维生素D缺乏与代谢相关脂肪性肝病的关系
DOI: 10.3969/j.issn.1001-5256.2022.07.034
利益冲突声明:所有作者均声明不存在利益冲突。
作者贡献声明:罗玲负责论文撰写; 廖献花协助论文修改; 钟碧慧负责论文指导和审阅。
Research advances in vitamin D deficiency and metabolic associated fatty liver disease
-
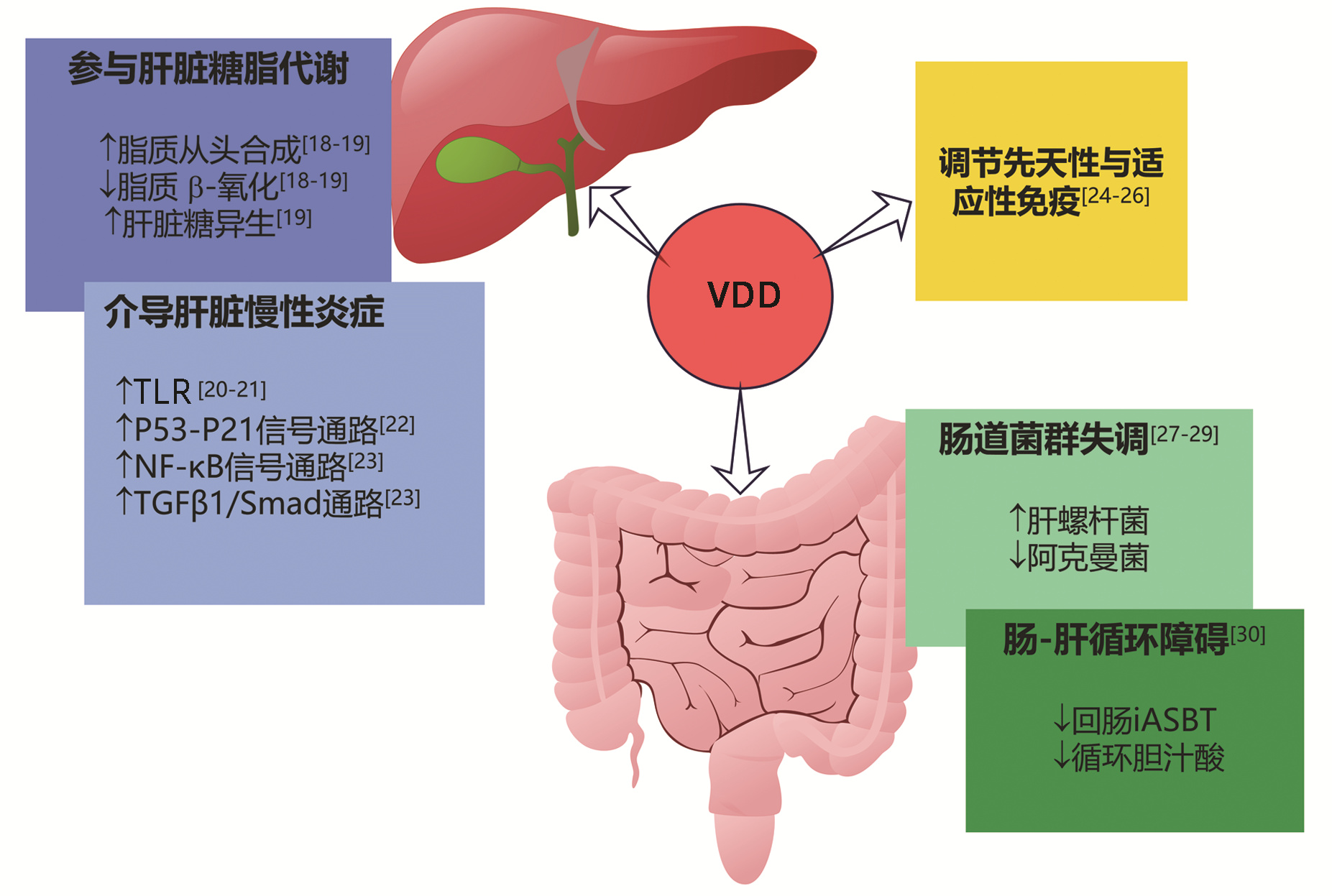
摘要: 代谢相关脂肪性肝病(MAFLD)为全球第一大慢性肝病,但发病机制仍不明确,尚缺乏有效的治疗药物。介绍了MAFLD患者常伴有维生素D缺乏,维生素D可能通过影响糖脂代谢、炎症信号通路、免疫调节、肠道微生态等多种途径参与MAFLD的发生发展。提出维生素D有望成为MAFLD的治疗药物,临床上需关注MAFLD患者维生素D水平的监测和管理,但其内在机制、具体补充剂量及疗程亟待深入探索。Abstract: Metabolic associated fatty liver disease (MAFLD) is the largest chronic liver disease in the world. Its pathogenesis remains unclear and there is still a lack of effective drugs. This article introduces vitamin D deficiency commonly observed in patients with MAFLD, and it is pointed out that vitamin D may participate in the development and progression of MAFLD through various pathways such as glucose and lipid metabolism, inflammatory signaling pathways, immune modulation, and intestinal microecology. It is proposed that vitamin D supplement is expected to become an effective drug for the treatment of MAFLD, and the monitoring and management of vitamin D level should be taken seriously for MAFLD patients in clinical practice. Further studies are needed to explore its underlying mechanism, dose for supplementation, and course of treatment.
-
[1] ESLAM M, NEWSOME PN, SARIN SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement[J]. J Hepatol, 2020, 73(1): 202-209. DOI: 10.1016/j.jhep.2020.03.039. [2] COTTER TG, RINELLA M. Nonalcoholic fatty liver disease 2020: The state of the disease[J]. Gastroenterology, 2020, 158(7): 1851-1864. DOI: 10.1053/j.gastro.2020.01.052. [3] ZHOU F, ZHOU J, WANG W, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: A systematic review and Meta-analysis[J]. Hepatology, 2019, 70(4): 1119-1133. DOI: 10.1002/hep.30702. [4] XIAO QQ, WANG MY, FAN JG. Brief introduction of APASL clinical practice guidelines on metabolic associated fatty liver disease (Treatment Part)[J]. J Clin Hepatol, 2021, 37(1): 41-45. DOI: 10.3969/j.issn.1001-5256.2021.01.009.肖倩倩, 王梦雨, 范建高. 亚太肝病研究学会代谢相关脂肪性肝病临床诊疗指南(治疗部分)简介[J]. 临床肝胆病杂志, 2021, 37(1): 41-45. DOI: 10.3969/j.issn.1001-5256.2021.01.009. [5] ANDERSON JL, MAY HT, HORNE BD, et al. Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population[J]. Am J Cardiol, 2010, 106(7): 963-968. DOI: 10.1016/j.amjcard.2010.05.027. [6] MA JT, CAI S, WAN L, et al. Research progress in the effect of vitamin D deficiency on skeletal and extraskeletal health[J]. Chin J Osteoporosis, 2020, 26(1): 109-113. DOI: 10.3969/j.issn.1006-7108.马江涛, 柴爽, 万雷, 等. 维生素D缺乏对骨和骨外作用研究进展[J]. 中国骨质疏松杂志, 2020, 26(1): 109-113. DOI: 10.3969/j.Issn.1006-7108. [7] PACIFICO L, OSBORN JF, BONCI E, et al. Association between vitamin D levels and nonalcoholic fatty liver disease: Potential confounding variables[J]. Mini Rev Med Chem, 2019, 19(4): 310-332. DOI: 10.2174/1389557518666181025153712. [8] van SCHOOR N, LIPS P. Global overview of vitamin D status[J]. Endocrinol Metab Clin North Am, 2017, 46(4): 845-870. DOI: 10.1016/j.ecl.2017.07.002. [9] LI M, LV F, ZHANG Z, et al. Establishment of a normal reference value of parathyroid hormone in a large healthy Chinese population and evaluation of its relation to bone turnover and bone mineral density[J]. Osteoporos Int, 2016, 27(5): 1907-1916. DOI: 10.1007/s00198-015-3475-5. [10] WAN B, GAO Y, ZHENG Y, et al. Association between serum 25-hydroxy vitamin D level and metabolic associated fatty liver disease (MAFLD)-a population-based study[J]. Endocr J, 2021, 68(6): 631-637. DOI: 10.1507/endocrj.EJ20-0758. [11] NELSON JE, ROTH CL, WILSON LA, et al. Vitamin D deficiency is associated with increased risk of non-alcoholic steatohepatitis in adults with non-alcoholic fatty liver disease: possible role for MAPK and NF-κB?[J]. Am J Gastroenterol, 2016, 111(6): 852-863. DOI: 10.1038/ajg.2016.51. [12] ARAI T, ATSUKAWA M, TSUBOTA A, et al. Association of vitamin D levels and vitamin D-related gene polymorphisms with liver fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease[J]. Dig Liver Dis, 2019, 51(7): 1036-1042. DOI: 10.1016/j.dld.2018.12.022. [13] YANG BB, CHEN YH, ZHANG C, et al. Low vitamin D status is associated with advanced liver fibrosis in patients with nonalcoholic fatty liver disease[J]. Endocrine, 2017, 55(2): 582-590. DOI: 10.1007/s12020-016-1152-x. [14] ZHAI HL, WANG NJ, HAN B, et al. Low vitamin D levels and non-alcoholic fatty liver disease, evidence for their independent association in men in East China: a cross-sectional study (Survey on Prevalence in East China for Metabolic Diseases and Risk Factors (SPECT-China))[J]. Br J Nutr, 2016, 115(8): 1352-1359. DOI: 10.1017/S0007114516000386. [15] DUTRA J, LISBOA QC, FEROLLA SM, et al. Vitamin D levels are not associated with non-alcoholic fatty liver disease severity in a Brazilian population[J]. Int J Vitam Nutr Res, 2021, 91(5-6): 411-418. DOI: 10.1024/0300-9831/a000667. [16] LI L, ZHANG L, PAN S, et al. No significant association between vitamin D and nonalcoholic fatty liver disease in a Chinese population[J]. Dig Dis Sci, 2013, 58(8): 2376-2382. DOI: 10.1007/s10620-013-2658-1. [17] BUZZETTI E, PINZANI M, TSOCHATZIS EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD)[J]. Metabolism, 2016, 65(8): 1038-1048. DOI: 10.1016/j.metabol.2015.12.012. [18] YIN Y, YU Z, XIA M, et al. Vitamin D attenuates high fat diet-induced hepatic steatosis in rats by modulating lipid metabolism[J]. Eur J Clin Invest, 2012, 42(11): 1189-1196. DOI: 10.1111/j.1365-2362.2012.02706.x. [19] ELHAFIZ M, ZHAO G, ISMAIL M, et al. Imbalanced insulin substrate-1 and insulin substrate-2 signaling trigger hepatic steatosis in vitamin D deficient rats: 8-methoxypsoralen, a vitamin D receptor ligand with a promising anti-steatotic action[J]. Biochim Biophys Acta Mol Cell Biol Lipids, 2020, 1865(6): 158657. DOI: 10.1016/j.bbalip.2020.158657. [20] ROTH CL, ELFERS CT, FIGLEWICZ DP, et al. Vitamin D deficiency in obese rats exacerbates nonalcoholic fatty liver disease and increases hepatic resistin and Toll-like receptor activation[J]. Hepatology, 2012, 55(4): 1103-1111. DOI: 10.1002/hep.24737. [21] WANG H, ZHANG Q, CHAI Y, et al. 1, 25(OH)2D3 downregulates the Toll-like receptor 4-mediated inflammatory pathway and ameliorates liver injury in diabetic rats[J]. J Endocrinol Invest, 2015, 38(10): 1083-1091. DOI: 10.1007/s40618-015-0287-6. [22] MA M, LONG Q, CHEN F, et al. Active vitamin D impedes the progression of non-alcoholic fatty liver disease by inhibiting cell senescence in a rat model[J]. Clin Res Hepatol Gastroenterol, 2020, 44(4): 513-523. DOI: 10.1016/j.clinre.2019.10.007. [23] TANG HQ, LI XT, YAN X, et al. Effect of dihydroxyvitamin D3 in regulating NF-κB and TGF-β1/Smad pathway in mice of non-alcoholic steatohepatitis and liver fibrosis[J]. Med J Natl Defend Forces Northwest China, 2016, 37(8): 497-500. DOI: 10.16021/j.cnki.1007-8622.2016.08.003.唐寒秋, 李晓涛, 闫雪, 等. 1, 25-二羟维生素D3通过调节NF-κB和TGF-β1/Smad通路减轻小鼠非酒精型脂肪性肝炎和肝纤维化[J]. 西北国防医学杂志, 2016, 37(8): 497-500. DOI: 10.16021/j.cnki.1007-8622.2016.08.003. [24] KAMEN DL, TANGPRICHA V. Vitamin D and molecular actions on the immune system: modulation of innate and autoimmunity[J]. J Mol Med (Berl), 2010, 88(5): 441-450. DOI: 10.1007/s00109-010-0590-9. [25] LI HJ, HU SL, LIU Y, et al. Correlation between serum 25 hydroxyvitamin D3 level and peripheral blood T lymphocyte subsets in patients with chronic hepatitis B[J]. Clin J Med Offic, 2022, 50(2): 205-207, 210. DOI: 10.16680/j.1671-3826.2022.02.27.栗红江, 胡素玲, 刘洋, 等. 慢性乙型病毒性肝炎患者血清25-羟基维生素D3水平与外周血T淋巴细胞亚群相关性分析[J]. 临床军医杂志, 2022, 50(2): 205-207, 210. DOI: 10.16680/j.1671-3826.2022.02.27. [26] DRORI A, ROTNEMER-GOLINKIN D, AVNI S, et al. Attenuating the rate of total body fat accumulation and alleviating liver damage by oral administration of vitamin D-enriched edible mushrooms in a diet-induced obesity murine model is mediated by an anti-inflammatory paradigm shift[J]. BMC Gastroenterol, 2017, 17(1): 130. DOI: 10.1186/s12876-017-0688-4. [27] YANG LD, HE H, AN ZM. Role of intestinal flora in metabolic-associated fatty liver disease[J]. J Clin Hepatol, 2021, 37(9): 2231-2235. DOI: 10.3969/j.issn.1001-5256.2021.09.046.杨礼丹, 何訸, 安振梅. 肠道菌群在代谢相关脂肪性肝病中的作用[J]. 临床肝胆病杂志, 2021, 37(9): 2231-2235. DOI: 10.3969/j.issn.1001-5256.2021.09.046. [28] FAKHOURY H, KVIETYS PR, ALKATTAN W, et al. Vitamin D and intestinal homeostasis: Barrier, microbiota, and immune modulation[J]. J Steroid Biochem Mol Biol, 2020, 200: 105663. DOI: 10.1016/j.jsbmb.2020.105663. [29] SU D, NIE Y, ZHU A, et al. Vitamin D signaling through induction of paneth cell defensins maintains gut microbiota and improves metabolic disorders and hepatic steatosis in animal models[J]. Front Physiol, 2016, 7: 498. DOI: 10.3389/fphys.2016.00498. [30] KONG M, ZHU L, BAI L, et al. Vitamin D deficiency promotes nonalcoholic steatohepatitis through impaired enterohepatic circulation in animal model[J]. Am J Physiol Gastrointest Liver Physiol, 2014, 307(9): G883-G893. DOI: 10.1152/ajpgi.00427.2013. [31] BARCHETTA I, CIMINI FA, CAVALLO MG. Vitamin D and metabolic dysfunction-associated fatty liver disease (MAFLD): An update[J]. Nutrients, 2020, 12(11): 3302. DOI: 10.3390/nu12113302. [32] DONG B, ZHOU Y, WANG W, et al. Vitamin D receptor activation in liver macrophages ameliorates hepatic inflammation, steatosis, and insulin resistance in mice[J]. Hepatology, 2020, 71(5): 1559-1574. DOI: 10.1002/hep.30937. [33] BOZIC M, GUZMÁN C, BENET M, et al. Hepatocyte vitamin D receptor regulates lipid metabolism and mediates experimental diet-induced steatosis[J]. J Hepatol, 2016, 65(4): 748-757. DOI: 10.1016/j.jhep.2016.05.031. [34] BARCHETTA I, CAROTTI S, LABBADIA G, et al. Liver vitamin D receptor, CYP2R1, and CYP27A1 expression: relationship with liver histology and vitamin D3 levels in patients with nonalcoholic steatohepatitis or hepatitis C virus[J]. Hepatology, 2012, 56(6): 2180-2187. DOI: 10.1002/hep.25930. [35] NOBILI V, REIF S. Vitamin D and liver fibrosis: let's start soon before it's too late[J]. Gut, 2015, 64(5): 698-699. DOI: 10.1136/gutjnl-2014-308175. [36] GUO XF, WANG C, YANG T, et al. Vitamin D and non-alcoholic fatty liver disease: a meta-analysis of randomized controlled trials[J]. Food Funct, 2020, 11(9): 7389-7399. DOI: 10.1039/d0fo01095b. [37] LUKENDA ZANKO V, DOMISLOVIC V, TRKULJA V, et al. Vitamin D for treatment of non-alcoholic fatty liver disease detected by transient elastography: A randomized, double-blind, placebo-controlled trial[J]. Diabetes Obes Metab, 2020, 22(11): 2097-2106. DOI: 10.1111/dom.14129. [38] GEIER A, EICHINGER M, STIRNIMANN G, et al. Treatment of non-alcoholic steatohepatitis patients with vitamin D: a double-blinded, randomized, placebo-controlled pilot study[J]. Scand J Gastroenterol, 2018, 53(9): 1114-1120. DOI: 10.1080/00365521.2018.1501091. [39] DASARATHY J, VARGHESE R, FELDMAN A, et al. Patients with nonalcoholic fatty liver disease have a low response rate to vitamin D supplementation[J]. J Nutr, 2017, 147(10): 1938-1946. DOI: 10.3945/jn.117.254292. [40] TABRIZI R, MOOSAZADEH M, LANKARANI KB, et al. The effects of vitamin D supplementation on metabolic profiles and liver function in patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis of randomized controlled trials[J]. Diabetes Metab Syndr, 2017, 11(Suppl 2): S975-S982. DOI: 10.1016/j.dsx.2017.07.025. [41] DABBAGHMANESH MH, DANAFAR F, ESHRAGHIAN A, et al. Vitamin D supplementation for the treatment of non-alcoholic fatty liver disease: A randomized double blind placebo controlled trial[J]. Diabetes Metab Syndr, 2018, 12(4): 513-517. DOI: 10.1016/j.dsx.2018.03.006. [42] BOUCHER BJ. Why do so many trials of vitamin D supplementation fail?[J]. Endocr Connect, 2020, 9(9): R195-R206. DOI: 10.1530/EC-20-0274. [43] EL-SHERBINY M, ELDOSOKY M, EL-SHAFEY M, et al. Vitamin D nanoemulsion enhances hepatoprotective effect of conventional vitamin D in rats fed with a high-fat diet[J]. Chem Biol Interact, 2018, 288: 65-75. DOI: 10.1016/j.cbi.2018.04.010. [44] NAKANO T, CHENG YF, LAI CY, et al. Impact of artificial sunlight therapy on the progress of non-alcoholic fatty liver disease in rats[J]. J Hepatol, 2011, 55(2): 415-425. DOI: 10.1016/j.jhep.2010.11.028. [45] LUGER M, KRUSCHITZ R, KIENBACHER C, et al. Vitamin D3 loading is superior to conventional supplementation after weight loss surgery in vitamin D-deficient morbidly obese patients: A double-blind randomized placebo-controlled trial[J]. Obes Surg, 2017, 27(5): 1196-1207. DOI: 10.1007/s11695-016-2437-0. -



 PDF下载 ( 2173 KB)
PDF下载 ( 2173 KB)

 下载:
下载:


