LPRI评分在乙型肝炎肝纤维化及肝硬化中的诊断价值
DOI: 10.3969/j.issn.1001-5256.2022.07.014
Application value of liver stiffness measurement-to-platelet ratio index score in diagnosis of hepatitis B liver fibrosis and liver cirrhosis
-
摘要:
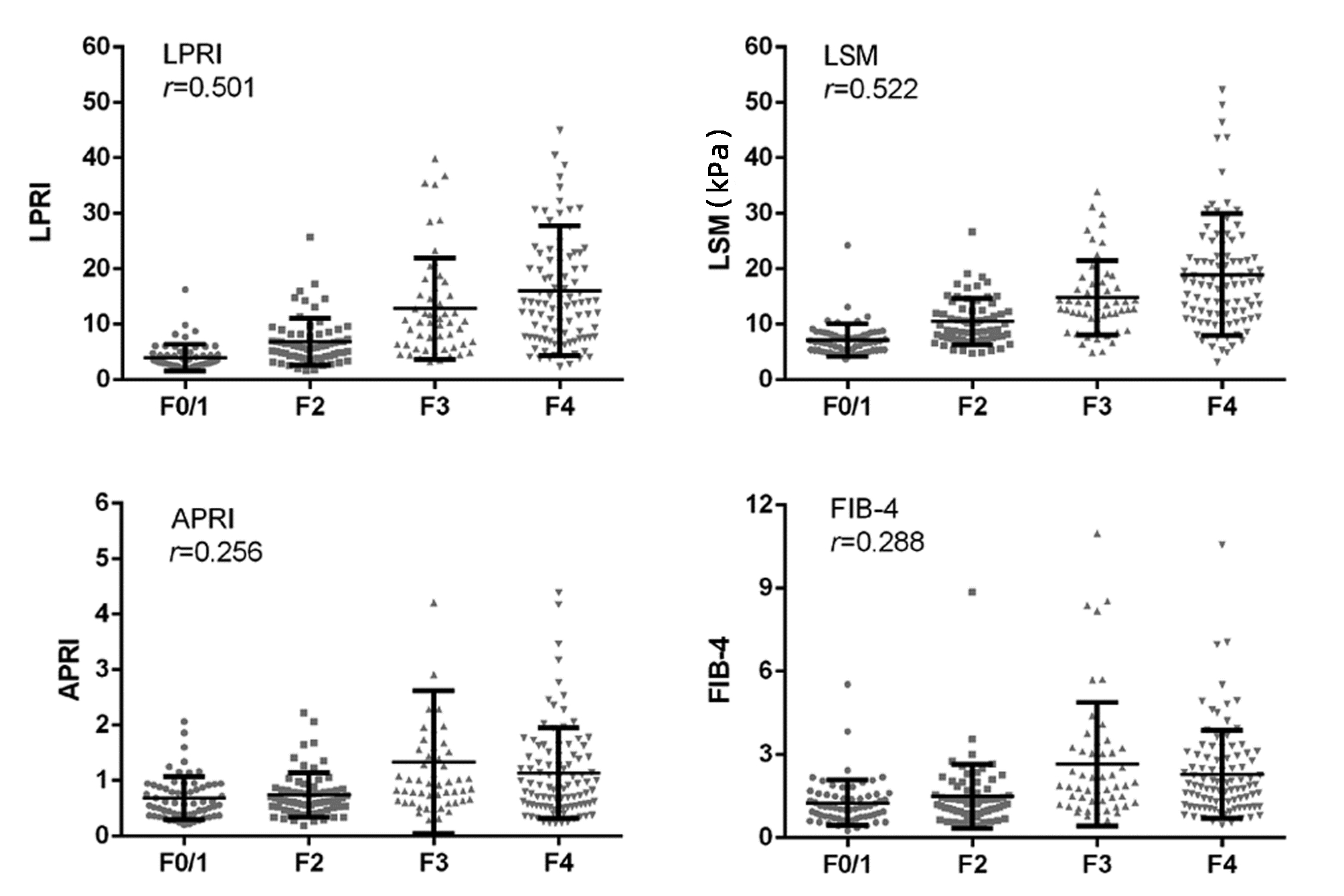
目的 肝纤维化程度的评估对于指导慢性乙型肝炎患者治疗及预测预后具有重要意义,本研究旨在评价LPRI评分对乙型肝炎肝纤维化/肝硬化初治人群的诊断价值。 方法 筛选首都医科大学附属北京友谊医院既往乙型肝炎研究队列2013年6月—2015年9月经肝穿刺确诊的慢性乙型肝炎患者276例。基于患者肝脏硬度测定(LSM)联合PLT计算LPRI评分,以肝脏病理为金标准,评价LPRI评分对于乙型肝炎肝纤维化及肝硬化的诊断价值。不符合正态分布计量资料多组间比较采用Kruskal-Wallis H秩和检验,计数资料组间比较采用χ2检验。各诊断模型与肝穿病理的相关性分析采用Spearman相关分析;通过DeLong法比较多个无创诊断模型(LPRI、LSM、APRI、FIB-4)的受试者工作特征曲线下面积(AUC)及诊断性能。采用Bootstrap方法对LPRI肝纤维化/肝硬化的诊断价值进行内部验证。 结果 根据肝纤维化程度的不同,分为F0/1组(n=63)、F2/3组(n=118)、F4组(n=95),3组间Alb、TBil、PLT、LSM、AFP及HBV DNA水平均具有统计学差异(P值均<0.05)。LPRI评分与肝穿病理有较好的相关性(r=0.501,P<0.001);对乙型肝炎显著性肝纤维化(AUC=0.88, 95%CI: 0.83~0.91)的诊断性能优于肝硬化(AUC=0.79, 95%CI: 0.73~0.83)。相比APRI评分和FIB-4指数,LPRI的诊断性能更好(P值均<0.05);与LSM联合后,LPRI评分能进一步补充LSM对肝硬化诊断的灵敏度(53%提高至82%)。经约登指数推荐的诊断显著性肝纤维化和肝硬化的LPRI评分界值分别为6.1(灵敏度71%,特异度92%)和6.9(灵敏度81%,特异度66%)。 结论 LPRI评分作为一种简易方便的肝纤维化无创诊断指数,在慢性乙型肝炎患者肝纤维化/肝硬化的诊断和分期中有一定的应用价值。 Abstract:Objective To investigate the diagnostic value of liver stiffness measurement-to-platelet ratio index (LPRI) score in previously untreated patients with hepatitis B liver fibrosis/liver cirrhosis, since the evaluation of liver fibrosis degree has great significance in guiding the treatment of chronic hepatitis B patients and predicting their prognosis. Methods A total of 276 chronic hepatitis B patients who were diagnosed by liver biopsy from June 2013 to September 2015 were selected from the hepatitis B study cohort of Beijing Friendship Hospital, Capital Medical University. LPRI score was calculated based on liver stiffness measurement (LSM) and platelet, and the value of LPRI score in the diagnosis of liver fibrosis and liver cirrhosis in hepatitis B patients was evaluated with liver pathology as the gold standard. The Kruskal-Wallis H test was used for comparison of non-normally distributed continuous data between multiple groups, and the chi-square test was used for comparison of categorical data between groups. A Spearman correlation analysis was used to investigate the correlation between each diagnostic model and liver biopsy, and the DeLong test was used to compare the area under the ROC curve (AUC) and diagnostic performance of several noninvasive diagnostic models, i.e., LPRI, LSM, aspartate aminotransferase-to-platelet ratio index (APRI), and fibrosis-4 (FIB-4). The Bootstrap method was used for the internal validation of the value of LPRI score in the diagnosis of liver fibrosis/cirrhosis. Results According to the stage of liver fibrosis, the patients were divided into F0/1 group with 63 patients, F2/3 group with 118 patients, and F4 group with 95 patients, and there were significant differences in albumin, total bilirubin, platelet count, LSM, alpha-fetoprotein, and HBV DNA between the three groups (all P < 0.05). LPRI score was significantly correlated with liver biopsy (r=0.501, P < 0.001); LPRI score had an AUC of 0.88 (95% confidence interval [CI]: 0.83-0.91) in the diagnosis of liver fibrosis and an AUC of 0.79 (95% CI: 0.73-0.83) in the diagnosis of liver cirrhosis, suggesting that the diagnostic performance of LPRI score for significant liver fibrosis was better than that for liver cirrhosis. LPRI had a better diagnostic performance than APRI and FIB-4 (both P < 0.05), and in combination with LSM, LPRI score further supplemented the sensitivity of LSM in the diagnosis of liver cirrhosis, with an increase from 53% to 82%. The cut-off values of LPRI score recommended by Youden index were 6.1 (with a sensitivity of 71% and a specificity of 92%) for significant liver fibrosis and 6.9 (with a sensitivity of 81% and a specificity of 66%) for liver cirrhosis. Conclusion As a simple and convenient noninvasive diagnostic index for liver fibrosis, LPRI score has a certain application value in the diagnosis and staging of liver fibrosis and liver cirrhosis in chronic hepatitis B patients. -
Key words:
- Hepatitis B, Chronic /
- Liver Cirrhosis /
- Diagnosis
-
表 1 入组患者的基线特征
Table 1. The baseline characteristics of all enrolled patients
项目 总体(n=276) F0/1组(n=63) F2/3组(n=118) F4组(n=95) χ2值 P值 人口学数据 年龄(岁) 39.0(31.0~48.0) 37.0(29.0~44.0) 39.0(31.8~46.3) 42.0(32.0~51.0) 2.205 0.332 男性(%) 70.4 66.7 70.3 77.1 146.962 <0.001 BMI(kg/m2) 23.2(21.0~25.1) 22.9(20.6~24.8) 23.0(21.0~24.7) 24.2 (21.6~26.8) 3.891 0.143 血清生化学检测 ALT(U/L) 60.9(36.0~100.0) 70.9(45.0~109.0) 61.7(35.1~101.0) 57.0(34.0~93.0) 2.737 0.254 AST(U/L) 43.9(31.8~64.0) 43.0(30.2~61.0) 44.0(32.1~66.2) 43.1(31.0~66.5) 0.244 0.885 Alb(g/L) 43.0(39.7~46.3) 44.0(41.0~47.0) 43.1(40.6~46.6) 41.9(37.8~45.5) 8.096 0.017 TBil(μmol/L) 15.5(11.0~24.5) 12.2(10.1~17.8) 13.6(10.7~17.4) 29.0(16.0~50.3) 69.988 <0.001 PLT(×109/L) 154.5(116.3~192.0) 192.0(161.0~238.0) 154.0(120.0~187.5) 128.0(98.0~163.0) 25.752 <0.001 LSM(kPa) 11.1(7.5~17.1) 6.8(5.3~8.4) 11.8(8.1~14.9) 17.2(11.3~22.3) 98.493 <0.001 AFP(ng/mL) 4.1(2.2~9.0) 2.5(1.5~5.0) 5.0(2.8~9.7) 5.8(2.9~17.9) 45.271 <0.001 病毒学检测 HBV DNA(log IU/mL) 6.3(5.1~7.5) 6.3(5.1~7.4) 6.2(5.0~7.2) 5.9(4.4~6.9) 10.769 0.005 表 2 不同肝纤维化模型LPRI与LSM、APRI、FIB-4的AUC比较
Table 2. The comparison of AUC between LPRI, LSM, APRI and FIB-4
不同模型比较 ≥F2组(n=213) F4组(n=94) △AUC Z值 P值 △AUC Z值 P值 LPRI vs LSM 0.010 0.52 0.600 0.010 0.63 0.530 LPRI vs APRI 0.180 6.08 <0.000 1 0.220 6.40 <0.000 1 LPRI vs FIB-4 0.132 4.60 <0.000 1 0.170 5.43 <0.000 1 注:△AUC,前后两种模型AUC的差值。 表 3 LPRI评分和LSM的肝纤维化诊断性能
Table 3. The diagnostic performance of LPRI score and LSM in significant fibrosis and cirrhosis
项目 LPRI LSM LSM联合LPRI ≥F2组 F4组 ≥F2组 F4组 ≥F2组 F4组 约登指数推荐界值 6.1 6.9 9.4 kPa 17.0 kPa - - 灵敏度(%) 71 81 73 53 79 82 特异度(%) 92 66 88 89 84 65 阳性预测值(%) 95 55 96 71 94 55 阴性预测值(%) 47 87 50 78 54 87 -
[1] Chinese Foundation for Hepatitis Prevention and Control; Chinese Society of Infectious Disease and Chinese Society of Hepatology, Chinese Medical Association; Liver Disease Committee of Chinese Research Hospital Association. Consensus on clinical application of transient elastography detecting liver fibrosis: A 2018 update[J]. Chin J Hepatol, 2019, 27(3): 182-191. DOI: 10.3760/cma.j.issn.1007-3418.2019.03.004.中国肝炎防治基金会, 中华医学会感染病学分会, 中华医学会肝病学分会和中国研究型医院学会肝病专业委员会. 瞬时弹性成像技术诊断肝纤维化专家共识(2018年更新版)[J]. 中华肝脏病杂志, 2019, 27(3): 182-191. DOI: 10.3760/cma.j.issn.1007-3418.2019.03.004. [2] LI HJ, HE JS, HU SL, et al. Clinical performance of acoustic radiation force impulse imaging combined with transient elastography and aspartate aminotransferase-to-platelet ratio index in evaluating the degree of liver fibrosis in hepatitis B patients[J]. Clin J Med Offic, 2020, 48(9): 1090-1091, 1094. DOI: 10.16680/j.1671-3826.2020.09.35.栗红江, 何久胜, 胡素玲, 等. 声辐射力脉冲成像技术、瞬时弹性成像技术及天冬氨酸氨基转移酶与血小板比率指数联合检测乙型肝炎肝纤维化程度临床效能[J]. 临床军医杂志, 2020, 48(9): 1090-1091, 1094. DOI: 10.16680/j.1671-3826.2020.09.35. [3] TERRAULT NA, LOK A, MCMAHON BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance[J]. Hepatology, 2018, 67(4): 1560-1599. DOI: 10.1002/hep.29800. [4] European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection[J]. J Hepatol, 2017, 67(2): 370-398. DOI: 10.1016/j.jhep.2017.03.021. [5] Chinese Society of Infectious Diseases, Chinese Medical Association, Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B (version 2019)[J]. J Clin Hepatol, 2019, 35(12): 2648-2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007.中华医学会感染病学分会, 中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35(12): 2648-2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. [6] PARK JJ, PARK JY, KIM DY, et al. Prediction of significant fibrosis in chronic hepatitis C patients with normal ALT[J]. Hepatogastroenterology, 2011, 58(109): 1321-1327. DOI: 10.5754/hge11041. [7] OKAJIMA A, SUMIDA Y, TAKETANI H, et al. Liver stiffness measurement to platelet ratio index predicts the stage of liver fibrosis in non-alcoholic fatty liver disease[J]. Hepatol Res, 2017, 47(8): 721-730. DOI: 10.1111/hepr.12793. [8] JIA J, HOU J, DING H, et al. Transient elastography compared to serum markers to predict liver fibrosis in a cohort of Chinese patients with chronic hepatitis B[J]. J Gastroenterol Hepatol, 2015, 30(4): 756-762. DOI: 10.1111/jgh.12840. [9] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Consensus on the diagnosis and therapy of hepatic fibrosis(2019)[J]. J Clin Hepatol, 2019, 35(10): 2163-2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会感染病学分会. 肝纤维化诊断及治疗共识(2019年)[J]. 临床肝胆病杂志, 2019, 35(10): 2163-2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007. [10] CHANG PE, HARTONO JL, NGAI YL, et al. Optimal liver stiffness measurement values for the diagnosis of significant fibrosis and cirrhosis in chronic liver disease in Singapore[J]. Singapore Med J, 2019, 60(10): 532-537. DOI: 10.11622/smedj.2018156. [11] AGBIM U, ASRANI SK. Non-invasive assessment of liver fibrosis and prognosis: an update on serum and elastography markers[J]. Expert Rev Gastroenterol Hepatol, 2019, 13(4): 361-374. DOI: 10.1080/17474124.2019.1579641. [12] ZHANG JL, ZOU GZ, GAO YF, et al. Value of globulin-platelet model in diagnosis of liver fibrosis in patients with chronic hepatitis B virus infection and alanine aminotransferase < 2×upper limit of normal[J]. J Clin Hepatol, 2020, 36(5): 1029-1032. DOI: 10.3969/j.issn.1001-5256.2020.05.016.张杰灵, 邹桂舟, 郜玉峰, 等. GP模型对ALT小于2倍正常值上限的慢性HBV感染者肝纤维化的诊断价值[J]. 临床肝胆病杂志, 2020, 36(5): 1029-1032. DOI: 10.3969/j.issn.1001-5256.2020.05.016. [13] NEWSOME PN, SASSO M, DEEKS JJ, et al. FibroScan-AST (FAST) score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis: a prospective derivation and global validation study[J]. Lancet Gastroenterol Hepatol, 2020, 5(4): 362-373. DOI: 10.1016/S2468-1253(19)30383-8. [14] GONG H, LI LP. Value of Fibroscan combined with GPR, APRI, NFS or FIB-4 for progressive liver fibrosis in patients with chronic hepatitis B and nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2020, 36(3): 541-545. DOI: 10.3969/j.issn.1001-5256.2020.03.DOI: 10.3969/j.issn.1001-5256.2020.03.014.龚航, 李良平. FibroScan分别与GPR、APRI、NFS、FIB-4联合应用对慢性乙型肝炎合并非酒精性脂肪性肝病进展期肝纤维化的诊断价值比较[J]. 临床肝胆病杂志, 2020, 36(3): 541-545. DOI: 10.3969/j.issn.1001-5256.2020.03.014. [15] TANG L, DENG YQ, WANG H, et al. Diagnostic value of noninvasive evaluation model of liver fibrosis in chronic hepatitis B[J]. Chin Gen Pract, 2020, 23(27): 3408-3415. DOI: 10.12114/j.issn.1007-9572.2020.00.354.唐龙, 邓永琼, 王鸿, 等. 无创肝纤维化模型对慢性乙型病毒性肝炎肝纤维化的诊断价值研究[J]. 中国全科医学, 2020, 23(27): 3408-3415. DOI: 10.12114/j.issn.1007-9572.2020.00.354. -



 PDF下载 ( 2320 KB)
PDF下载 ( 2320 KB)

 下载:
下载:



