预测HBV相关肝细胞癌生存的列线图模型的建立
DOI: 10.3969/j.issn.1001-5256.2022.07.020
Establishment of a nomogram model for predicting the survival of hepatitis B virus-related hepatocellular carcinoma
-
摘要:
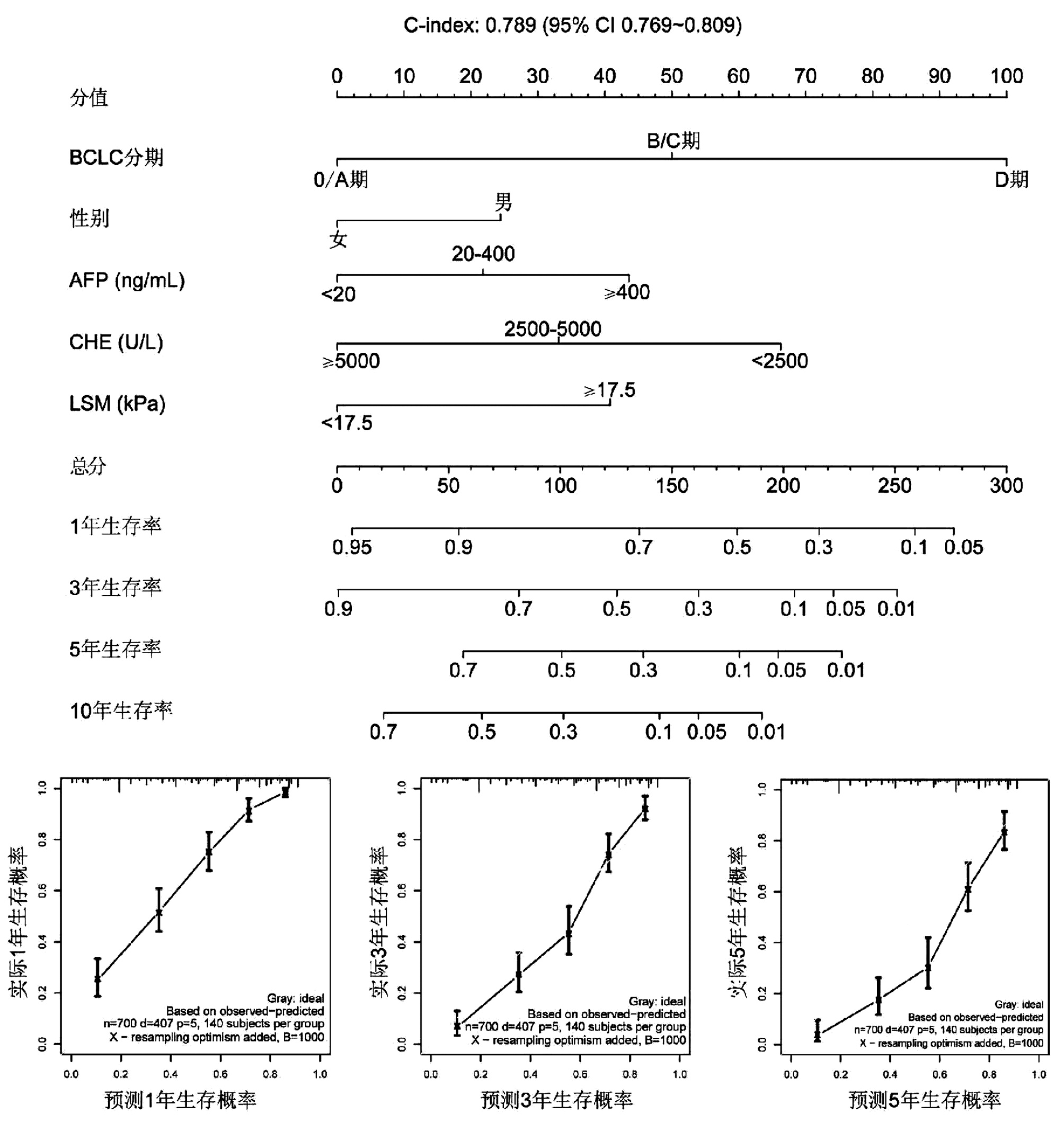
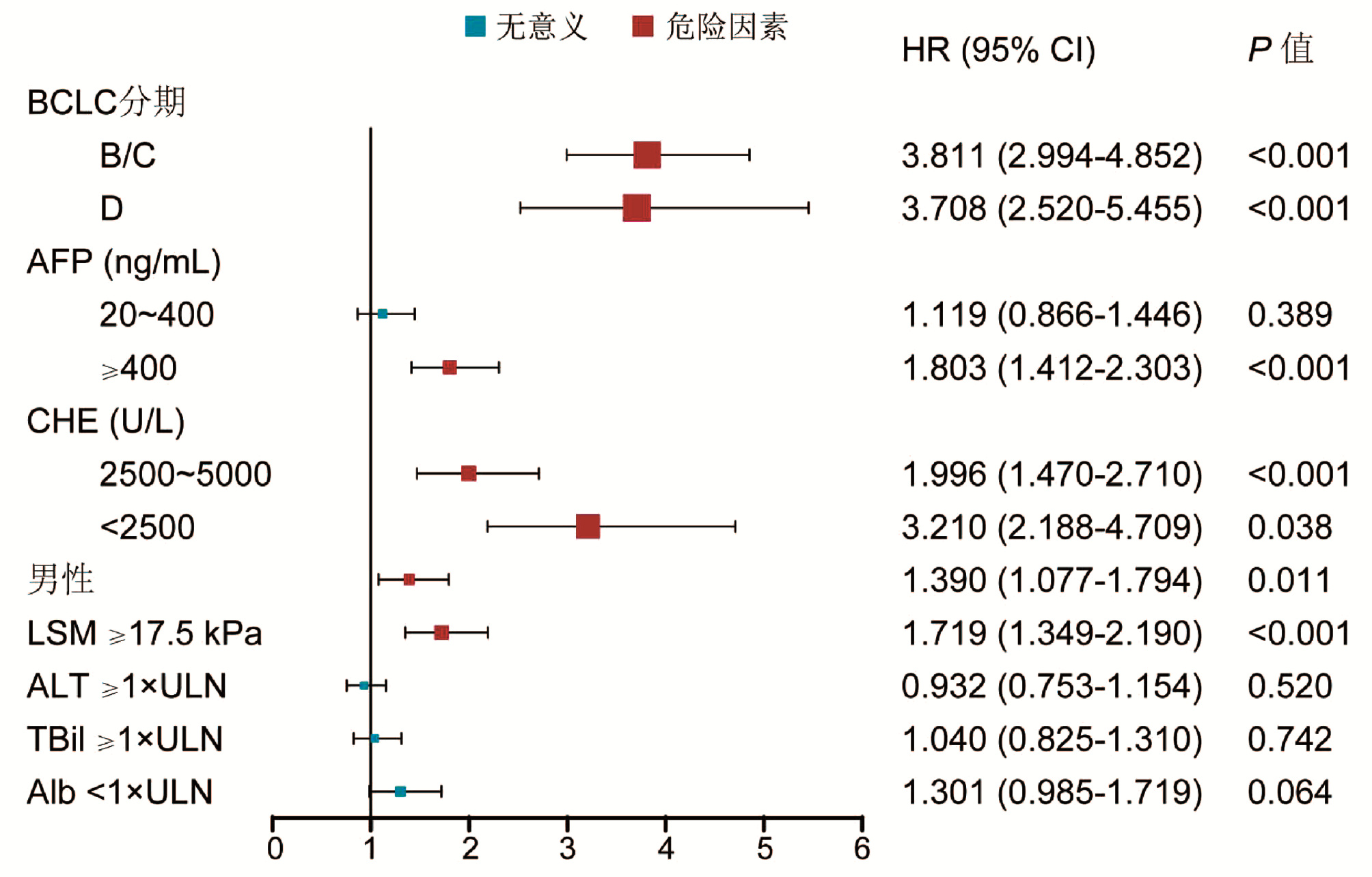
目的 筛选HBV相关肝细胞癌(HCC)死亡的危险因素并建立列线图预测模型。 方法 回顾性分析2010年1月—2020年1月在解放军总医院第五医学中心首次确诊为HBV相关HCC的700例患者的资料并进行随访,起点为HCC的诊断日期,终点为死亡。根据随访结果,分为死亡组(n=407)和生存组(n=293)。计量资料用组间比较采用独立样本t检验或Mann-Whitney U检验;计数资料组间比较采用χ2检验;采用Kaplan-Meier法计算生存率,log-rank检验进行单因素分析,应用多变量Cox比例风险回归筛选独立危险因素,并构建可预测1、3、5年生存率的列线图模型,采用200次10折交叉验证法对模型进行评价。 结果 两组的性别构成、Alb、TBil、ALT、AFP、CHE、LSM及BCLC分期比较差异均有统计学意义(P值均<0.05)。多因素分析显示男性[风险比(HR)=1.390,95%CI:1.077~1.794]、CHE(2500~5000 U/L)(HR=1.996,95%CI:1.470~2.710)、CHE<2500 U/L(HR=3.210,95%CI:2.188~4.709)、AFP≥400 ng/mL(HR=1.803,95%CI:1.412~2.303)、肝弹性值≥17.5 kPa(HR=1.719,95%CI: 1.349~2.190)、巴塞罗那分期B/C(HR=3.811,95%CI:2.994~4.852)、巴塞罗那分期D(HR=3.708,95%CI:2.520~5.455)为死亡的独立危险因素(P值均<0.05)。基于以上因素建立列线图模型,一致性指数为0.789(95%CI:0.769~0.809),校准曲线拟合良好,模型预测值与实际观测值之间的差异无统计学意义。 结论 本研究建立的列线图模型可以个体化预测HBV相关HCC患者的1、3、5年的生存率,有助于准确评估预后。 Abstract:Objective To investigate the risk factors for death in hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC), and to establish a nomogram predictive model. Methods A retrospective analysis was performed for the clinical data of 700 patients who were diagnosed with HBV-related HCC for the first time in The Fifth Medical Center of Chinese PLA General Hospital from January 2010 to January 2020, and the starting point of follow-up was the date of HCC diagnosis, with death as the endpoint. According to the results of follow-up, the patients were divided into death group with 407 patients and survival group with 293 patients. The independent samples t-test or the Mann-Whitney U test was used for comparison of continuous data between groups, and the chi-square test was used for comparison of categorical data between groups. The Kaplan-Meier method was used to calculate survival rates, and the log-rank test was used for univariate analysis. The multivariate Cox proportional-hazards regression model was used to screen out independent risk factors and establish a nomogram model to predict 1-, 3-, and 5-year survival rates, and 10-fold cross validation was performed 200 times to evaluate the model. Results There were significant differences between the two groups in sex composition, albumin, total bilirubin, alanine aminotransferase, alpha-fetoprotein (AFP), cholinesterase (CHE), liver stiffness measurement (LSM), and Barcelona Clinic Liver Cancer (BCLC) stage (all P < 0.05). The multivariate analysis showed that male sex (hazard ratio [HR]=1.390, 95% confidence interval [CI]: 1.077-1.794, P < 0.05), CHE (2500-5000 U/L) (HR=1.996, 95%CI: 1.470-2.710, P < 0.05), CHE < 2500 U/L (HR=3.210, 95%CI: 2.188-4.709, P < 0.05), AFP≥400 ng/mL (HR=1.803, 95%CI: 1.412-2.303, P < 0.05), LSM ≥17.5 kPa (HR=1.719, 95%CI: 1.349-2.190, P < 0.05), BCLC stage B/C (HR=3.811, 95%CI: 2.994-4.852, P < 0.05), and BCLC stage D (HR=3.708, 95%CI: 2.520-5.455, P < 0.05) were independent risk factors for death. The nomogram model established based on the above factors had an index of concordance of 0.789 (95%CI: 0.769-0.809) with well-fitted calibration curves, and there was no significant difference between the predicted value of the model and the actual observed value. Conclusion The nomogram model established in this study can predict the 1-, 3-, and 5-year survival rates of HBV-related HCC patients and help to accurately assess the prognosis of patients. -
Key words:
- Carcinoma, Hepatocellular /
- Hepatitis B virus /
- Nomograms
-
表 1 纳入患者的基线资料
Table 1. Baseline characteristics of enrolled patients
项目 总体(n=700) 死亡组(n=407) 生存组(n=293) 统计值 P值 男[例(%)] 522(74.6) 332(81.6) 190(64.8) χ2=25.13 <0.001 年龄(岁) 53.8±9.3 54.1±9.5 53.6±8.9 t=-0.67 0.501 家族史[例(%)] 385(55.0) 213(52.3) 172(58.7) χ2=2.79 0.095 糖尿病[例(%)] 90(12.9) 49(12.0) 41(14.0) χ2=0.58 0.446 HBeAg阳性[例(%)] 241(34.4) 137(33.7) 104(35.5) χ2=0.25 0.614 HBeAg血清学转换1)[例(%)] 53(13.4) 37(15.7) 16(9.9) χ2=2.37 0.124 LSM≥17.5 kPa[例(%)] 465(66.4) 315(77.4) 150(51.2) χ2=52.40 <0.001 Alb(g/L) 33.20±6.20 31.57±6.10 35.60±5.60 t=8.90 <0.001 TBil(μmol/L) 19.2(13.2~32.1) 22.0(14.8~41.4) 16.2(11.4~23.4) Z=-7.18 <0.001 PLT(×109/L) 94(59~145) 92(58~145) 95(61~146) Z=-0.43 0.670 ALT(U/L) 34(23~52) 45(30~71) 25(20~33) Z=-13.09 <0.001 AFP[例(%)] χ2=56.06 <0.001 <20 ng/mL 319(45.6) 147(36.1) 172(58.7) 20~400 ng/mL 199(28.4) 114(28) 85(29.0) ≥400 ng/mL 182(26.0) 146(35.9) 36(12.3) CHE[例(%)] χ2=121.78 <0.001 ≥5000 U/L 241(34.4) 78(19.2) 163(55.6) 2500~5000 U/L 295(42.2) 188(46.2) 107(36.5) <2500 U/L 164(23.4) 141(34.6) 23(7.8) BCLC分期[例(%)] χ2=174.49 <0.001 0/A 333(47.6) 109(26.8) 224(76.5) B/C 305(43.6) 239(58.7) 66(22.5) D 62(8.8) 59(14.5) 3(1.0) 注:1)定义为经抗病毒治疗后HBeAg阳性转为抗HBe阳性者在HBeAg阳性(397例)中的比例。 表 2 200次10折交叉验证的AUC值
Table 2. The area under the receiver operating characteristic curves from 200-time 10-fold cross validation
生存率 最小值 Q25 中位值 平均值 Q75 最大值 1年 0.704 0.834 0.864 0.862 0.893 0.968 3年 0.679 0.831 0.863 0.860 0.894 0.981 5年 0.609 0.801 0.844 0.841 0.887 0.994 -
[1] Chinese Society of Liver Cancer, Chinese Anti-Cancer Association; Liver Cancer Study Group, Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Pathology, Chinese Anti-Cancer Association; et al. Evidence-based practice guidelines for the standardized pathological diagnosis of primary liver cancer in China(2015 update)[J]. J Clin Hepatol, 2015, 31(6): 833-839. DOI: 10.3969/j.issn.1001-5256.2015.06.004.中国抗癌协会肝癌专业委员会, 中华医学会肝病学分会肝癌学组, 中国抗癌协会病理专业委员会, 等. 原发性肝癌规范化病理诊断指南(2015年版)[J]. 临床肝胆病杂志, 2015, 31(6): 833-839. DOI: 10.3969/j.issn.1001-5256.2015.06.004. [2] KULIK L, EL-SERAG HB. Epidemiology and management of hepatocellular carcinoma[J]. Gastroenterology, 2019, 156(2): 477-491. e1. DOI: 10.1053/j.gastro.2018.08.065. [3] Chinese Society of Infectious Diseases, Chinese Medical Association, Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B (version 2019)[J]. J Clin Hepatol, 2019, 35(12): 2648-2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007.中华医学会感染病学分会, 中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35(12): 2648-2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. [4] WANG CY, YANG WC, TAN WH, et al. Nomogram for predicting significant liver injury in chronic hepatitis B patients with immune tolerance[J]. J Clin Hepatol, 2021, 37(7): 1529-1533. DOI: 10.3969/j.issn.1001-5256.2021.07.010.王春艳, 杨武才, 谭文辉, 等. 慢性乙型肝炎免疫耐受期患者显著肝损伤的列线图模型及其预测价值分析[J]. 临床肝胆病杂志, 2021, 37(7): 1529-1533. DOI: 10.3969/j.issn.1001-5256.2021.07.010. [5] XU J, JI D, WANG CY, et al. Clinical significance of plasma D-dimers in patients with hepatitis B cirrhosis[J]. J Clin Hepatol, 2020, 36(3): 551-555. DOI: 10.3969/j.issn.1001-5256.2020.03.016.徐静, 纪冬, 王春艳, 等. 乙型肝炎肝硬化患者血浆D-二聚体水平变化的临床意义[J]. 临床肝胆病杂志, 2020, 36(3): 551-555. DOI: 10.3969/j.issn.1001-5256.2020.03.016. [6] MA LJ, JI D, WANG CY, et al. A noninvasive diagnosis model for chronic hepatitis B patient based on conventional parameters[J]. Med J Chin PLA, 2019, 44(10): 857-861. DOI: 10.11855/j.issn.0577-7402.2019.10.08.马丽君, 纪冬, 王春艳, 等. 基于常规指标建立肝脏炎症及纤维化无创诊断模型[J]. 解放军医学杂志, 2019, 44(10): 857-861. DOI: 10.11855/j.issn.0577-7402.2019.10.08. [7] ALLEMANI C, MATSUDA T, di CARLO V, et al. Global surveillance of trends in cancer survival 2000-14(CONCORD-3): Analysis of individual records for 37513025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries[J]. Lancet, 2018, 391(10125): 1023-1075. DOI: 10.1016/S0140-6736(17)33326-3. [8] MEI HSUAN LEE. Risk of hepatocellular carcinoma in patients with hepatitis C virus infection[J/CD]. Chin J Exp Clin Infect Dis(Electronic Edition), 2020, 14(1): 88. DOI: 10.3887/1674-1358-2020-1-1.MEI HSUAN LEE. 丙型肝炎病毒感染者患肝细胞癌的风险[J/CD]. 中华实验和临床感染病杂志(电子版), 2020, 14(1): 88. DOI: 10.3887/1674-1358-2020-1-1. [9] SHARMA SA, KOWGIER M, HANSEN BE, et al. Toronto HCC risk index: A validated scoring system to predict 10-year risk of HCC in patients with cirrhosis[J]. J Hepatol, 2018, 68(1): 92-99. DOI: 10.1016/j.jhep.2017.07.033. [10] FAN C, LI M, GAN Y, et al. A simple AGED score for risk classification of primary liver cancer: Development and validation with long-term prospective HBsAg-positive cohorts in Qidong, China[J]. Gut, 2019, 68(5): 948-949. DOI: 10.1136/gutjnl-2018-316525. [11] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. The guideline of prevention and treatment for chronic hepatitis B (2010 version)[J]. J Clin Hepatol, 2011, 27(1): 113-128. http://lcgdbzz.org/article/id/LCGD201101035中华医学会肝病学分会和感染病学分会. 慢性乙型肝炎防治指南(2010年版)[J]. 临床肝胆病杂志, 2011, 27(1): 113-128. http://lcgdbzz.org/article/id/LCGD201101035 [12] Chinese Society of Liver Cancer, Chinese Anti-Cancer Association; Liver Cancer Study Group, Chinese Society of Hepatology, Chinese Medical Association. Expert Consensus on standardized diagnosis and treatment of primary liver cancer[J]. J Clin Hepatol, 2009, 25(2): 83-92. http://lcgdbzz.org/article/id/LCGD200902003中国抗癌协会肝癌专业委员会, 中国抗癌协会临床肿瘤学协作专业委员会, 中华医学会肝病学分会肝癌学组. 原发性肝癌规范化诊治的专家共识[J]. 临床肝胆病杂志, 2009, 25(2): 83-92. http://lcgdbzz.org/article/id/LCGD200902003 [13] LLOVET JM, BRÚ C, BRUIX J. Prognosis of hepatocellular carcinoma: The BCLC staging classification[J]. Semin Liver Dis, 1999, 19(3): 329-338. DOI: 10.1055/s-2007-1007122. [14] ZHENG R, QU C, ZHANG S, et al. Liver cancer incidence and mortality in China: Temporal trends and projections to 2030[J]. Chin J Cancer Res, 2018, 30(6): 571-579. DOI: 10.21147/j.issn.1000-9604.2018.06.01. [15] LIU YY. New progress of hepatocellular carcinoma treatment[J]. Chin J Dig Surg, 2022, 21(1): 15-18. DOI: 10.3760/cma.j.cn115610-20220107-00020.刘允怡. 肝细胞癌治疗的新发展[J]. 中华消化外科杂志, 2022, 21(1): 15-18. DOI: 10.3760/cma.j.cn115610-20220107-00020. [16] Rospective surveillance for very early hepatocellular carcinoma (PreCar) Expert Pane. Expert consensus on early screening strategies for liver cancer in China[J]. Chin Hepatol, 2021, 26(8): 825-831. DOI: 10.3969/j.issn.1008-1704.2021.08.001.全国多中心前瞻性肝癌极早期预警筛查项目(PRECAR)专家组. 中国肝癌早筛策略专家共识[J]. 肝脏, 2021, 26(8): 825-831. DOI: 10.3969/j.issn.1008-1704.2021.08.001. [17] GOLDBERG DS, TADDEI TH, SERPER M, et al. Identifying barriers to hepatocellular carcinoma surveillance in a national sample of patients with cirrhosis[J]. Hepatology, 2017, 65(3): 864-874. DOI: 10.1002/hep.28765. [18] Professional Committee for Prevention and Control of Hepatobiliary and Pancreatic Diseases of Chinese Preventive Medicine Association; Professional Committee for Hepatology, Chinese Research Hospital Association; Chinese Society of Hepatology, Chinese Medical Association, et al. Guideline for stratified screening and surveillance of primary liver cancer (2020 edition)[J]. J Clin Hepatol, 2021, 37(2): 286-295. DOI: 10.3969/j.issn.1001-5256.2021.02.009.中华预防医学会肝胆胰疾病预防与控制专业委员会, 中国研究型医院学会肝病专业委员会, 中华医学会肝病学分会, 等. 原发性肝癌的分层筛查与监测指南(2020版)[J]. 临床肝胆病杂志, 2021, 37(2): 286-295. DOI: 10.3969/j.issn.1001-5256.2021.02.009. [19] SUN YL, ZHU RT, WANG WJ. Reflection and practice of long-term management of hepatocellular carcinoma[J]. Chin J Dig Surg, 2022, 21(2): 231-236. DOI: 10.3760/cma.j.cn115610-20211122-00582.孙玉岭, 朱荣涛, 王维杰. 肝细胞癌长程化管理的思考与实践[J]. 中华消化外科杂志, 2022, 21(2): 231-236. DOI: 10.3760/cma.j.cn115610-20211122-00582. [20] CHEN WQ, ZHANG RS, ZHANG SW, et al. Report of cancer incidence and mortality in China, 2013[J]. China Cancer, 2017, 26(1): 1-7. DOI: 10.11735/j.issn.1004-0242.2017.01.A001.陈万青, 郑荣寿, 张思维, 等. 2013年中国恶性肿瘤发病和死亡分析[J]. 中国肿瘤, 2017, 26(1): 1-7. DOI: 10.11735/j.issn.1004-0242.2017.01.A001. [21] CHEN SH, JI D, HU ZJ, et al. Transient elastography combined with alpha fetoprotein as an early-warning model for hepatocellular carcinoma[J]. Chin Hepatol, 2019, 24(1): 20-24. DOI: 10.14000/j.cnki.issn.1008-1704.2019.01.009.陈松海, 纪冬, 胡志军, 等. 瞬时弹性成像联合甲胎蛋白对肝细胞癌的早期预警价值[J]. 肝脏, 2019, 24(1): 20-24. DOI: 10.14000/j.cnki.issn.1008-1704.2019.01.009. [22] WEN XY, OU ML, CHENG JJ, et al. Application of serum PIVKA-Ⅱ and AFP in clinical diagnosis of primary hepatocellular carcinoma[J]. Int J Lab Med, 2020, 41(13): 1594-1597. DOI: 10.3969/j.issn.1673-4130.2020.13.014.文小艳, 欧明林, 陈洁晶, 等. 血清PIVKA-Ⅱ与AFP联合检测在原发性肝癌临床诊断中的应用[J]. 国际检验医学杂志, 2020, 41(13): 1594-1597. DOI: 10.3969/j.issn.1673-4130.2020.13.014. [23] GALLE PR, FOERSTER F, KUDO M, et al. Biology and significance of alpha-fetoprotein in hepatocellular carcinoma[J]. Liver Int, 2019, 39(12): 2214-2229. DOI: 10.1111/liv.14223. [24] LIU B, WANG SM, YUAN AL. Correlation between intestinal flora and serum ammonia and cholinesterase in patients with liver cancer[J]. Anhui Med Pharm J, 2021, 25(6): 1128-1131. DOI: 10.3969/j.issn.1009-6469.2021.06.016.刘波, 王少敏, 袁岸龙. 肝癌病人肠道菌群与血氨、血清胆碱酯酶的相关性[J]. 安徽医药, 2021, 25(6): 1128-1131. DOI: 10.3969/j.issn.1009-6469.2021.06.016. [25] KONG J, XIANG XX. Value of serum cholinesterase in diagnosis/treatment and prognostic evaluation of liver diseases[J]. J Clin Hepatol, 2017, 33(9): 1806-1809. DOI: 10.3969/j.issn.1001-5256.2017.09.040.孔剑, 向晓星. 血清胆碱酯酶在肝病诊疗及转归中的应用价值[J]. 临床肝胆病杂志, 2017, 33(9): 1806-1809. DOI: 10.3969/j.issn.1001-5256.2017.09.040. [26] WANG L, LIU XE, ZHUANG H. The clinical application of Fibro Touch in patients with liver fibrosis, cirrhosis and hepatocellular carcinoma caused by chronic hepatitis B[J]. Chin J Viral Dis, 2017, 33(9): 1806-1809. DOI: 10.3969/j.issn.1001-5256.2017.09.040.王林, 刘学恩, 庄辉. FibroTouch检测在慢性乙型肝炎肝纤维化、肝硬化和肝癌患者中的临床应用[J]. 中国病毒病杂志, 2017, 33(9): 1806-1809. DOI: 10.3969/j.issn.1001-5256.2017.09.040. [27] ABDELKADER NA, ABDELALEEM MH, EI MAATY MA, et al. Role of transient elastography in the prediction of de novo recurrence of hepatocellular carcinoma after radiofrequency ablation: Single-center Egyptian study[J]. Egyptian Liver J, 2021, 11(1): 28. DOI: 10.1186/S43066-021-00099-3. [28] JUNG KS, KIM SU, CHOI GH, et al. Prediction of recurrence after curative resection of hepatocellular carcinoma using liver stiffness measurement (FibroScan®)[J]. Ann Surg Oncol, 2012, 19(13): 4278-4286. DOI: 10.1245/s10434-012-2422-3. [29] LI M, NIE QH. Value of FibroScan for diagnosis of primary liver cancer: A Meta-analysis[J]. J Clin Hepatol, 2016, 32(2): 312-316. DOI: 10.3969/j.issn.1001-5256.2016.02.023.李汨, 聂青和. FibroScan诊断原发性肝癌准确性的Meta分析[J]. 临床肝胆病杂志, 2016, 32(2): 312-316. DOI: 10.3969/j.issn.1001-5256.2016.02.023. [30] HE YJ, ZHANG ZM, HE WM, et al. Epidemiological characteristics and prognosis of hepatocellular carcinoma: A single-center observational real-world cohort study of 1302 cases[J]. J Clin Hepatol, 2019, 35(5): 1002-1007. DOI: 10.3969/j.issn.1001-5256.2019.05.014.何雅婧, 张植明, 何伟猛, 等. 1302例单中心观察性肝细胞癌真实世界队列的流行病学特征与预后[J]. 临床肝胆病杂志, 2019, 35(5): 1002-1007. DOI: 10.3969/j.issn.1001-5256.2019.05.014. [31] TSILIMIGRAS DI, BAGANTE F, SAHARA K, et al. Prognosis after resection of Barcelona Clinic Liver Cancer (BCLC) Stage 0, A and B hepatocellular carcinoma: A comprehensive assessment of the current BCLC classification[J]. Ann Surg Oncol, 2019, 26(11): 3693-3700. DOI: 10.1245/s10434-019-07580-9. [32] LI JH, FU N, NIU XM, et al. Etiology and clinical characteristics in 573 patients with prim ary liver cancer[J]. J Prac Hepatol, 2015, 18(4): 399-402. DOI: 10.3969/j.issn.1672-5069.2015.04.017.李佳红, 付娜, 牛学敏, 等. 573例原发性肝癌病因及临床特点分析[J]. 实用肝脏病杂志, 2015, 18(4): 399-402. DOI: 10.3969/j.issn.1672-5069.2015.04.017. [33] ZHANG L, YANL, NIU H, et al. A nomogram to predict prognosis of patients with unresected hepatocellular carcinoma undergoing radiotherapy: A population-based study[J]. J Cancer, 2019, 10(19): 4564-4573. DOI: 10.7150/jca.30365. [34] ZHANG S, WANG X, LI Z, et al. Score for the overall survival probability of patients with first-diagnosed distantly metastatic cervical cancer: A novel nomogram-based risk assessment system[J]. Front Oncol, 2019, 9: 1106. DOI: 10.3389/fonc.2019.01106. [35] LIANG ZC, LI ZW, LAI K, et al. Application of 10-fold cross-validation in the evaluation of generalization ability of prediction models and the realization. in R[J]. Chin J Hospital Statistics, 2020, 27(4): 289-292. DOI: 10.3969/j.issn.1006-5253.2020.04.001.梁子超, 李智炜, 赖铿, 等. 10折交叉验证用于预测模型泛化能力评价及其R软件实现[J]. 中国医院统计, 2020, 27(4): 289-292. DOI: 10.3969/j.issn.1006-5253.2020.04.001. -



 PDF下载 ( 3359 KB)
PDF下载 ( 3359 KB)

 下载:
下载: