肺炎克雷伯菌肝脓肿的临床特征及预后影响因素分析
DOI: 10.3969/j.issn.1001-5256.2022.07.023
Clinical features of Klebsiella pneumoniae liver abscess and influencing factors for prognosis
-
摘要:
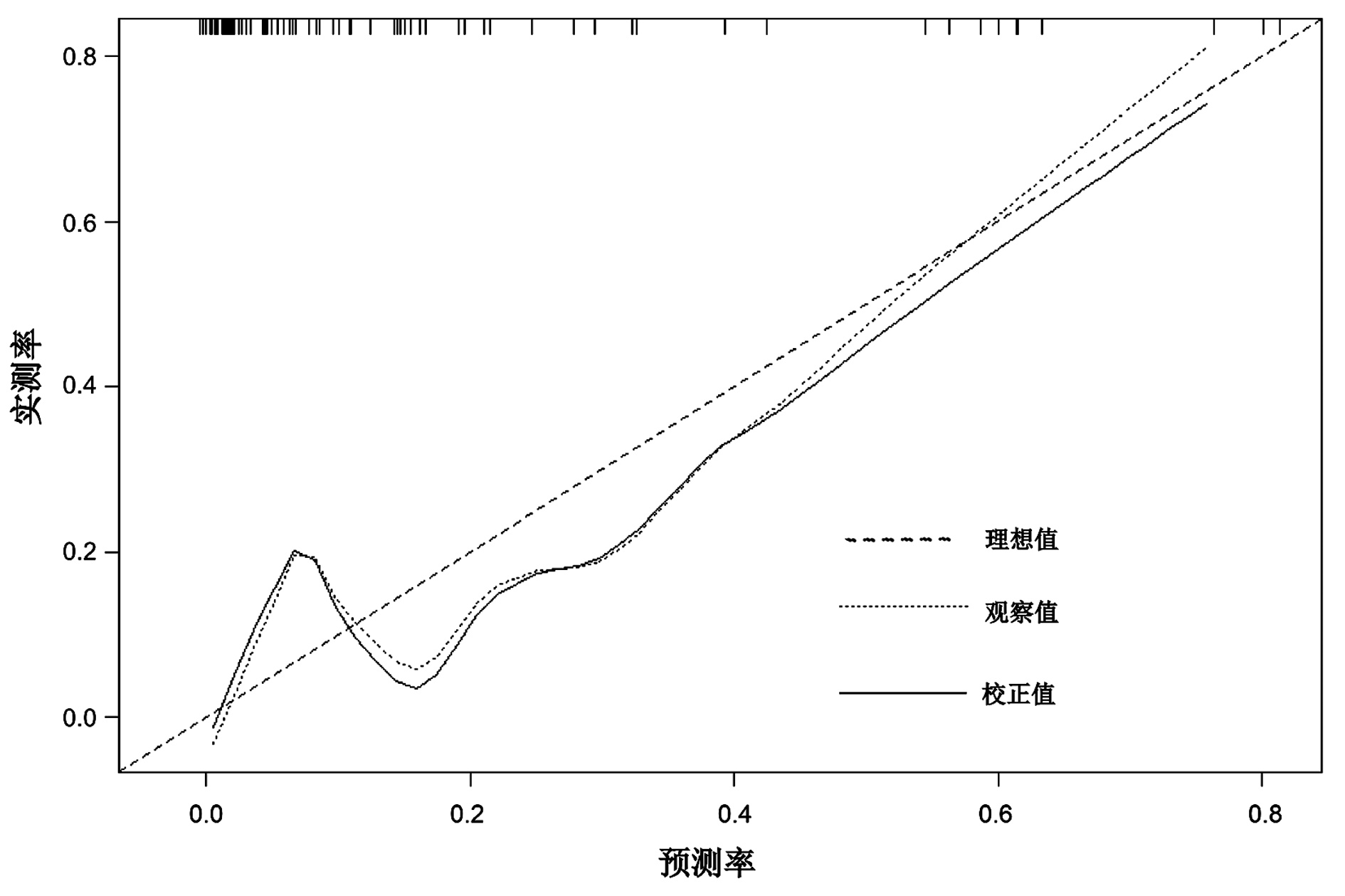
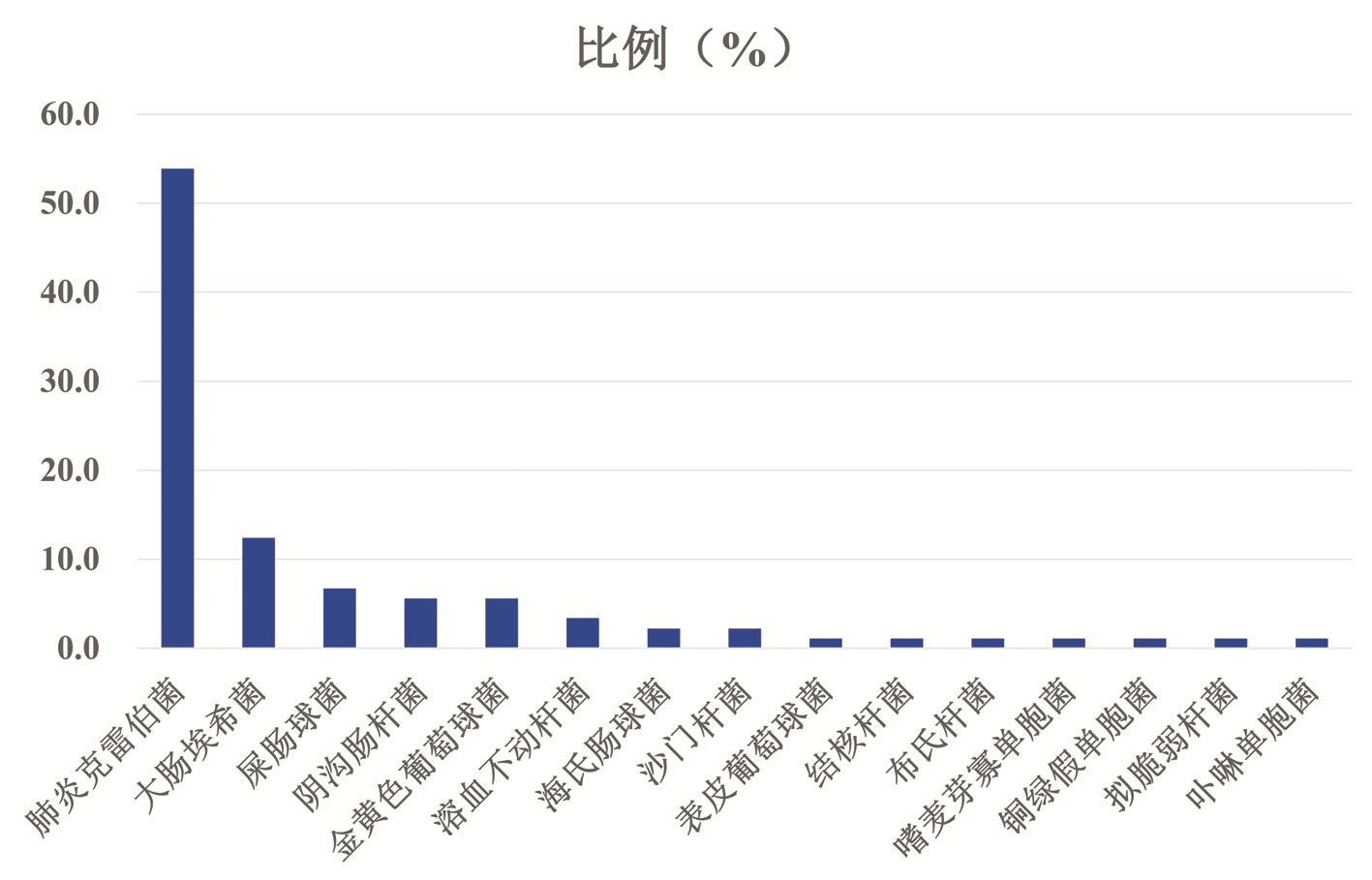
目的 探讨肺炎克雷伯菌肝脓肿的临床特点及预后影响因素。 方法 回顾性选取2010年1月— 2020年1月在首都医科大学附属北京地坛医院住院、并且血培养或脓液培养阳性的肝脓肿患者。根据病原学结果分为肺炎克雷伯菌组(KP组)与非肺炎克雷伯菌组(非KP组)。比较两组之间临床特点。计量资料两组间比较采用两独立样本t检验或Mann-Whitney U检验。计数资料两组间比较采用χ2检验。采用多因素logistic回归分析筛选预后不良的独立影响因素,建立Nomogram预测模型,通过C-index对模型进行内部验证,利用决策曲线对模型进行分析。 结果 共纳入89例有明确病原学结果的肝脓肿患者,KP组48例,非KP组41例。与非KP组患者比较,KP组患者合并2型糖尿病(χ2=12.508,P<0.001)、高血压病(χ2=4.215,P=0.040)、脂肪性肝病(χ2=6.832,P=0.009)的比例较高,而合并恶性肿瘤病史(χ2=15.039,P<0.001)、人类免疫缺陷病毒(HIV)感染(χ2=15.039,P<0.001)、胆囊结石病史(χ2=5.834,P=0.016)的比例较低,KP组患者发生死亡结局的比例(χ2=4.115,P=0.042)亦较非KP组低。KP组白细胞计数(Z=-2.087,P=0.037)、血红蛋白(t=4.67,P<0.001)、纤维蛋白原(Z=-3.300,P=0.001)、C反应蛋白(Z=-3.276,P=0.001)、降钙素原(Z=-0.361,P<0.001)、ALT(Z=-2.436,P=0.015)水平较非KP组高。多因素logistic回归分析显示,合并脓毒症[比值比(OR)=9.110,95%CI: 1.268~65.443,P=0.028]、肺部感染(OR=17.720,95%CI: 2.661~118.010,P=0.003)、低白蛋白水平(OR=0.815,95%CI: 0.692~0.960,P=0.016)是肝脓肿预后不良危险因素,超声引导下脓腔穿刺治疗(OR=8.551,95%CI: 1.549~47.195,P=0. 014)为预后较好保护因素。 结论 KP肝脓肿可能更易发生于糖尿病、高血压、脂肪性肝病人群。合并脓毒症、肺部感染、低白蛋白水平是肝脓肿预后不良危险因素,超声引导下脓腔穿刺治疗为较好预后保护因素。基于本研究构建的列线图预测模型对肝脓肿患者进行干预治疗可改善患者预后。 Abstract:Objective To investigate the clinical features of Klebsiella pneumoniae liver abscess and the influencing factors for prognosis. Methods A retrospective analysis was performed for the patients with liver abscess who were hospitalized and had positive blood culture or pus culture in Beijing Ditan Hospital, Capital Medical University, from January 2010 to January 2020, and according to the results of etiology, these patients were divided into Klebsiella pneumoniae group (KP group) and non-Klebsiella pneumoniae group (non-KP group). Clinical features were compared between the two groups. The two-independent-samples t test or the Mann-Whitney U test was used for comparison of continuous data between two groups, and the chi-square test was used for comparison of categorical data between two groups. A multivariate logistic regression analysis was used to identify independent influencing factors for poor prognosis, and a nomogram predictive model was established based on these factors. Index of concordance (C-index) was used for internal validation, and a decision curve analysis was also performed. Results A total of 89 patients with liver abscess were enrolled, with 48 patients in the KP group and 41 in the non-KP group. Compared with the non-KP group, the KP group had a significantly higher proportion of patients with type 2 diabetes mellitus (χ2=12.508, P < 0.001), hypertension (χ2=4.215, P=0.04), or fatty liver disease (χ2=6.832, P=0.009) and a significantly lower proportion of patients with a medical history of malignant tumor (χ2=15.039, P < 0.001), human immunodeficiency virus infection (χ2=15.039, P < 0.001), or a medical history of gallstones (χ2=5.834, P=0.016), as well as a significantly lower proportion of patients with the outcome of death (χ2=4.115, P=0.042). Compared with the non-KP group, the KP group had significantly higher levels of leukocyte count (Z=-2.087, P=0.037), hemoglobin (t=4.67, P < 0.001), fibrinogen (Z=-3.300, P=0.001), C-reactive protein (Z=-3.276, P=0.001), procalcitonin (Z=-0.361, P < 0.001), and alanine aminotransferase (Z=-2.436, P=0.015). The multivariate logistic regression analysis showed that sepsis (odds ratio [OR]=9.110, 95% confidence interval [CI]: 1.268-65.443, P=0.028), pulmonary infection (OR=17.720, 95%CI: 2.661-118.010, P=0.003), and low albumin level (OR=0.815, 95%CI: 0.692-0.960, P=0.016) were the risk factors for poor prognosis of liver abscess, while ultrasound-guided abscess puncture therapy (OR=8.551, 95%CI: 1.549-47.195, P=0.014) was a protective factor for relatively good prognosis of liver abscess. Conclusion KP liver abscess may be more likely to occur in patients with diabetes mellitus, hypertension, and fatty liver disease. Sepsis, pulmonary infection, and low albumin level are the risk factors for poor prognosis of liver abscess, while ultrasound-guided abscess puncture is a protective factor for relatively good prognosis. Intervention treatment based on the nomogram predictive model established in this study can effectively improve the prognosis of patients with liver abscess. -
Key words:
- Liver Abscess /
- Klebsiella Pneumonia /
- Nomograms /
- Prognosis
-
表 1 KP组与非KP组患者基本资料比较
Table 1. Comparison of basic characteristics between the KP and non-KP patients
指标 总例数(n=89) KP组(n=48) 非KP组(n=41) 统计值 P值 年龄(岁) 54.4±13.0 55.2±12.7 53.5±13.4 t=0.610 0.541 性别(男/女,例) 61/28 30/18 31/10 χ2=1.762 0.184 基础疾病[例(%)] 2型糖尿病 35(39.3) 27(56.3) 8(19.5) χ2=12.508 <0.001 高血压 27(30.3) 19(39.6) 8(19.5) χ2=4.215 0.040 脂肪性肝病 17(19.1) 14(29.2) 3(7.3) χ2=6.832 0.009 HIV 17(19.1)) 2(4.2) 15(36.6) χ2=15.039 <0.001 胆囊结石 13(14.6) 3(6.3) 10(24.4) χ2=5.834 0.016 腹腔手术史 26(29.2) 11(22.9) 15(36.6) χ2=1.998 0.158 肝硬化 9(10.1) 2(4.2) 7(17.1) χ2=2.757 0.097 恶性肿瘤 17(19.1) 2(4.2) 15(36.6) χ2=15.039 <0.001 慢性肾病 3(3.4) 1(2.1) 2(4.9) χ2=0.019 0.889 病死率[例(%)] 5(5.6) 0 5(12.2) χ2= 4.115 0.042 表 2 KP组与非KP组患者肝脓肿影像学资料及实验室指标比较
Table 2. Comparison of image and laboratory findings between the KP and non-KP patients
指标 总例数(n=89) KP组(n=48) 非KP组(n=41) 统计值 P值 病灶个数[例(%)] χ2=0.027 0.870 单发 60(67.4) 32(66.7) 28(68.3) ≥2个 29(32.6) 16(33.3) 13(31.7) 病灶位置[例(%)] χ2=0.622 0.733 右叶 61(68.5) 33(68.8) 28(68.3) 左叶 15(16.9) 7(14.6) 8(19.5) 左右叶 13(14.6) 8(16.7) 5(12.2) 最大直径(cm) 7.6(4.9~9.9) 8.1(6.4~10.2) 7.0(4.5~8.4) Z=-2.305 0.021 气腔形成[例(%)] 14(15.7) 9(18.8) 5(12.2) χ2=0.717 0.397 腹腔积液[例(%)] 18(20.2) 6(12.5) 12(29.3) χ2=3.854 0.050 脾肿大[例(%)] 28(31.5) 17(35.4) 11(26.8) χ2=0.756 0.385 白细胞计数(×109/L) 9.6(7.4~13.3) 10.6(8.5~14.0) 8.6(6.4~11.9) Z=-2.087 0.037 中性粒细胞计数(×109/L) 7.8(6.0~11.4) 8.7(6.9~11.5) 7.2(5.0~10.4) Z=-1.885 0.060 血红蛋白(g/L) 114.3±21.5 123.1±18.5 103.9±20.2 t=4.670 <0.001 ALT(U/L) 47.5(23.6~111.8) 66.8(28.7~125.7) 37.7(22.4~60.6) Z=-2.436 0.015 总胆红素(μmol/L) 15.9(7.9~31.0) 16.2(7.9~33.5) 15.7(9.3~21.1) Z=-0.638 0.526 碱性磷酸酶(U/L) 132.1(85.3~200.2) 154.8(101.2~198.0) 117.2(73.6~202.2) Z=-1.000 0.319 白蛋白(g/L) 31.8±5.7 32.3±5.6 31.1±5.9 t=0.950 0.344 肌酐(μmol/L) 62.9(53.0~83.3) 62.9(53.0~103.2) 62.9(54.0~80.0) Z=-0.560 0.578 INR 1.25(1.17~1.41) 1.3(1.2~1.4) 1.2(1.1~1.4) Z=-0.758 0.451 纤维蛋白原(mg/dL) 487.0(379.0~591.5) 515.5(464.8~631.2) 455.0(365.0~487.0) Z=-3.300 0.001 C反应蛋白(mg/L) 156.0(79.9~242.6) 185.4(116.4~293.1) 116.4(51.8~187.0) Z=-3.276 0.001 降钙素原(ng/mL) 1.4(0.4~10.6) 2.4(0.9~26.6) 0.8(0.2~3.4) Z=-0.361 <0.001 住院费用(万元) 4.6(2.8~7.2) 4.0(2.8~5.7) 5.1(3.3~8.0) Z=-1.465 0.144 表 3 肝脓肿预后影响因素的多因素logistic回归分析
Table 3. Multivariate logistic regression analysis of prognostic factors in patients with liver abscess
变量 回归系数 SE Wald OR 95%CI P值 脓毒症(有/无) 2.209 1.006 4.823 9.110 1.268~65.443 0.028 肺部感染(有/无) 2.875 0.967 8.830 17.720 2.661~118.010 0.003 超声穿刺(未做/做) 2.146 0.872 6.062 8.551 1.549~47.195 0.014 白蛋白 - 0.205 0.083 6.034 0.815 0.692~0.960 0.016 纤维蛋白原 - 0.005 0.003 3.131 0.995 0.990~1.001 0.077 高密度脂蛋白 2.341 1.726 1.839 10.388 0.353~33.285 0.175 -
[1] MOHSEN AH, GREEN ST, READ RC, et al. Liver abscess in adults: ten years experience in a UK centre[J]. QJM, 2002, 95(12): 797-802. DOI: 10.1093/qjmed/95.12.797. [2] CHEN YC, LIN CH, CHANG SN, et al. Epidemiology and clinical outcome of pyogenic liver abscess: an analysis from the National Health Insurance Research Database of Taiwan, 2000-2011[J]. J Microbiol Immunol Infect, 2016, 49(5): 646-653. DOI: 10.1016/j.jmii.2014.08.028. [3] TSAI FC, HUANG YT, CHANG LY, et al. Pyogenic liver abscess as endemic disease, Taiwan[J]. Emerg Infect Dis, 2008, 14(10): 1592-1600. DOI: 10.3201/eid1410.071254. [4] LIU Y, WANG JY, JIANG W. An increasing prominent disease of Klebsiella pneumoniae liver abscess: Etiology, diagnosis, and treatment[J]. Gastroenterol Res Pract, 2013, 2013: 258514. DOI: 10.1155/2013/258514. [5] YIN D, JI C, ZHANG S, et al. Clinical characteristics and management of 1572 patients with pyogenic liver abscess: A 12-year retrospective study[J]. Liver Int, 2021, 41(4): 810-818. DOI: 10.1111/liv.14760. [6] SIU LK, YEH KM, LIN JC, et al. Klebsiella pneumoniae liver abscess: a new invasive syndrome[J]. Lancet Infect Dis, 2012, 12(11): 881-887. DOI: 10.1016/S1473-3099(12)70205-0. [7] CERWENKA H. Pyogenic liver abscess: differences in etiology and treatment in Southeast Asia and Central Europe[J]. World J Gastroenterol, 2010, 16(20): 2458-2462. DOI: 10.3748/wjg.v16.i20.2458. [8] RUIZ-HERNÁNDEZ JJ, LEÓN-MAZORRA M, CONDE-MARTEL A, et al. Pyogenic liver abscesses: mortality-related factors[J]. Eur J Gastroenterol Hepatol, 2007, 19(10): 853-858. DOI: 10.1097/MEG.0b013e3282eeb53b. [9] YANG CC, YEN CH, HO MW, et al. Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae[J]. J Microbiol Immunol Infect, 2004, 37(3): 176-184. [10] CHUNG DR, LEE SS, LEE HR, et al. Emerging invasive liver abscess caused by K1 serotype Klebsiella pneumoniae in Korea[J]. J Infect, 2007, 54(6): 578-583. DOI: 10.1016/j.jinf.2006.11.008. [11] HUI P, ZHU P, LIAO W, et al. Bacterial flora distribution and antimicrobial resistance of pyogenic liver abscess: a multicenter retrospective study (A report of 897 cases)[J]. Chin J Dig Surg, 2019, 18(10): 924-933. DOI: 10.3760/cma.j.issn.1673-9752.2019.10.007.惠鹏, 朱鹏, 廖威, 等. 细菌性肝脓肿菌群分布与耐药性分析的多中心回顾性研究(附897例报告)[J]. 中华消化外科杂志, 2019, 18(10): 924-933. DOI: 10.3760/cma.j.issn.1673-9752.2019.10.007. [12] LEE JH, JANG YR, AHN SJ, et al. A retrospective study of pyogenic liver abscess caused primarily by Klebsiella pneumoniae vs. non-Klebsiella pneumoniae: CT and clinical differentiation[J]. Abdom Radiol (NY), 2020, 45(9): 2669-2679. DOI: 10.1007/s00261-019-02389-2. [13] XU SB, YANG SY, WENG SS, et al. Clinical characteristics of patients with Klebsiella pneumoniae pyogenic liver abscess[J]. Chin J Intern Med, 2020, 59(6): 439-444. DOI: 10.3760/cma.j.cn112138-20190610-00403.徐水宝, 杨思宇, 翁珊珊, 等. 肺炎克雷伯菌肝脓肿临床特征分析[J]. 中华内科杂志, 2020, 59(6): 439-444. DOI: 10.3760/cma.j.cn112138-20190610-00403. [14] PASTAGIA M, ARUMUGAM V. Klebsiella pneumoniae liver abscesses in a public hospital in Queens, New York[J]. Travel Med Infect Dis, 2008, 6(4): 228-233. DOI: 10.1016/j.tmaid.2008.02.005. [15] MOORE LS, CLARKE IL, DONALDSON H, et al. Community-acquired Klebsiella pneumoniae liver abscess: the London experience[J]. Infection, 2014, 42(1): 219-221. DOI: 10.1007/s15010-013-0520-1. [16] FANG CT, LAI SY, YI WC, et al. Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess[J]. Clin Infect Dis, 2007, 45(3): 284-293. DOI: 10.1086/519262. [17] YAO N, KANG W, LIAN JQ, et al. Clinical features of Klebsiella pneumoniae liver abscess versus Escherichia coli liver abscess[J]. J Clin Hepatol, 2020, 36(9): 2010-2014. DOI: 10.3969/j.issn.1001-5256.2020.09.020.姚娜, 康文, 连建奇, 等. 肺炎克雷伯菌肝脓肿与大肠埃希菌肝脓肿临床特点对比分析[J]. 临床肝胆病杂志, 2020, 36(9): 2010-2014. DOI: 10.3969/j.issn.1001-5256.2020.09.020. [18] LIN JC, SIU LK, FUNG CP, et al. Impaired phagocytosis of capsular serotypes K1 or K2 Klebsiella pneumoniae in type 2 diabetes mellitus patients with poor glycemic control[J]. J Clin Endocrinol Metab, 2006, 91(8): 3084-3087. DOI: 10.1210/jc.2005-2749. [19] CHEN SC, WU WY, YEH CH, et al. Comparison of Escherichia coli and Klebsiella pneumoniae liver abscesses[J]. Am J Med Sci, 2007, 334(2): 97-105. DOI: 10.1097/MAJ.0b013e31812f59c7. [20] QIAN Y, WONG CC, LAI S, et al. A retrospective study of pyogenic liver abscess focusing on Klebsiella pneumoniae as a primary pathogen in China from 1994 to 2015[J]. Sci Rep, 2016, 6: 38587. DOI: 10.1038/srep38587. [21] YOON JH, KIM YJ, JUN YH, et al. Liver abscess due to Klebsiella pneumoniae: risk factors for metastatic infection[J]. Scand J Infect Dis, 2014, 46(1): 21-26. DOI: 10.3109/00365548.2013.851414. [22] CAI MT, FAN CL, LI L, et al. Case-control analysis of liver abscess in patients with acquired immunodeficiency syndrome[J]. Chin J Infect Chemother, 2019, 19(5): 465-472. DOI: 10.16718/j.1009-7708.2019.05.001.蔡妙甜, 范春蕾, 李磊, 等. 艾滋病肝脓肿患者临床特征的对照分析[J]. 中国感染与化疗杂志, 2019, 19(5): 465-472. DOI: 10.16718/j.1009-7708.2019.05.001. [23] ASTON SJ. Pneumonia in the developing world: Characteristic features and approach to management[J]. Respirology, 2017, 22(7): 1276-1287. DOI: 10.1111/resp.13112. [24] NEILL L, EDWARDS F, COLLIN SM, et al. Clinical characteristics and treatment outcomes in a cohort of patients with pyogenic and amoebic liver abscess[J]. BMC Infect Dis, 2019, 19(1): 490. DOI: 10.1186/s12879-019-4127-8. [25] LI S, YU S, PENG M, et al. Clinical features and development of Sepsis in Klebsiella pneumoniae infected liver abscess patients: a retrospective analysis of 135 cases[J]. BMC Infect Dis, 2021, 21(1): 597. DOI: 10.1186/s12879-021-06325-y. [26] CHENG Y, BAI YF, QIU YP, et al. Clinical features of Klebsiella pneumoniae liver abscess and molecular characteristics of bacterial infection[J]. China Mod Doct, 2021, 59(17): 124-128. https://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS202117030.htm程颖, 白永凤, 邱玉萍, 等. 肺炎克雷伯菌肝脓肿的临床特点及感染菌的分子特征[J]. 中国现代医生, 2021, 59(17): 124-128. https://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS202117030.htm [27] MATSUKUMA Y, TANAKA S, TANIGUCHI M, et al. Association of geriatric nutritional risk index with infection-related mortality in patients undergoing hemodialysis: The Q-Cohort Study[J]. Clin Nutr, 2019, 38(1): 279-287. DOI: 10.1016/j.clnu.2018.01.019. [28] SOLOMKIN JS, MAZUSKI JE, BRADLEY JS, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America[J]. Clin Infect Dis, 2010, 50(2): 133-164. DOI: 10.1086/649554. [29] LIU L, CHEN W, LU X, et al. Pyogenic liver abscess: A retrospective study of 105 cases in an emergency department from east China[J]. J Emerg Med, 2017, 52(4): 409-416. DOI: 10.1016/j.jemermed.2016.09.026. -



 PDF下载 ( 2391 KB)
PDF下载 ( 2391 KB)

 下载:
下载: