU Z, ZHU Y, JIANG J, et al. The clinical characteristics and etiological study of nonalcoholic fatty liver disease in Chinese women with PCOS[J]. Iran J Reprod Med, 2013, 11(9): 725-732. [7] PETTA S, CIRESI A, BIANCO J, et al. Insulin resistance and hyperandrogenism drive steatosis and fibrosis risk in young females with PCOS[J]. PLoS One, 2017, 12(11): e0186136. DOI: 10.1371/journal.pone.0186136. [8] SARKAR M, TERRAULT N, CHAN W, et al. Polycystic ovary syndrome (PCOS) is associated with NASH severity and advanced fibrosis[J]. Liver Int, 2020, 40(2): 355-359. DOI: 10.1111/liv.14279. [9] BALLESTRI S, ZONA S, TARGHER G, et al. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis[J]. J Gastroenterol Hepatol, 2016, 31(5): 936-944. DOI: 10.1111/jgh.13264. [10] YOUNOSSI ZM, KOENIG AB, ABDELATIF D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes[J]. Hepatology, 2016, 64(1): 73-84. DOI: 10.1002/hep.28431. [11] SAKURAI Y, KUBOTA N, YAMAUCHI T, et al. Role of insulin resistance in MAFLD[J]. Int J Mol Sc, 2021, 22(8): 4156. DOI: 10.3390/ijms22084156. [12] LEGRO RS, CASTRACANE VD, KAUFFMAN RP. Detecting insulin resistance in polycystic ovary syndrome: Purposes and pitfalls[J]. Obstet Gynecol Surv, 2004, 59(2): 141-154. DOI: 10.1097/01.OGX.0000109523.25076.E2. [13] DIAMANTI-KANDARAKIS E, DUNAIF A. Insulin resistance and the polycystic ovary syndrome revisited: An update on mechanisms and implications[J]. Endocr Rev, 2012, 33(6): 981-1030. DOI: 10.1210/er.2011-1034. [14] QU X, DONNELLY R. Sex hormone-binding globulin (SHBG) as an early biomarker and therapeutic target in polycystic ovary syndrome[J]. Int J Mol Sci, 2020, 21(21): 8191. DOI: 10.3390/ijms21218191. [15] FENG C, JIN Z, CHI X, et al. SHBG expression is correlated with PI3K/AKT pathway activity in a cellular model of human insulin resistance[J]. Gynecol Endocrinol, 2018, 34(7): 567-573. DOI: 10.1080/09513590.2017.1411474. [16] SIMÓ R, SAEZ-LOPEZ C, LECUBE A, et al. Adiponectin upregulates SHBG production: Molecular mechanisms and potential implications[J]. Endocrinology, 2014, 155(8): 2820-2830. DOI: 10.1210/en.2014-1072. [17] SALVA-PASTOR N, CHÁVEZ-TAPIA NC, URIBE M, et al. Understanding the association of polycystic ovary syndrome and non-alcoholic fatty liver disease[J]. J Steroid Biochem Mol Biol, 2019, 194: 105445. DOI: 10.1016/j.jsbmb.2019.105445. [18] ROSENFIELD RL, EHRMANN DA. The pathogenesis of polycystic ovary syndrome (PCOS): The hypothesis of PCOS as functional ovarian hyperandrogenism revisited[J]. Endocr Rev, 2016, 37(5): 467-520. DOI: 10.1210/er.2015-1104. [19] QIAO PY, WANG XP, YANG SS, et al. Changes of sex hormones in patients with PCOS before and after treatment and their relationship with insulin resistance and obesity[J]. J Clin Exp Med, 2022, 21(1): 62-65. DOI: 10.3969/j.issn.1671-4695.2022.01.017.乔鹏艳, 王仙萍, 杨姗姗, 等. PCOS患者治疗前后性激素的变化及其与胰岛素抵抗、肥胖的关系[J]. 临床和实验医学杂志, 2022, 21(1): 62-65. DOI: 10.3969/j.issn.1671-4695.2022.01.017. [20] ROCHA A, FARIA LC, GUIMARÃES T, et al. Non-alcoholic fatty liver disease in women with polycystic ovary syndrome: Systematic review and meta-analysis[J]. J Endocrinol Invest, 2017, 40(12): 1279-1288. DOI: 10.1007/s40618-017-0708-9. [21] SARKAR M, TERRAULT N, CHAN W, et al. Polycystic ovary syndrome (PCOS) is associated with NASH severity and advanced fibrosis[J]. Liver Int, 2020, 40(2): 355-359. DOI: 10.1111/liv.14279. [22] LI T, ZHANG T, CUI T, et al. Involvement of endogenous testosterone in hepatic steatosis in women with polycystic ovarian syndrome[J]. J Steroid Biochem Mol Biol, 2020, 204: 105752. DOI: 10.1016/j.jsbmb.2020.105752. [23] ADEYANJU OA, FALODUN TO, MICHAEL OS, et al. Spironolactone reversed hepato-ovarian triglyceride accumulation caused by letrozole-induced polycystic ovarian syndrome: Tissue uric acid-a familiar foe[J]. Naunyn Schmiedebergs Arch Pharmacol, 2020, 393(6): 1055-1066. DOI: 10.1007/s00210-020-01809-1. [24] CUI P, HU W, MA T, et al. Long-term androgen excess induces insulin resistance and non-alcoholic fatty liver disease in PCOS-like rats[J]. J Steroid Biochem Mol Biol, 2021, 208: 105829. DOI: 10.1016/j.jsbmb.2021.105829. [25] SEIDU T, MCWHORTER P, MYER J, et al. DHT causes liver steatosis via transcriptional regulation of SCAP in normal weight female mice[J]. J Endocrinol, 2021, 250(2): 49-65. DOI: 10.1530/JOE-21-0040. [26] PASQUALI R, ORIOLO C. Obesity and androgens in women[J]. Front Horm Res, 2019, 53: 120-134. DOI: 10.1159/000494908. [27] OGUZ SH, I·DILMAN I, HELVACI N, et al. Tissue fat quantification by magnetic resonance imaging: Proton density fat fraction in polycystic ovary syndrome[J]. Reprod Biomed Online, 2020, 41(2): 329-334. DOI: 10.1016/j.rbmo.2020.04.024. [28] YE W, XIE T, SONG Y, et al. The role of androgen and its related signals in PCOS[J]. J Cell Mol Med, 2021, 25(4): 1825-1837. DOI: 10.1111/jcmm.16205. [29] YU JL, HOU LH, SUN M, et al. Difference analysis of clinical characteristics of polycystic ovary syndrome patients with different body mass index[J]. China Med Herald, 2020, 17(26): 75-78. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202026020.htm于婧璐, 侯丽辉, 孙淼, 等. 不同体重指数的多囊卵巢综合征患者的临床特征差异性分析[J]. 中国医药导报, 2020, 17(26): 75-78. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202026020.htm [30] Endocrine Study Group and Expert Group, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Chinese guidelines for the diagnosis and treatment of polycystic ovary syndrome[J]. Chin J Obstetr Gynecol, 2018, 53(1): 2-6. DOI: 10.3760/cma.j.issn.0529-567x.2018.01.002.中华医学会妇产科学分会内分泌学组及指南专家组. 多囊卵巢综合征中国诊疗指南[J]. 中华妇产科杂志, 2018, 53(1): 2-6. DOI: 10.3760/cma.j.issn.0529-567x.2018.01.002. [31] AYONRINDE OT, ODDY WH, ADAMS LA, et al. Infant nutrition and maternal obesity influence the risk of non-alcoholic fatty liver disease in adolescents[J]. J Hepatol, 2017, 67(3): 568-576. DOI: 10.1016/j.jhep.2017.03.029. [32] GANGALE MF, MIELE L, LANZONE A, et al. Long-term metformin treatment is able to reduce the prevalence of metabolic syndrome and its hepatic involvement in young hyperinsulinaemic overweight patients with polycystic ovarian syndrome[J]. Clin Endocrinol (Oxf), 2011, 75(4): 520-527. DOI: 10.1111/j.1365-2265.2011.04093.x. [33] TAN S, VOLLMAR N, BENSON S, et al. Liver injury indicating fatty liver but not serologic NASH marker improves under metformin treatment in polycystic ovary syndrome[J]. Int J Endocrinol, 2015, 2015: 254169. DOI: 10.1155/2015/254169. [34] IBÁÑEZ L, DEL RÍO L, DÍAZ M, et al. Normalizing ovulation rate by preferential reduction of hepato-visceral fat in adolescent girls with polycystic ovary syndrome[J]. J Adolesc Health, 2017, 61(4): 446-453. DOI: 10.1016/j.jadohealth.2017.04.010. [35] XU Y, WU Y, HUANG Q. Comparison of the effect between pioglitazone and metformin in treating patients with PCOS: A meta-analysis[J]. Arch Gynecol Obstet, 2017, 296(4): 661-677. DOI: 10.1007/s00404-017-4480-z. [36] VALSAMAKIS G, LOIS K, KUMAR S, et al. Metabolic and other effects of pioglit-azone as an add-on therapy to metformin in the treatment of polycystic ovary syndrome (PCOS)[J]. Hormones (Athens), 2013, 12(3): 363-78. DOI: 10.1007/BF03401302. [37] KAHAL H, ABOUDA G, RIGBY AS, et al. Glucagon-like peptide-1 analogue, liraglutide, improves liver fibrosis markers in obese women with polycystic ovary syndrome and nonalcoholic fatty liver disease[J]. Clin Endocrinol (Oxf), 2014, 81(4): 523-528. DOI: 10.1111/cen.12369. [38] FRØSSING S, NYLANDER M, CHABANOVA E, et al. Effect of liraglutide on ectopic fat in polycystic ovary syndrome: A randomized clinical trial[J]. Diabetes Obes Metab, 2018, 20(1): 215-218. DOI: 10.1111/dom.13053. [39] SIAMASHVILI M, DAVIS SN. Update on the effects of GLP-1 receptor agonists for the treatment of polycystic ovary syndrome[J]. Expert Rev Clin Pharmacol, 2021, 14(9): 1081-1089. DOI: 10.1080/17512433.2021.1933433. [40] NEWSOME PN, BUCHHOLTZ K, CUSI K, et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis[J]. N Engl J Med, 2021, 384(12): 1113-1124. DOI: 10.1056/NEJMoa2028395. [41] YARIBEYGI H, SATHYAPALAN T, MALEKI M, et al. Molecular mechanisms by which SGLT2 inhibitors can induce insulin sensitivity in diabetic milieu: A mechanistic review[J]. Life Sci, 2020, 240: 117090. DOI: 10.1016/j.lfs.2019.117090. [42] MANTOVANI A, BYRNE CD, SCORLETTI E, et al. Efficacy and safety of anti-hyperglycaemic drugs in patients with non-alcoholic fatty liver disease with or without diabetes: An updated systematic review of randomized controlled trials[J]. Diabetes Metab, 2020, 46(6): 427-441. DOI: 10.1016/j.diabet.2019.12.007. [43] SEKO Y, NISHIKAWA T, UMEMURA A, et al. Efficacy and safety of canagliflozin in type 2 diabetes mellitus patients with biopsy-proven nonalcoholic steatohepatitis classified as stage 1-3 fibrosis[J]. Diabetes Metab Syndr Obes, 2018, 11: 835-843. DOI: 10.2147/DMSO.S184767. [44] ITANI T, ISHIHARA T. Efficacy of canagliflozin against nonalcoholic fatty liver disease: A prospective cohort study[J]. Obes Sci Pract, 2018, 4(5): 477-482. DOI: 10.1002/osp4.294. [45] OLANIYI KS, ONIYIDE AA, ADEYANJU OA, et al. Low dose spironolactone-mediated androgen-adiponectin modulation alleviates endocrine-metabolic disturbances in letrozole-induced PCOS[J]. Toxicol Appl Pharmacol, 2021, 411: 115381. DOI: 10.1016/j.taap.2020.115381. [46] PANI A, GIOSSI R, MENICHELLI D, et al. Inositol and non-alcoholic fatty liver disease: A systematic review on deficiencies and supplementation[J]. Nutrients, 2020, 12(11). DOI: 10.3390/nu12113379. [47] GAN WJ, LI G. Ovulation induction in the treatment of patients with polycystic ovary syndrome[J]. Chin J Reproduct Contracept, 2019, (4): 322-324. DOI: 10.3760/cma.j.issn.2096-2916.2019.04.012.甘文锦, 李刚. 多囊卵巢综合征患者促排卵治疗的研究进展[J]. 中华生殖与避孕杂志, 2019, 39(4): 322-324. DOI: 10.3760/cma.j.issn.2096-2916.2019.04.012. [48] LEE E, LIM Y, KWON SW, et al. Pinitol consumption improves liver health status by reducing oxidative stress and fatty acid accumulation in subjects with non-alcoholic fatty liver disease: A randomized, double-blind, placebo-controlled trial[J]. J Nutr Biochem, 2019, 68: 33-41. DOI: 10.1016/j.jnutbio.2019.03.006. [49] KALYANARAMAN R, PAL L. A narrative review of current understanding of the pathophysiology of polycystic ovary syndrome: Focus on plausible relevance of vitamin D[J]. Int J Mol Sci, 2021, 22(9): 4905. DOI: 10.3390/ijms22094905. [50] AL-BAYYARI N, AL-DOMI H, ZAYED F, et al. Androgens and hirsutism score of overweight women with polycystic ovary syndrome improved after vitamin D treatment: A randomized placebo controlled clinical trial[J]. Clin Nutr, 2021, 40(3): 870-878. DOI: 10.1016/j.clnu.2020.09.024. [51] MENG J, ZHU Y. Efficacy of simvastatin plus metformin for polycystic ovary syndrome: A meta-analysis of randomized controlled trials[J]. Eur J Obstet Gynecol Reprod Biol, 2021, 257: 19-24. DOI: 10.1016/j.ejogrb.2020.11.070. [52] XIA Y, WANG Y, CUI M, et al. Efficacy of omega-3 fatty acid supplementation on cardiovascular risk factors in patients with polycystic ovary syndrome: A systematic review and meta-analysis[J]. Ann Palliat Med, 2021, 10(6): 6425-6437. DOI: 10.21037/apm-21-1050. [53] CLIMAX J, NEWSOME PN, HAMZA M, et al. Effects of epeleuton, a novel synthetic second-generation n-3 fatty acid, on non-alcoholic fatty liver disease, triglycerides, glycemic control, and cardiometabolic and inflammatory markers[J]. J Am Heart Assoc, 2020, 9(16): e016334. DOI: 10.1161/JAHA.119.016334. [54] CHUDZICKA-STRUGAŁA I, KUBIAK A, BANASZEWSKA B, et al. Effects of synbiotic supplementation and lifestyle modifications on women with polycystic ovary syndrome[J]. J Clin Endocrinol Metab, 2021, 106(9): 2566-2573. DOI: 10.1210/clinem/dgab369. [55] ARON-WISNEWSKY J, WARMBRUNN MV, NIEUWDORP M, et al. Nonalcoholic fatty liver disease: Modulating gut microbiota to improve severity?[J]. Gastroenterology, 2020, 158(7): 1881-1898. DOI: 10.1053/j.gastro.2020.01.049. -



 PDF下载 ( 2143 KB)
PDF下载 ( 2143 KB)

 下载:
下载:


