加速康复外科在胰十二指肠切除术围手术期应用有效性和安全性的系统评价与Meta分析
DOI: 10.3969/j.issn.1001-5256.2022.06.026
Efficacy and safety of enhanced recovery after surgery in the perioperative period of pancreaticoduodenectomy: A systematic review and Meta-analysis
-
摘要:
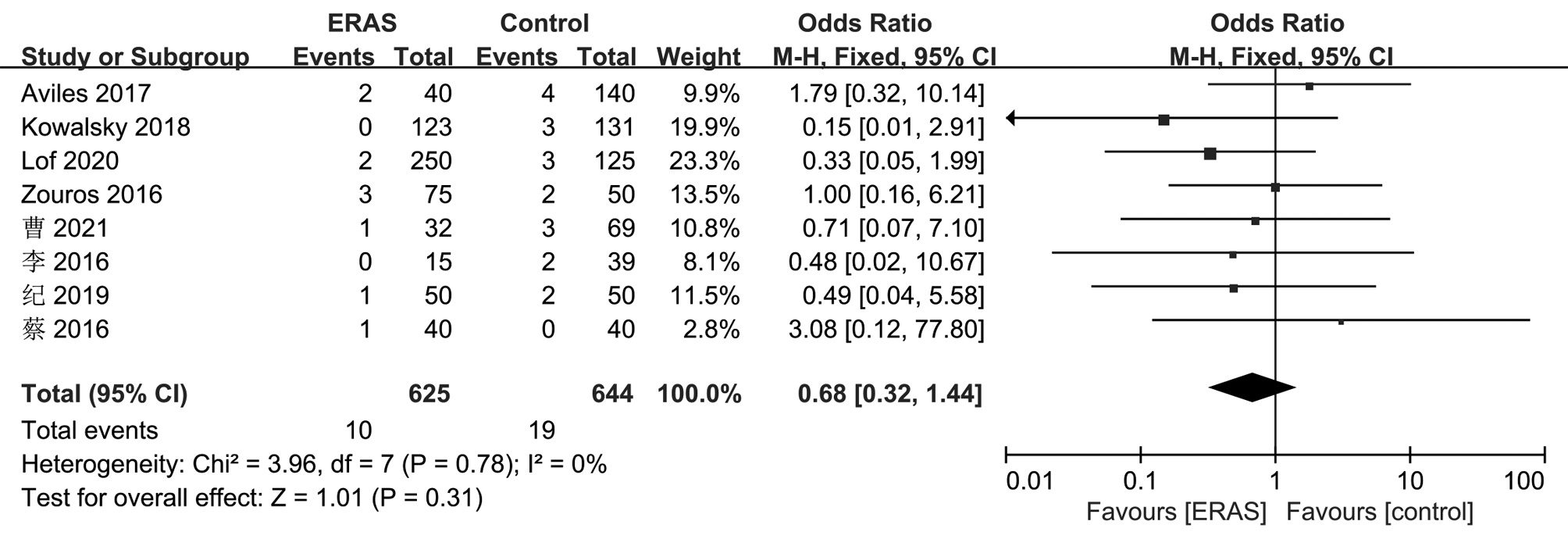
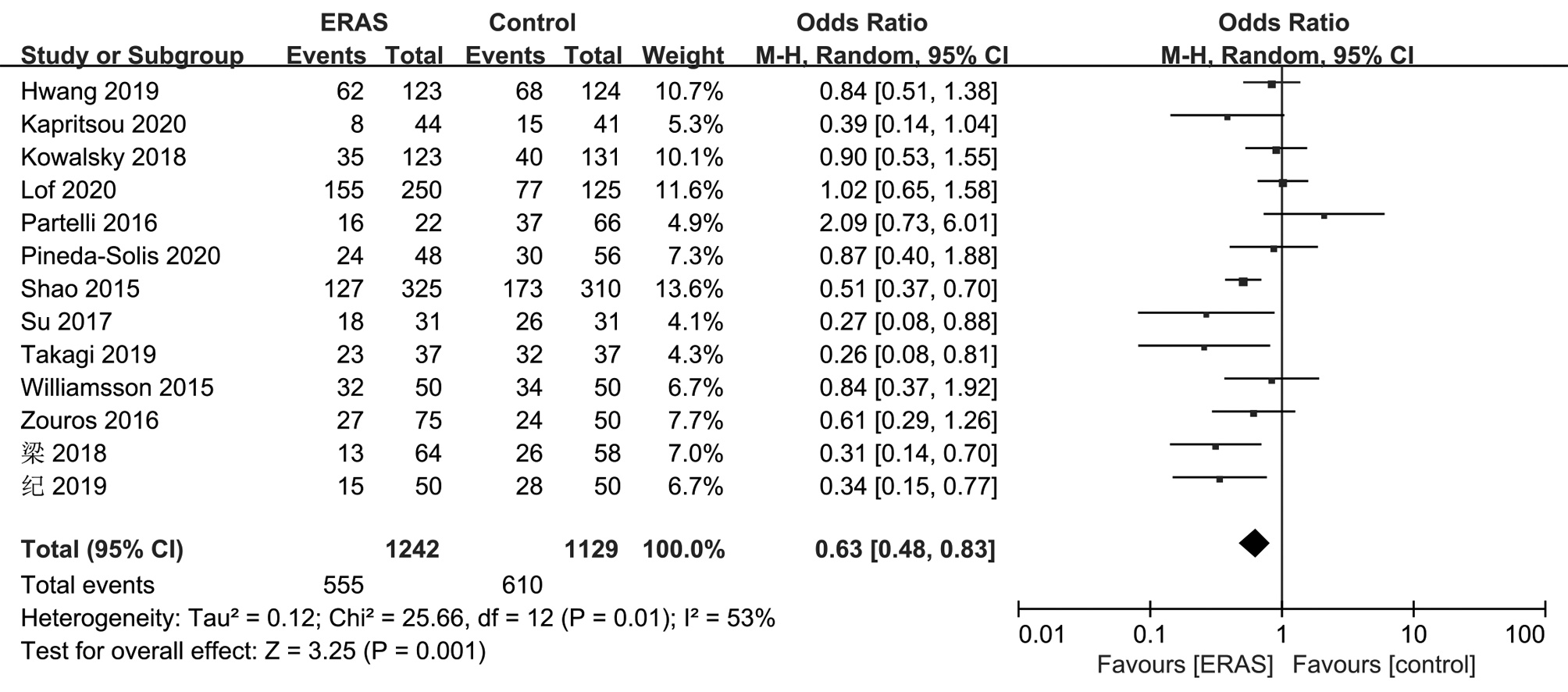
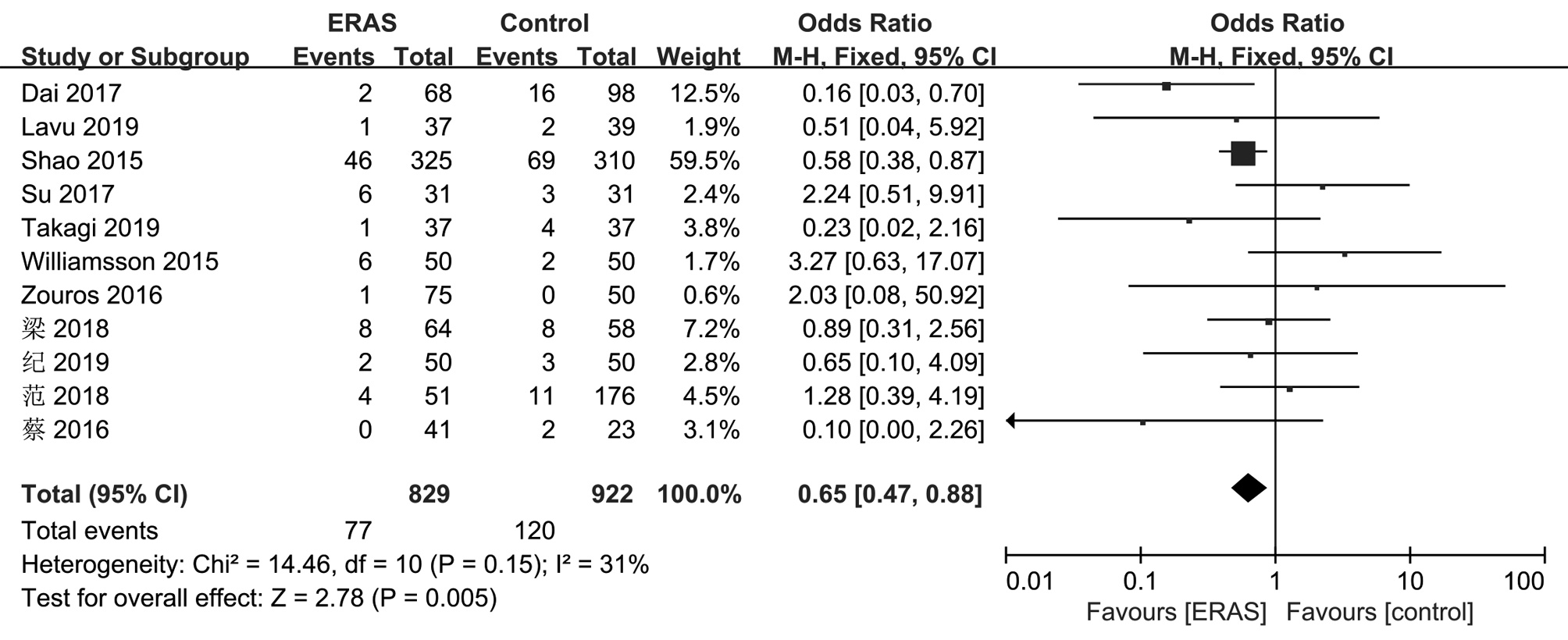
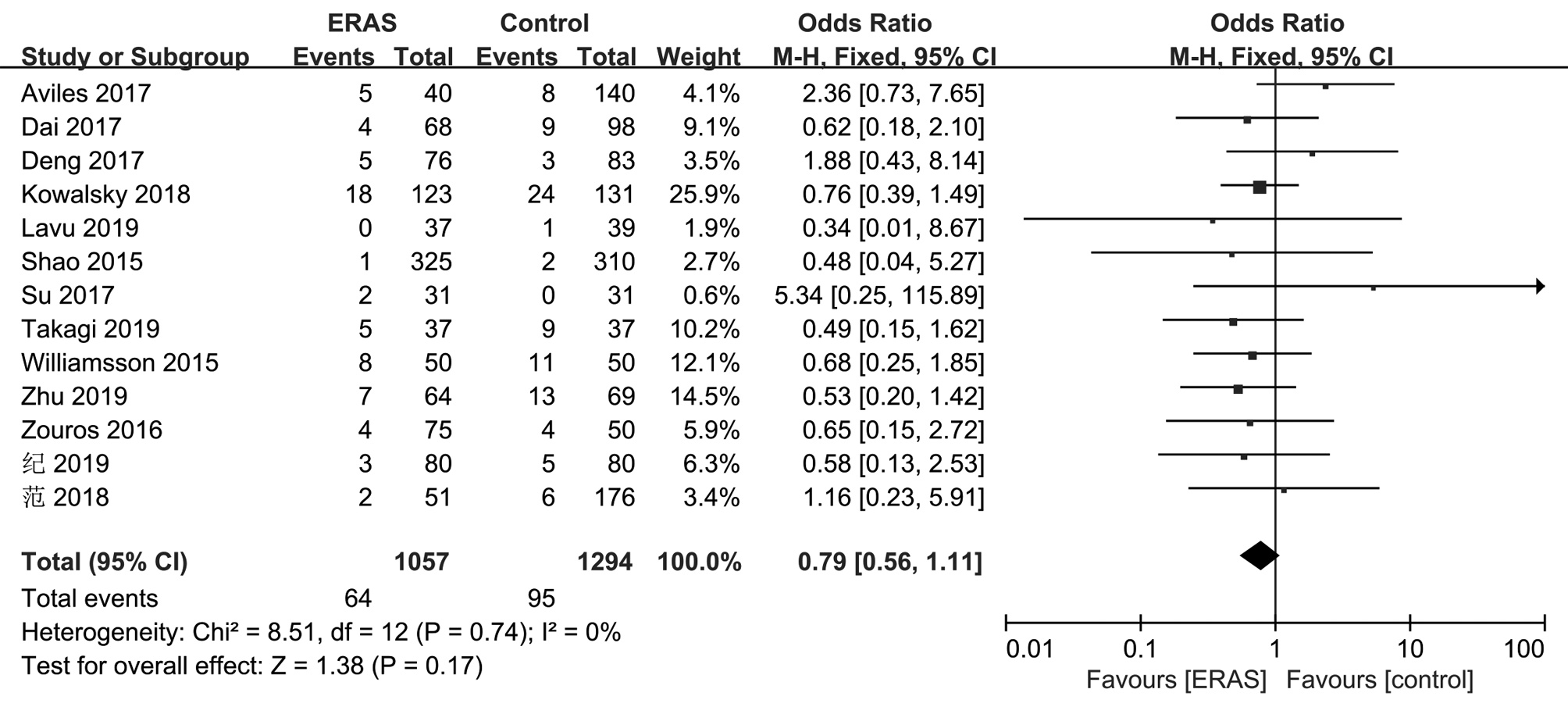
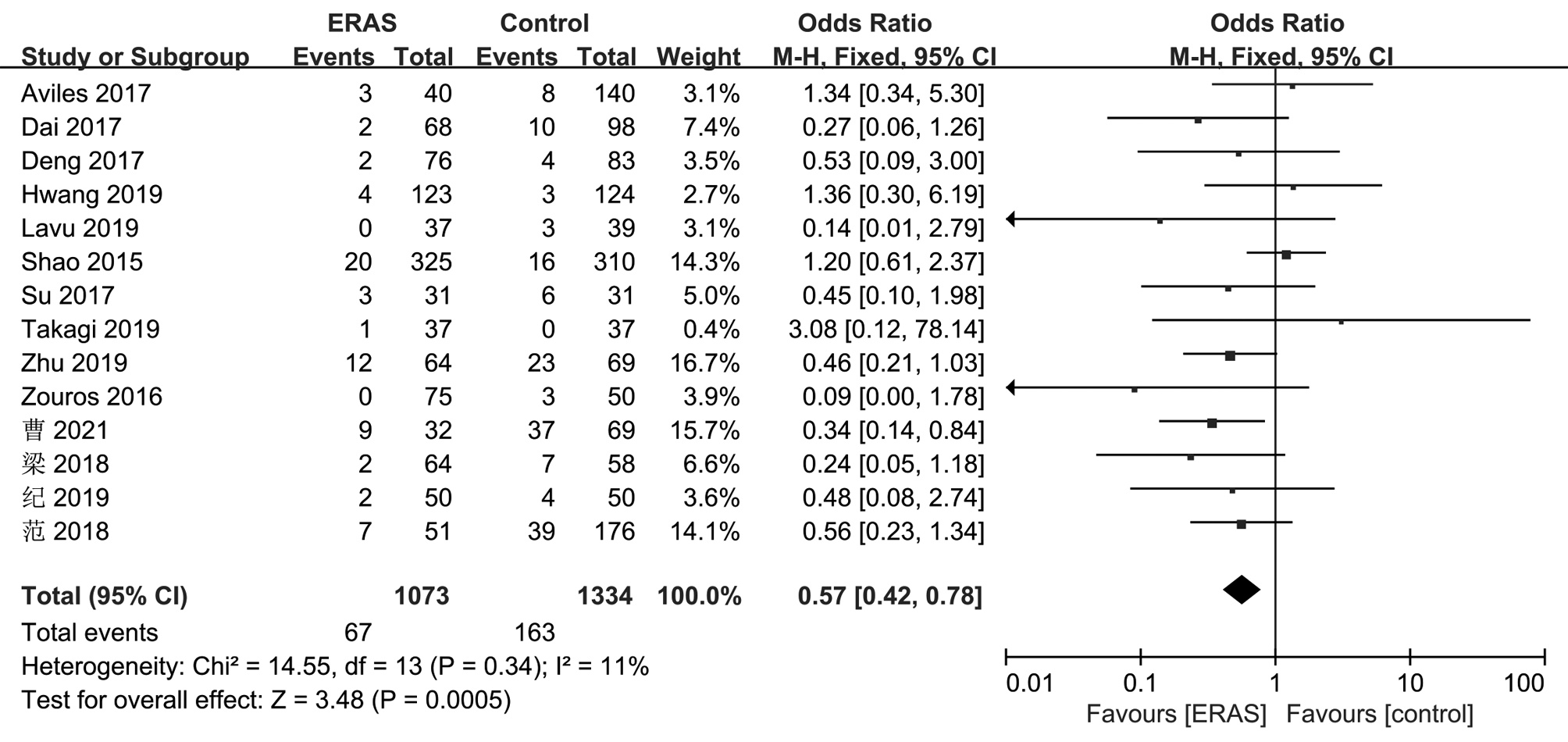
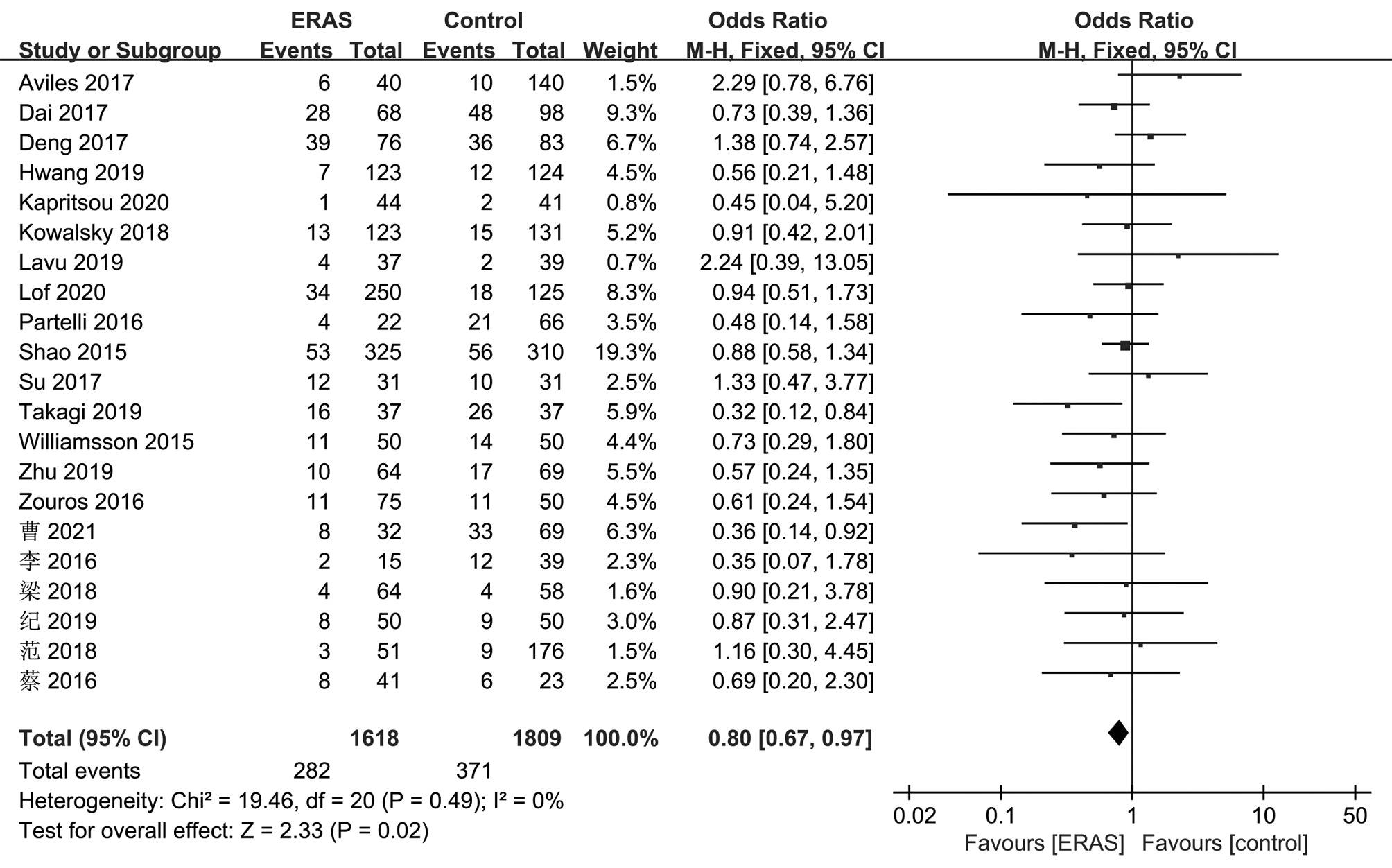
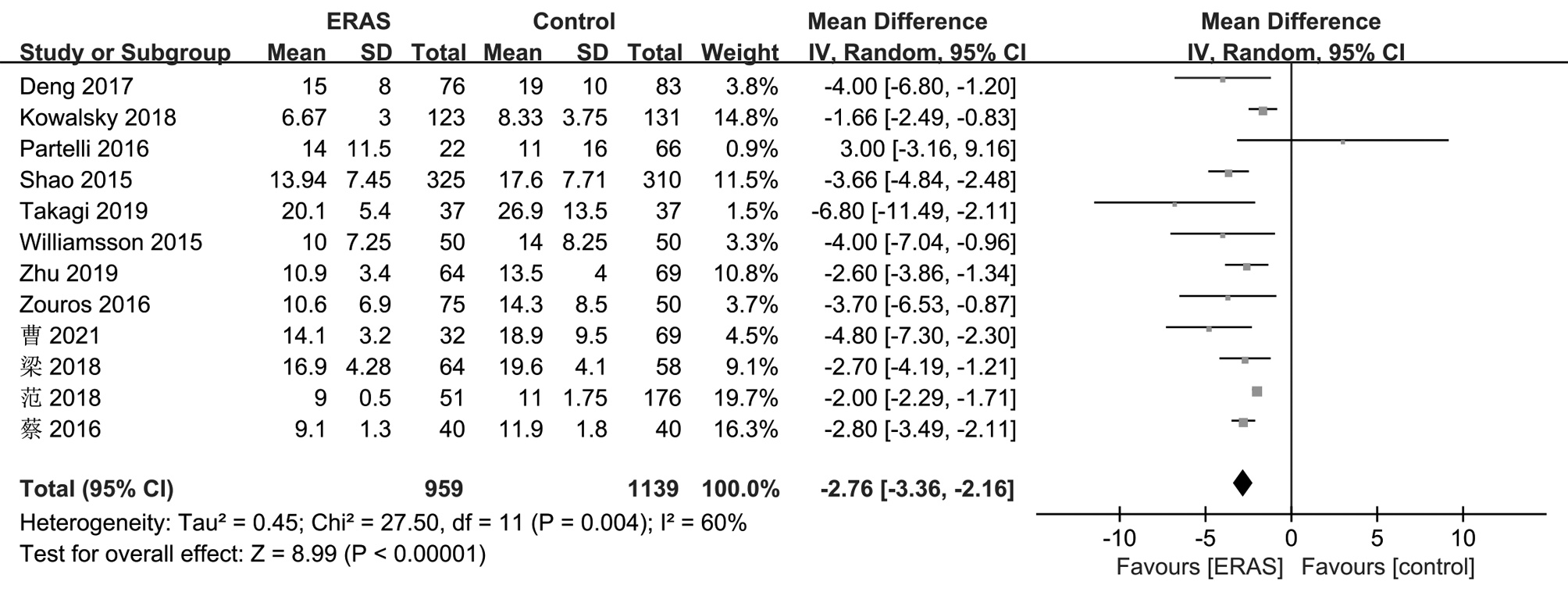
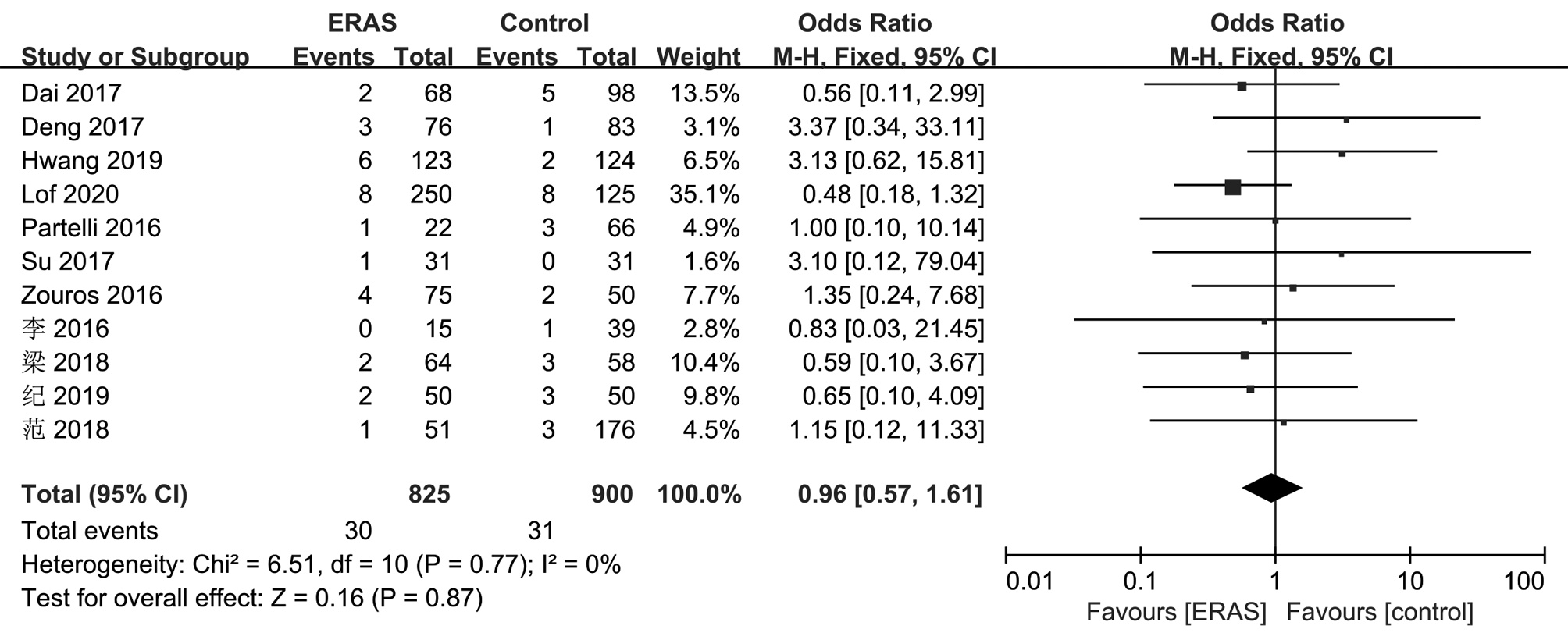
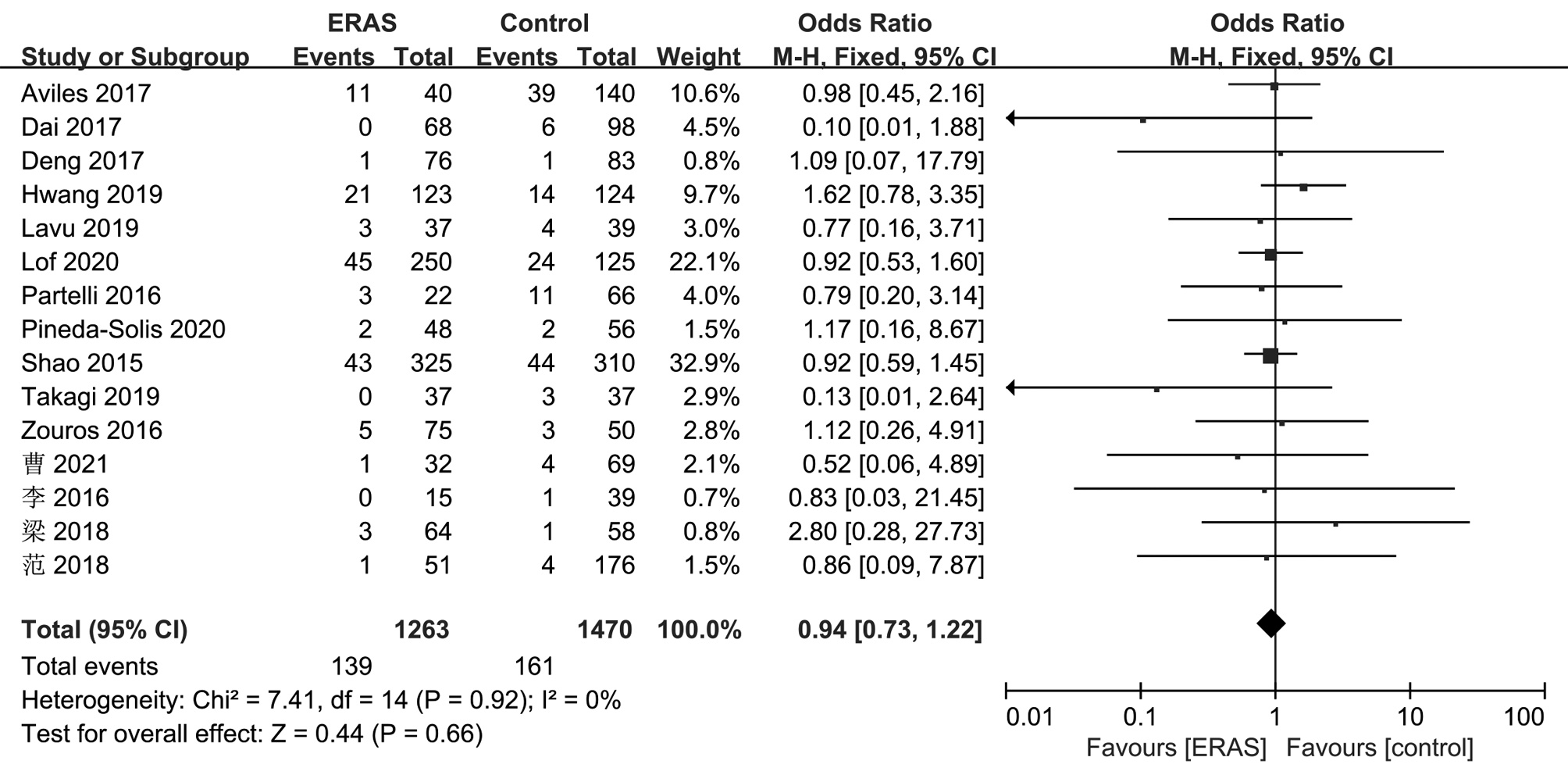
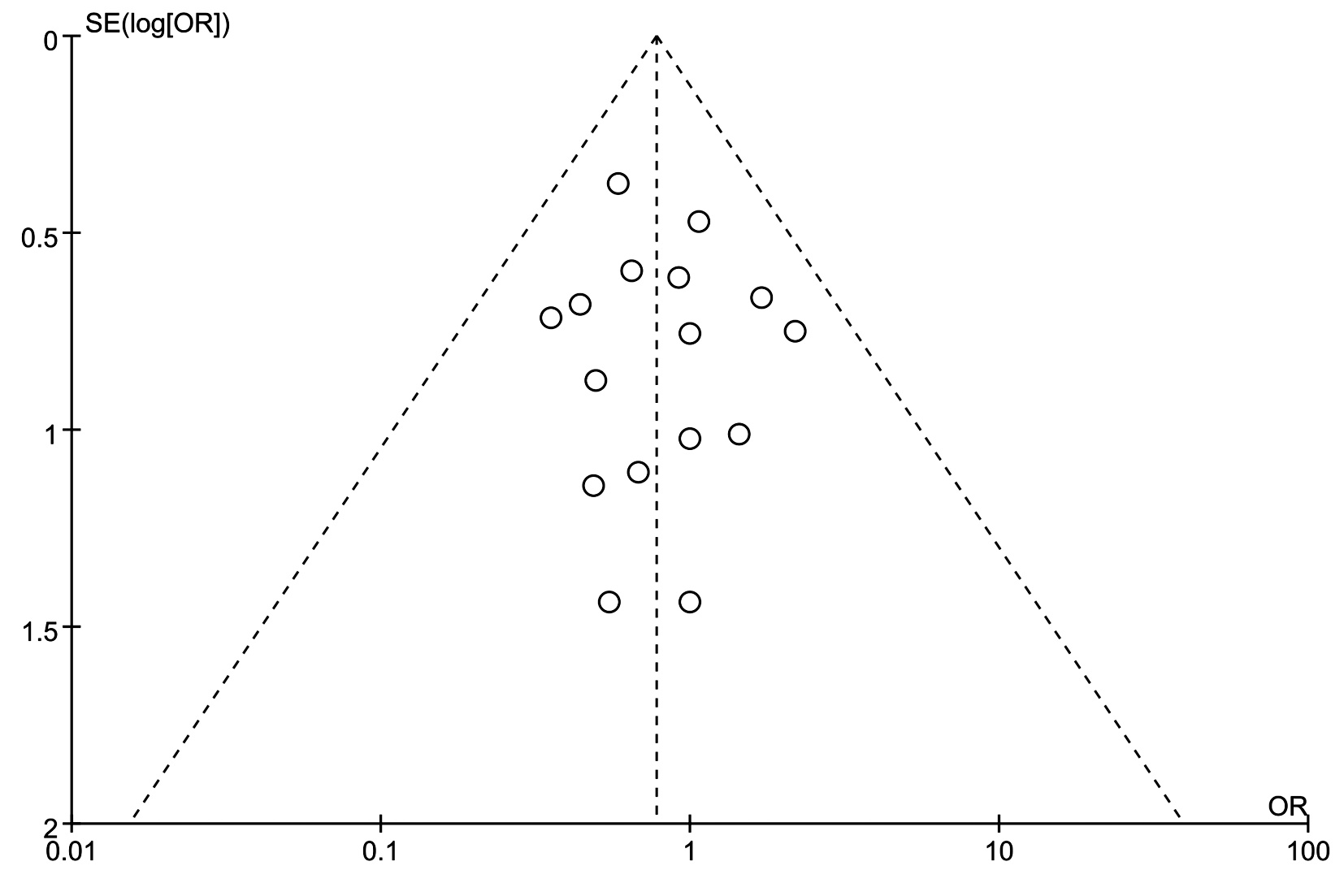
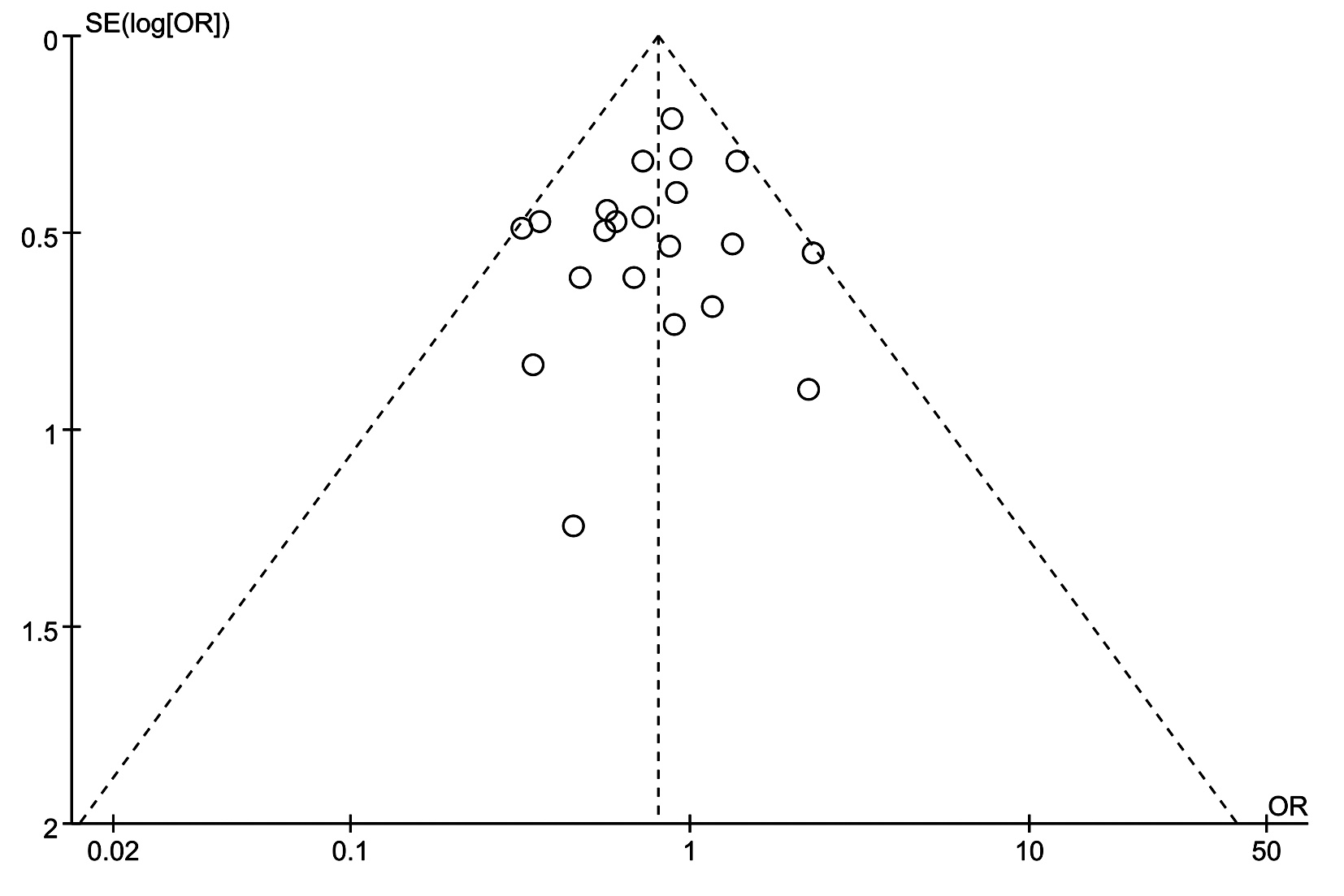
目的 系统评价加速康复外科(ERAS)在胰十二指肠切除术(PD)围手术期应用的有效性和安全性。 方法 检索中、英文数据库中有关ERAS应用于PD的临床对照研究,检索时间限定为2000年—2021年。对文献进行筛选、质量评价和数据提取,最后采用RevMan5.3软件进行Meta分析。本研究已在PROSPERO注册,注册号为: CRD42021287931。 结果 共纳入22项临床对照研究,包含3511例患者。结果显示,在PD围手术期实施ERAS,与传统术后管理相较,可减少患者总并发症(OR=0.63,95%CI:0.48~0.83,P=0.001)、腹腔感染(OR=0.65,95%CI:0.47~0.88,P=0.005)、肺部并发症(OR=0.57,95%CI:0.42~0.78,P=0.000 5)、胰漏(OR=0.80,95%CI:0.67~0.97,P=0.02)、胃排空障碍(OR=0.58,95%CI:0.48~0.71,P<0.001)的发生率,并可有效减少术后住院时间(MD=-2.76,95%CI:-3.36~-2.16,P<0.001),差异均有统计学意义。但在病死率、切口感染、术后出血率、再次手术和再次入院等方面,两组差异均无统计学意义(P值均>0.05)。 结论 ERAS应用于PD围手术期具有较好的有效性及安全性,可显著减少患者术后并发症的发生率和术后住院时间。 Abstract:Objective To investigate the efficacy and safety of enhanced recovery after surgery (ERAS) in the perioperative period of pancreaticoduodenectomy (PD). Methods Chinese and English databases were searched for controlled clinical trials on the application of ERAS in PD published from 2000 to 2021. Screening, quality assessment, and data extraction were performed for the articles, and RevMan5.3 software was used for meta-analysis. This study was registered on PROSPERO with a registration number of CRD42021287931. Results A total of 22 controlled clinical trials were included, with 3531 patients in total. The results showed that the implementation of ERAS in the perioperative period of PD reduced the incidence rates of total complications (odds ratio [OR]=0.63, 95% confidence interval [CI]: 0.48-0.83, P=0.001), abdominal infection (OR=0.65, 95% CI: 0.47-0.88, P=0.005), pulmonary complications (OR=0.57, 95% CI: 0.42-0.78, P=0.000 5), pancreatic leakage (OR=0.80, 95% CI: 0.67-0.97, P=0.02), and delayed gastric emptying (OR=0.58, 95% CI: 0.48-0.71, P < 0.001) and effectively shortened the length of postoperative hospital stay (mean difference=-2.76, 95% CI: -3.36 to -2.16, P < 0.001). However, there were no significant differences between the two groups in mortality rate, incision infection, postoperative bleeding rate, reoperation, and rehospitalization (all P > 0.05). Conclusion ERAS has good efficacy and safety in the perioperative period of PD and can significantly reduce the incidence rates of postoperative complications and shorten the length of postoperative hospital stay. Therefore, it holds promise for clinical application. -
Key words:
- Enhanced Recovery After Surgery /
- Pancreaticoduodenectomy /
- Meta-Analysis
-
表 1 纳入文献基本特征及质量评价
Table 1. Basic characteristics and quality evaluation of the included
作者 年份 国家 研究类型 例数 男/女
(例)年龄(岁)
(ERAS组/Control组)NOS/Jadad质量
评分(分)ERAS组 Control组 Aviles等[12] 2017 中国 RCS 40 140 98/82 58±13/57±12 9 Dai等[13] 2017 中国 RCS 68 98 85/81 58.5(18~69)/59.2(14~83) 8 Deng等[14] 2017 中国 RCT 76 83 92/67 54.5±12.7/51.3±15.0 5 Hwang等[15] 2019 韩国 RCT 123 124 153/94 63.3±9.2/62.9±9.2 4 Kapritsou等[16] 2020 希腊 RCT 44 41 52/33 60.5±11.7/64.8±11.9 6 Kowalsky等[17] 2019 美国 RCS 123 131 134/120 68.2±9.8/66.3±10.4 8 Lavu等[18] 2019 美国 RCT 37 39 38/38 65.8±9.6/65.0±9.3 6 Lof等[19] 2020 英国 RCS 250 125 214/161 65±10.9/66±9.7 8 Partelli等[20] 2016 意大利 RCS 22 66 47/41 77(75~82)/77.5(75~82) 7 Pineda-Solis等[21] 2020 美国 RCS 48 56 48/56 66.7±8.6/61.8±13.5 8 Shao等[22] 2015 中国 RCS 325 310 378/257 56.9±11.5/57±12 8 Su等[23] 2017 中国 RCS 31 31 37/25 62±9/61±11 8 Takagi等[24] 2019 日本 RCT 37 37 40/34 67.8±9.7/66.8±9.3 4 Williamsson等[25] 2015 瑞典 RCS 50 50 57/43 69(15~80)/67(25~81) 8 Zhu等[26] 2019 中国 RCS 64 69 59/74 64.3±7.9/64.1±11.5 8 Zouros等[27] 2016 希腊 RCS 75 50 80/45 65.9±10.5/63.9±11.6 9 曹昕彤等[28] 2021 中国 RCS 32 69 55/46 55(27~76)/56(38~81) 7 李向阳等[29] 2016 中国 RCS 15 39 36/18 52.7(41~71)/56.6(35~77) 8 梁琦等[30] 2018 中国 RCS 64 58 68/54 56.3±6.7/54.7±7.9 7 纪柏等[31] 2019 中国 RCS 50 50 48/52 57.0±14.2/59.3±15.3 8 范闻等[32] 2018 中国 RCS 51 176 130/97 56.8±1.6/58.2±0.9 8 蔡云强等[33] 2016 中国 RCS 41 23 38/26 54±5/52±6 8 注:RCS,回顾性临床研究。 -
[1] KEHLET H. Multimodal approach to control postoperative pathophysiology and rehabilitation[J]. Br J Anaesth, 1997, 78(5): 606-617. DOI: 10.1093/bja/78.5.606. [2] LJUNGQVIST O, SCOTT M, FEARON KC. Enhanced recovery after surgery: A review[J]. JAMA Surg, 2017, 152(3): 292-298. DOI: 10.1001/jamasurg.2016.4952. [3] BASSE L, RASKOV HH, HJORT JAKOBSEN D, et al. Accelerated postoperative recovery programme after colonic resection improves physical performance, pulmonary function and body composition[J]. Br J Surg, 2002, 89(4): 446-453. DOI: 10.1046/j.0007-1323.2001.02044.x. [4] DORCARATTO D, GRANDE L, PERA M. Enhanced recovery in gastrointestinal surgery: Upper gastrointestinal surgery[J]. Dig Surg, 2013, 30(1): 70-78. DOI: 10.1159/000350701. [5] MALVIYA A, MARTIN K, HARPER I, et al. Enhanced recovery program for hip and knee replacement reduces death rate[J]. Acta Orthop, 2011, 82(5): 577-581. DOI: 10.3109/17453674.2011.618911. [6] de GROOT JJ, van ES LE, MAESSEN JM, et al. Diffusion of enhanced recovery principles in gynecologic oncology surgery: Is active implementation still necessary?[J]. Gynecol Oncol, 2014, 134(3): 570-575. DOI: 10.1016/j.ygyno.2014.06.019. [7] SCHNELLDORFER T, WARE AL, SARR MG, et al. Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: Is cure possible?[J]. Ann Surg, 2008, 247(3): 456-462. DOI: 10.1097/SLA.0b013e3181613142. [8] DEOLIVEIRA ML, WINTER JM, SCHAFER M, et al. Assessment of complications after pancreatic surgery: A novel grading system applied to 633 patients undergoing pancreaticoduodenectomy[J]. Ann Surg, 2006, 244(6): 931-937; discussion 937-939. DOI: 10.1097/01.sla.0000246856.03918.9a. [9] de WILDE RF, BESSELINK MG, van der TWEEL I, et al. Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality[J]. Br J Surg, 2012, 99(3): 404-410. DOI: 10.1002/bjs.8664. [10] JADAD AR, MOORE RA, CARROLL D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary?[J]. Control Clin Trials, 1996, 17(1): 1-12. DOI: 10.1016/0197-2456(95)00134-4. [11] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25(9): 603-605. DOI: 10.1007/s10654-010-9491-z. [12] AVILES C, HOCKENBERRY M, VROCHIDES D, et al. Perioperative care implementation: Evidence-based practice for patients with pancreaticoduodenectomy using the enhanced recovery after surgery guidelines[J]. Clin J Oncol Nurs, 2017, 21(4): 466-472. DOI: 10.1188/17.CJON.466-472. [13] DAI J, JIANG Y, FU D. Reducing postoperative complications and improving clinical outcome: Enhanced recovery after surgery in pancreaticoduodenectomy—A retrospective cohort study[J]. Int J Surg, 2017, 39: 176-181. DOI: 10.1016/j.ijsu.2017.01.089. [14] DENG X, CHENG X, HUO Z, et al. Modified protocol for enhanced recovery after surgery is beneficial for Chinese cancer patients undergoing pancreaticoduodenectomy[J]. Oncotarget, 2017, 8(29): 47841-47848. DOI: 10.18632/oncotarget.18092. [15] HWANG DW, KIM HJ, LEE JH, et al. Effect of enhanced recovery after surgery program on pancreaticoduodenectomy: A randomized controlled trial[J]. J Hepatobiliary Pancreat Sci, 2019, 26(8): 360-369. DOI: 10.1002/jhbp.641. [16] KAPRITSOU M, PAPATHANASSOGLOU ED, KONSTANTINOU EA, et al. Effects of the enhanced recovery program on the recovery and stress response in patients with cancer undergoing pancreatoduodenectomy[J]. Gastroenterol Nurs, 2020, 43(2): 146-155. DOI: 10.1097/SGA.0000000000000417. [17] KOWALSKY SJ, ZENATI MS, STEVE J, et al. A Combination of robotic approach and ERAS pathway optimizes outcomes and cost for pancreatoduodenectomy[J]. Ann Surg, 2019, 269(6): 1138-1145. DOI: 10.1097/SLA.0000000000002707. [18] LAVU H, MCCALL NS, WINTER JM, et al. Enhancing patient outcomes while containing costs after complex abdominal operation: A randomized controlled trial of the whipple accelerated recovery pathway[J]. J Am Coll Surg, 2019, 228(4): 415-424. DOI: 10.1016/j.jamcollsurg.2018.12.032. [19] LOF S, BENEDETTI CACCIAGUERRA A, ALJARRAH R, et al. Implementation of enhanced recovery after surgery for pancreatoduodenectomy increases the proportion of patients achieving textbook outcome: A retrospective cohort study[J]. Pancreatology, 2020, 20(5): 976-983. DOI: 10.1016/j.pan.2020.05.018. [20] PARTELLI S, CRIPPA S, CASTAGNANI R, et al. Evaluation of an enhanced recovery protocol after pancreaticoduodenectomy in elderly patients[J]. HPB (Oxford), 2016, 18(2): 153-158. DOI: 10.1016/j.hpb.2015.09.009. [21] PINEDA-SOLIS K, BURCHARD PR, RUFFOLO LI, et al. Early prediction of length of stay after pancreaticoduodenectomy[J]. J Surg Res, 2021, 260: 499-505. DOI: 10.1016/j.jss.2020.11.060. [22] SHAO Z, JIN G, JI W, et al. The role of fast-track surgery in pancreaticoduodenectomy: A retrospective cohort study of 635 consecutive resections[J]. Int J Surg, 2015, 15: 129-133. DOI: 10.1016/j.ijsu.2015.01.007. [23] SU W, LU F, ZHANG X, et al. A hospital-to-home evaluation of an enhanced recovery protocol for elective pancreaticoduodenectomy in China: A cohort study[J]. Medicine (Baltimore), 2017, 96(41): e8206. DOI: 10.1097/MD.0000000000008206. [24] TAKAGI K, YOSHIDA R, YAGI T, et al. Effect of an enhanced recovery after surgery protocol in patients undergoing pancreaticoduodenectomy: A randomized controlled trial[J]. Clin Nutr, 2019, 38(1): 174-181. DOI: 10.1016/j.clnu.2018.01.002. [25] WILLIAMSSON C, KARLSSON N, STURESSON C, et al. Impact of a fast-track surgery programme for pancreaticoduodenectomy[J]. Br J Surg, 2015, 102(9): 1133-1141. DOI: 10.1002/bjs.9856. [26] ZHU J, LI X, LI H, et al. Enhanced recovery after surgery pathways benefit patients with soft pancreatic texture following pancreaticoduodenectomy[J]. Am J Surg, 2020, 219(6): 1019-1023. DOI: 10.1016/j.amjsurg.2019.08.002. [27] ZOUROS E, LIAKAKOS T, MACHAIRAS A, et al. Improvement of gastric emptying by enhanced recovery after pancreaticoduodenectomy[J]. Hepatobiliary Pancreat Dis Int, 2016, 15(2): 198-208. DOI: 10.1016/s1499-3872(16)60061-9. [28] CAO XT, NING CH, LI JR et al. Application value of enhanced recovery after surgery in perioperative management of pancreaticoduodenectomy[J]. Chin J Gen Surg, 2021, 30(3): 305-312. DOI: 10.7659/j.issn.1005-6947.2021.03.008.曹昕彤, 宁彩虹, 李嘉荣, 等. 快速康复外科在胰十二指肠切除术围术期管理中的应用价值[J]. 中国普通外科杂志, 2021, 30(3): 305-312. DOI: 10.7659/j.issn.1005-6947.2021.03.008. [29] LI XY, ZHAO X, ZHENG P, et al. Application of enhanced recovery after surgery in patients with duodenopancreatectomy[J]. J Hepatopancreatobiliary Surg, 2016, 28(6): 460-464. DOI: 10.11952/j.issn.1007-1954.2016.06.004.李向阳, 赵鑫, 郑鹏, 等. 加速康复外科在胰十二指肠切除术中的应用[J]. 肝胆胰外科杂志, 2016, 28(6): 460-464. DOI: 10.11952/j.issn.1007-1954.2016.06.004. [30] LIANG Q. The value of application of enhanced recovery after surgery in the perioperative of pancreatoduodenectomy[D]. Lanzhou: Lanzhou University, 2018.梁琦. 快速康复外科在胰十二指肠切除术围术期中的应用价值[D]. 兰州: 兰州大学, 2018. [31] JI B, LIU SY, ZHANG W, et al. Clinical effect of the enhanced recovery after surgery strategy for pancreaticoduodenectomy[J]. J Clin Hepatol, 2019, 35(5): 1032-1036. DOI: 10.3969/j.issn.1001-5256.2019.05.019.纪柏, 刘松阳, 张威, 等. 加速康复外科在胰十二指肠切除术中的应用效果分析[J]. 临床肝胆病杂志, 2019, 35(5): 1032-1036. DOI: 10.3969/j.issn.1001-5256.2019.05.019. [32] FAN W, TIAN BL. Application of multi-subjects and multi-modes intervention in the enhanced recovery after pancreaticoduodenectomy[J]. Chin J Bases Clin Gen Surg, 2018, 25(6): 695-701. DOI: 10.7507/1007-9424.201710048.范闻, 田伯乐. 多学科多模式干预在胰十二指肠切除术后快速康复中的应用[J]. 中国普外基础与临床杂志, 2018, 25(6): 695-701. DOI: 10.7507/1007-9424.201710048. [33] CAI YQ, XIA QH, GAO P, et al. Application value of enhanced recovery after surgery in laparoscopic pancreaticoduodenectomy[J]. Chin J Dig Surg, 2016, 15(6): 552-556. DOI: 10.3760/cma.j.issn.1673-9752.2016.06.007.蔡云强, 夏青红, 高攀, 等. 加速康复外科在腹腔镜胰十二指肠切除术中的应用价值[J]. 中华消化外科杂志, 2016, 15(6): 552-556. DOI: 10.3760/cma.j.issn.1673-9752.2016.06.007. [34] GOOIKER GA, LEMMENS VE, BESSELINK MG, et al. Impact of centralization of pancreatic cancer surgery on resection rates and survival[J]. Br J Surg, 2014, 101(8): 1000-1005. DOI: 10.1002/bjs.9468. [35] PASSERI MJ, BAKER EH, SIDDIQUI IA, et al. Total compared with partial pancreatectomy for pancreatic adenocarcinoma: assessment of resection margin, readmission rate, and survival from the U.S. National Cancer Database[J]. Curr Oncol, 2019, 26(3): e346-346e356. DOI: 10.3747/co.26.4066. [36] MCEVOY SH, LAVELLE LP, HOARE SM, et al. Pancreaticoduodenectomy: expected post-operative anatomy and complications[J]. Br J Radiol, 2014, 87(1041): 20140050. DOI: 10.1259/bjr.20140050. [37] WILMORE DW, KEHLET H. Management of patients in fast track surgery[J]. BMJ, 2001, 322(7284): 473-476. DOI: 10.1136/bmj.322.7284.473. [38] MAHENDRAN R, TEWARI M, DIXIT VK, et al. Enhanced recovery after surgery protocol enhances early postoperative recovery after pancreaticoduodenectomy[J]. Hepatobiliary Pancreat Dis Int, 2019, 18(2): 188-193. DOI: 10.1016/j.hbpd.2018.12.005. [39] YERMILOV I, JAIN S, SEKERIS E, et al. Utilization of parenteral nutrition following pancreaticoduodenectomy: Is routine jejunostomy tube placement warranted?[J]. Dig Dis Sci, 2009, 54(7): 1582-1588. DOI: 10.1007/s10620-008-0526-1. [40] HERMSEN JL, SANO Y, KUDSK KA. Food fight! Parenteral nutrition, enteral stimulation and gut-derived mucosal immunity[J]. Langenbecks Arch Surg, 2009, 394(1): 17-30. DOI: 10.1007/s00423-008-0339-x. [41] GIANOTTI L, NESPOLI L, TORSELLI L, et al. Safety, feasibility, and tolerance of early oral feeding after colorectal resection outside an enhanced recovery after surgery (ERAS) program[J]. Int J Colorectal Dis, 2011, 26(6): 747-753. DOI: 10.1007/s00384-011-1138-3. [42] YIP VS, DUNNE DF, SAMUELS S, et al. Adherence to early mobilisation: Key for successful enhanced recovery after liver resection[J]. Eur J Surg Oncol, 2016, 42(10): 1561-1567. DOI: 10.1016/j.ejso.2016.07.015. [43] NELSON R, EDWARDS S, TSE B. Prophylactic nasogastric decompression after abdominal surgery[J]. Cochrane Database Syst Rev, 2007, 3: CD004929. DOI: 10.1002/14651858.CD004929.pub3. [44] ERAS Compliance Group. The impact of enhanced recovery protocol compliance on elective colorectal cancer resection: Results from an international registry[J]. Ann Surg, 2015, 261(6): 1153-1159. DOI: 10.1097/SLA.0000000000001029. [45] COOLSEN MM, van DAM RM, van der WILT AA, et al. Systematic review and meta-analysis of enhanced recovery after pancreatic surgery with particular emphasis on pancreaticoduodenectomies[J]. World J Surg, 2013, 37(8): 1909-1918. DOI: 10.1007/s00268-013-2044-3. 期刊类型引用(5)
1. 王耀磊,王盼攀. 肝门部胆管癌患者术后并发症发生情况及其影响因素的Logistic回归分析. 医学理论与实践. 2024(11): 1822-1825 .  百度学术
百度学术2. 李明,于群,肖熙,刘影倩,黄裕存. 外科Apgar评分及POSSUM评分对老年严重胸部外伤术后预后的评估价值. 名医. 2023(09): 30-32 .  百度学术
百度学术3. 朱磊,赵海淳,李珊珊,孟君. 外科Apgar评分对术前新辅助化疗进展期胃癌术后并发症的预测价值. 中国现代普通外科进展. 2022(12): 990-993 .  百度学术
百度学术4. 章周海,涂从银. 肝门部胆管癌的手术疗效分析. 肝胆外科杂志. 2021(03): 223-225 .  百度学术
百度学术5. 遆军锋,温陈,张小云,姜丹丹. 肝门部胆管癌术后并发症发生危险因素及术前外科改良 Apgar评分、血清总胆红素水平对并发症的预测价值. 陕西医学杂志. 2021(12): 1513-1516 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 3967 KB)
PDF下载 ( 3967 KB)


 下载:
下载:


 百度学术
百度学术

