肝硬化食管胃底静脉曲张破裂出血患者再出血预测模型的建立
DOI: 10.3969/j.issn.1001-5256.2022.11.011
Developing the prediction model of esophagogastric variceal rebleeding in patients with liver cirrhosis based on artificial neural network
-
摘要:
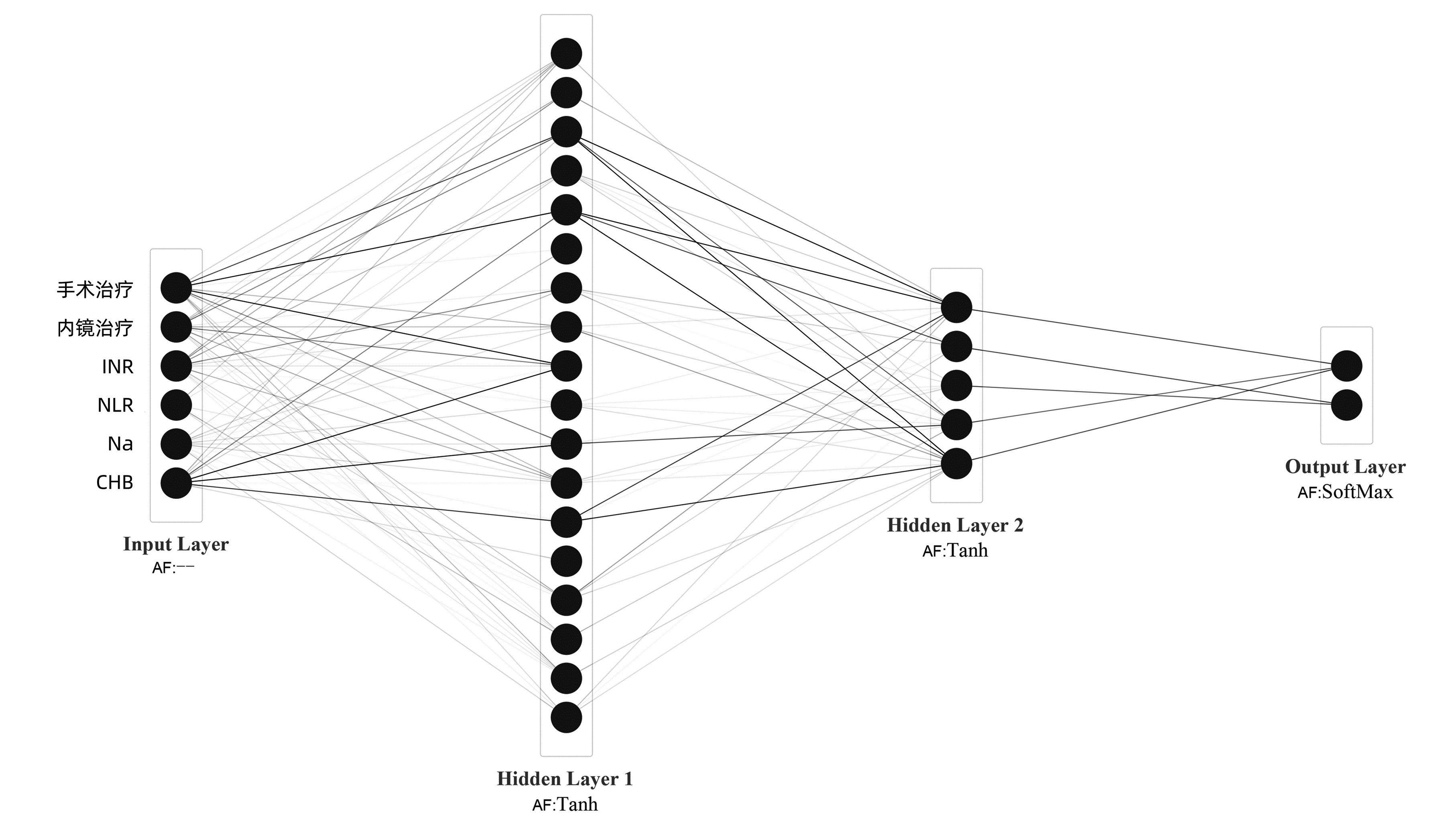
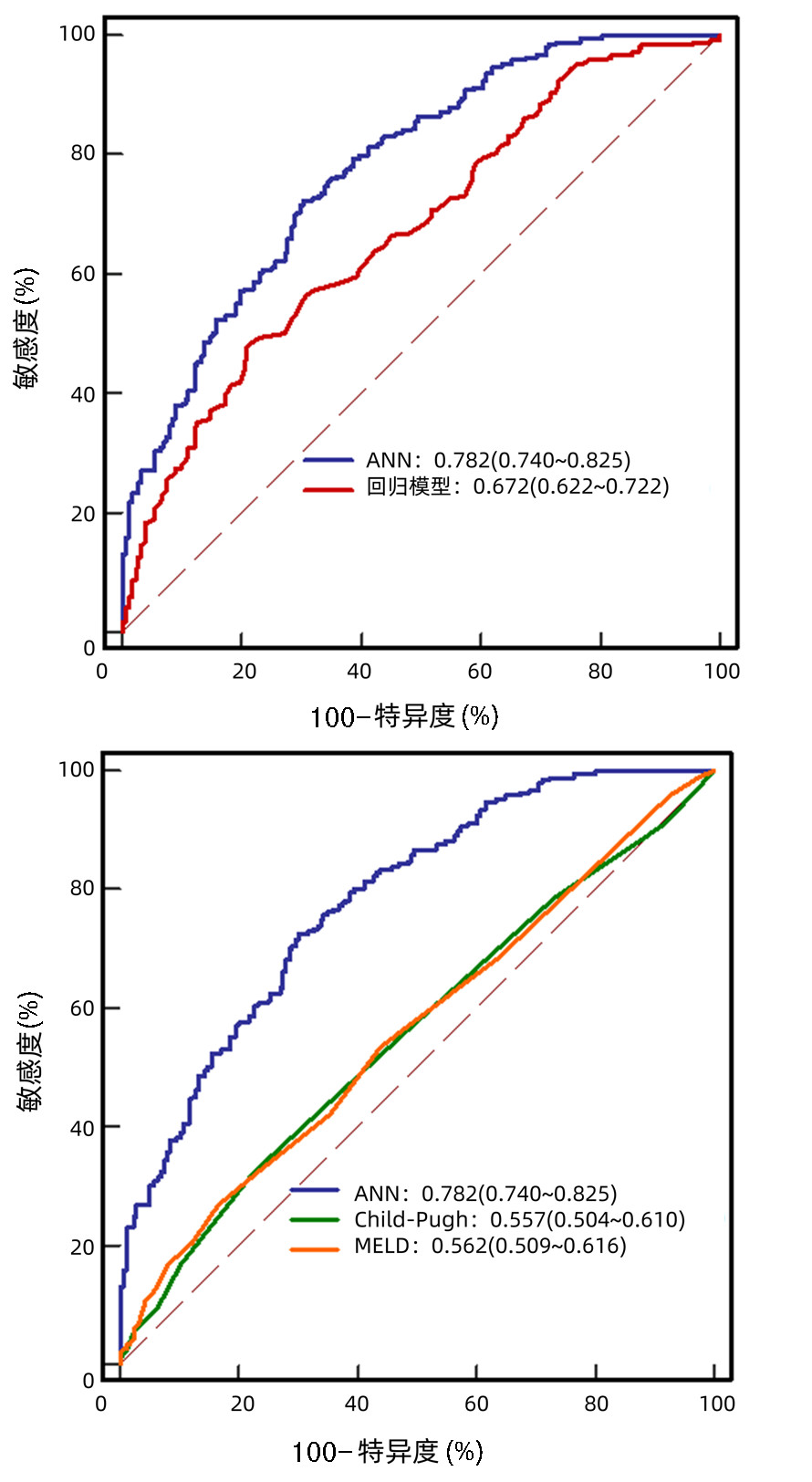
目的 构建可以用来预测肝硬化食管胃底静脉曲张破裂出血患者1年内再出血风险的预测模型。 方法 选取2008年8月—2017年10月于首都医科大学附属北京地坛医院住院的肝硬化食管胃底静脉曲张破裂出血患者441例,并对其进行为期1年的随访观察。以再出血作为研究终点,根据1年内是否发生再出血事件将患者分为再出血组(249例)和未再出血组(192例)。计数资料采用Fisher精确检验或者χ2检验。计量资料符合正态分布两组间比较采用t检验,不符合正态分布的两组间比较采用Mann-Whitney U检验。采用Cox单因素和多因素回归分析影响食管胃底静脉曲张破裂出血患者1年内再出血的独立影响因素,并构建预测模型,利用ROC曲线下面积评估该模型的预测性能。 结果 有249例(56.5%)患者在1年内发生食管胃底静脉曲张破裂再出血事件,Cox多因素分析显示:INR(AHR=1.566,95%CI:1.023~2.398,P=0.039)、NLR(AHR=1.033,95%CI:1.009~1.058,P=0.006)是1年内再出血的独立危险因素;而CHB(AHR=0.769,95%CI:0.597~0.991,P=0.042)、Na(AHR=0.967,95%CI:0.936~0.999,P=0.044)、内镜(AHR=0.829,95%CI:0.743~0.926,P=0.001)及手术治疗(AHR=0.246,95%CI:0.120~0.504,P<0.001)是保护因素。利用上述6个独立影响因素,成功构建了一个人工神经网络模型(https://wangxianbo.math.ink/PoRiEV-zq/index.html),其预测1年内再出血的ROC曲线下面积为0.782(95%CI:0.740~0.825),明显优于Cox回归模型的0.672(95%CI:0.622~0.722,P<0.001)、Child-Pugh评分的0.557(95%CI:0.504~0.610,P<0.001)和MELD评分的0.562(95%CI:0.509~0.616,P<0.001)。 结论 人工神经网络模型具有良好的个体化预测性能,可以作为临床食管胃底静脉曲张破裂再出血的风险评估工具。 Abstract:Objective To develop an artificial neural network model to predict the risk of rebleeding within one year in cirrhotic patients with esophagogastric variceal bleeding. Methods We retrospectively collected 441 cirrhotic patients with esophagogastric variceal bleeding hospitalized at Beijing Ditan Hospital, Capital Medical University, from August 2008 to October 2017. The enrolled patients were followed up for one year. According to the primary endpoint which was rebleeding within one year, patients were divided into rebleeding (249 cases) and non-rebleeding (192 cases) groups. Fisher exact test or chi-square test were used for comparison of categorical data. Comparison of continuous data with normal distribution between groups was performed using t test, while comparison of non-normally distributed data was performed by Mann-Whitney U test. Cox univariate and multivariate regression were used to identify independent factors affecting rebleeding within one year in cirrhotic patients with esophagogastric variceal bleeding, and then an artificial neural network prediction model was constructed using identified factors. The predictive performance of the model was evaluated using the area under the receiver operating characteristic curve (AUC). Results In total, 249 (56.5%) patients developed esophagogastric variceal rebleeding within one year. Cox multivariate regression showed INR (AHR=1.566, 95%CI: 1.023~2.398, P=0.039) and NLR (AHR=1.033, 95%CI: 1.009~1.058, P=0.006) were risk factors for 1-year rebleeding, while CHB (AHR=0.769, 95%CI: 0.597~0.991, P=0.042), Na (AHR=0.967, 95%CI: 0.936~0.999, P=0.044), endoscopic (AHR=0.829, 95%CI: 0.743~0.926, P=0.001) and surgical treatment (AHR=0.246, 95%CI: 0.120~0.504, P < 0.001) were protective factors. Using the above six independent influence factors, we successfully constructed an artificial neural network model (https://lixuan.me/annmodel/myg-v3/). The model's ability to predict 1-year rebleeding had an AUC of 0.782 (95%CI: 0.740-0.825), which was higher than 0.672 (95%CI: 0.622-0.722, P < 0.001) of Cox regression model, 0.557 (95%CI: 0.504-0.610, P < 0.001) of Child-Pugh and 0.562 (95%CI: 0.509-0.616, P < 0.001) of MELD scores. Conclusion The artificial neural network model has good individualized prediction performance and can be used as a risk assessment tool for esophagogastric variceal rebleeding. -
Key words:
- Esophageal and Gastric Varices /
- Hemorrhage /
- Neural Networks(Computer)
-
表 1 肝硬化EVB患者基线特征
Table 1. Baseline characteristics of cirrhotic patients with EVB
指标 所有患者
(n=441)未再出血组
(n=192)再出血组
(n=249)统计值 P值 年龄(岁) 52.46±10.51 52.43±10.81 52.48±10.28 t=0.446 0.505 男/女(例) 309/132 136/56 173/76 χ2=0.095 0.758 病因[例(%)] CHB 251(56.9) 124(64.6) 127(51.0) χ2=8.152 0.004 CHC 44(10.0) 15(7.8) 29(11.6) χ2=1.774 0.183 ALD 122(27.7) 41(21.4) 81(32.5) χ2=6.766 0.009 AIH 26(5.9) 14(7.3) 12(4.8) χ2=1.194 0.274 细菌感染[例(%)] 245(55.6) 100(52.1) 145(58.2) χ2=1.660 0.198 Child-Pugh分级[例(%)] χ2=3.948 0.047 A/B(5~9) 377(85.5) 171(89.1) 206(82.7) C(10~13) 60(13.6) 19(9.9) 41(16.5) MELD评分 10.00(9.00~13.00) 10.00(9.00~12.00) 11.00(9.00~14.00) Z=-2.238 0.025 ALT(U/L) 24.40(17.20~39.40) 24.35(17.23~39.93) 24.40(17.20~39.30) Z=-0.273 0.785 AST(U/L) 30.20(21.65~49.55) 28.75(21.20~48.08) 31.50(22.15~49.75) Z=-0.676 0.499 TBil(μmol/L) 19.50(12.75~31.25) 18.90(12.55~29.75) 20.30(12.85~33.05) Z=-1.162 0.245 GGT(U/L) 8.50(5.50~13.85) 23.10(13.60~46.10) 29.10(15.65~69.70) Z=-2.529 0.011 Alb(g/L) 29.97±5.78 30.17±5.76 29.82±5.80 t=0.006 0.937 Na(mmol/L) 139.0(136.7~141.2) 139.4(137.0~141.3) 138.5(136.2~141.2) Z=-2.056 0.040 Cr(μmol/L) 65.30(52.65~77.50) 64.25(50.93~76.78) 66.00(54.00~78.55) Z=-1.234 0.217 GLU(mmol/L) 8.43(6.72~11.27) 8.00(6.53~10.65) 8.83(6.91~11.63) Z=-2.241 0.217 WBC(×109/L) 4.36(2.92~6.39) 4.19(2.88~6.29) 4.50(2.92~6.50) Z=-1.001 0.317 NLR 4.15(2.71~6.78) 3.85(2.62~6.09) 4.50(2.80~7.42) Z=-2.402 0.016 Hb(g/L) 76.20(59.20~96.00) 76.20(58.55~97.75) 76.20(60.45~95.00) Z=-0.159 0.874 PLT(×109/L) 60.90(43.40~79.00) 59.50(43.25~79.98) 61.00(44.05~79.00) Z=-0.055 0.956 PT(s) 15.30(14.05~17.20) 15.00(13.93~16.80) 15.40(14.15~17.45) Z=-1.721 0.085 INR 1.29(1.18~1.45) 1.27(1.17~1.42) 1.31(1.19~1.49) Z=-2.478 0.013 内镜治疗次数 1.0(1.0~2.0) 2.0(1.0~2.0) 1.0(1.0~3.0) Z=-0.836 0.403 手术治疗[例(%)] 37(8.4) 29(15.1) 8(3.2) χ2=19.944 <0.001 TIPS[例(%)] 6(1.4) 4(2.1) 2(0.8) χ2=1.324 0.411 β受体阻滞剂[例(%)] 24(5.4) 14(7.3) 10(4.0) χ2=0.040 0.841 注:GLU,葡萄糖;NLR,中性粒细胞与淋巴细胞比值;PT,凝血酶原时间;INR,国际标准化比值;TIPS,经颈静脉肝内门体分流术。 表 2 肝硬化EVB患者再出血的Cox单因素和多因素分析
Table 2. Univariate and multivariate Cox analysis with esophagogastric variceal rebleeding
变量 单因素分析 多因素分析 HR(95%CI) P值 AHR(95%CI) P值 年龄(岁) 1.001(0.989~1.013) 0.891 男/女 1.094(0.835~1.433) 0.514 CHB 0.686(0.535~0.880) 0.003 0.769(0.597~0.991) 0.042 CHC 1.330(0.903~1.960) 0.149 ALD 1.356(1.039~1.768) 0.025 AIH 0.732(0.410~1.308) 0.293 细菌感染 1.248(0.970~1.606) 0.084 ALT(U/L) 1.001(1.000~1.002) 0.040 AST(U/L) 1.000(1.000~1.001) 0.105 TBil(μmol/L) 1.004(1.001~1.006) 0.002 GGT(U/L) 1.001(1.000~1.003) 0.076 Alb(g/L) 0.989(0.968~1.011) 0.313 Na(mmol/L) 0.950(0.919~0.982) 0.003 0.967(0.936~0.999) 0.044 Cr(μmol/L) 1.004(1.000~1.007) 0.030 GLU(mmol/L) 1.023(0.999~1.046) 0.056 WBC(×109/L) 1.035(1.012~1.057) 0.002 NLR 1.029(1.009~1.049) 0.004 1.033(1.009~1.058) 0.006 Hb(g/L) 1.000(0.996~1.005) 0.862 PLT(×109/L) 1.001(0.998~1.004) 0.542 PT(s) 1.050(1.012~1.089) 0.010 INR 1.947(1.273~2.977) 0.002 1.566(1.023~2.398) 0.039 内镜治疗次数 0.863(0.775~0.961) 0.007 0.829(0.743~0.926) 0.001 手术治疗 0.261(0.129~0.527) <0.001 0.246(0.120~0.504) <0.001 TIPS 0.422(0.105~1.698) 0.225 β受体阻滞剂 0.998(0.582~1.711) 0.994 -
[1] HOLSTER IL, TJWA ET, MOELKER A, et al. Covered transjugular intrahepatic portosystemic shunt versus endoscopic therapy+β-blocker for prevention of variceal rebleeding[J]. Hepatology, 2016, 63(2): 581-589. DOI: 10.1002/hep.28318. [2] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Endoscopy, Chinese Medical Association. Guidelines for the diagnosis and treatment of esophageal and gastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2016, 32(2): 203-219. DOI: 10.3969/j.issn.1001-5256.2016.02.002.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2016, 32(2): 203-219. DOI: 10.3969/j.issn.1001-5256.2016.02.002. [3] VERDA D, PARODI S, FERRARI E, et al. Analyzing gene expression data for pediatric and adult cancer diagnosis using logic learning machine and standard supervised methods[J]. BMC Bioinformatics, 2019, 20(Suppl 9): 390. DOI: 10.1186/s12859-019-2953-8. [4] CHI S, TIAN Y, WANG F, et al. A novel lifelong machine learning-based method to eliminate calibration drift in clinical prediction models[J]. Artif Intell Med, 2022, 125: 102256. DOI: 10.1016/j.artmed.2022.102256. [5] GARCIA-TSAO G, SANYAL AJ, GRACE ND, et al. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis[J]. Hepatology, 2007, 46(3): 922-938. DOI: 10.1002/hep.21907. [6] PUGH RN, MURRAY-LYON IM, DAWSON JL, et al. Transection of the oesophagus for bleeding oesophageal varices[J]. Br J Surg, 1973, 60(8): 646-649. DOI: 10.1002/bjs.1800600817. [7] FONG TV, HUNG FC, CHIU KW, et al. Model for end-stage liver disease (MELD) score for predicting late esophageal varices rebleeding in cirrhotic patients[J]. Hepatogastroenterology, 2008, 55(84): 1055-1058. [8] DING RH, HU YM, LI XG, et al. Current status of prevention and treatment of esophagogastric variceal bleeding in cirrhotic portal hypertension patients in Ningxia region: a multicenter study[J]. Chin J Dig Surg, 2021, 20(10): 1078-1084. DOI: 10.3760/cma.j.cn115610-20210928-00464.丁荣华, 胡燕梅, 李小果, 等. 宁夏地区肝硬化门静脉高压食管胃底静脉曲张出血防治现状的多中心研究[J]. 中华消化外科杂志, 2021, 20(10): 1078-1084. DOI: 10.3760/cma.j.cn115610-20210928-00464. [9] DENG SM, ZHANG JX, QI Y, et al. Study on the application of endoscopic ligation in esophageal varices and the risk factors of postoperative rebleeding[J]. Chin J Med Offic, 2021, 49(6): 718-720. DOI: 10.16680/j.1671-3826.2021.06.43.邓水苗, 张嘉星, 齐晔, 等. 内镜下套扎术在食管静脉曲张中应用及其术后再出血高危因素研究[J]. 临床军医杂志, 2021, 49(6): 718-720. DOI: 10.16680/j.1671-3826.2021.06.43. [10] HAO Y, TAN P, ZHAO YG, et al. Antibiotic prophylaxis in gastroesophageal variceal bleeding: A prospective study[J]. J Pract Hepatol, 2012, 15(1): 29-31. DOI: 10.3969/j.issn.1672-5069.2012.01.010.郝勇, 谭萍, 赵亚刚, 等. 肝硬化食管胃底静脉曲张出血患者预防性抗菌治疗的前瞻性研究[J]. 实用肝脏病杂志, 2012, 15(1): 29-31. DOI: 10.3969/j.issn.1672-5069.2012.01.010. [11] YANG H, LIU YX, LI P, et al. Analysis of risk factors for early rebleeding from esophageal and gastric varices in patients with liver cirrhosis[J]. J Clin Hepatol, 2014, 30(6): 540-542. DOI: 10.3969/j.issn.1001-5256.2014.06.18.杨花, 刘云霞, 李鹏, 等. 肝硬化患者食管胃底静脉曲张破裂早期再出血的危险因素分析[J]. 临床肝胆病杂志, 2014, 30(6): 540-542. DOI: 10.3969/j.issn.1001-5256.2014.06.18. [12] LIU X, HE L, HAN J, et al. Association of neutrophil-lymphocyte ratio and T lymphocytes with the pathogenesis and progression of HBV-associated primary liver cancer[J]. PLoS One, 2017, 12(2): e0170605. DOI: 10.1371/journal.pone.0170605. [13] PLEVRIS JN, DHARIWAL A, ELTON RA, et al. The platelet count as a predictor of variceal hemorrhage in primary biliary cirrhosis[J]. Am J Gastroenterol, 1995, 90(6): 959-961. [14] CHEN LH, HU NZ, WANG YL. The value of MESO (MELD/Na index) scoring system in predicting prognosis of patients with cirrhosis[J]. J Clin Hepatol, 2011, 27(10): 1044-1046, 1054. DOI: 10.3969/j.issn.1001-5256.2011.10.008.陈丽红, 胡乃中, 王亚雷. 终末期肝病模型与血清钠比值在肝硬化患者预后判断中的价值[J]. 临床肝胆病杂志, 2011, 27(10): 1044-1046, 1054. DOI: 10.3969/j.issn.1001-5256.2011. 10.008. [15] HONG JB, LYU NH, WANG AJ, et al. Analysis of the risk factors for early rebleeding in oesophageal and gastric varices[J]. Chin J Dig, 2010, 30(11): 836-837. DOI: 10.3760/cma.j.issn.0254-1432.2010.11.013.洪军波, 吕农华, 汪安江, 等. 食管胃静脉曲张早期再出血的危险因素分析[J]. 中华消化杂志, 2010, 30(11): 836-837. DOI: 10.3760/cma.j.issn.0254-1432.2010.11.013. [16] HUO TI, LIN HC, WU JC, et al. Proposal of a modified Child-Turcotte-Pugh scoring system and comparison with the model for end-stage liver disease for outcome prediction in patients with cirrhosis[J]. Liver Transpl, 2006, 12(1): 65-71. DOI: 10.1002/lt.20560. [17] KAMATH PS, WIESNER RH, MALINCHOC M, et al. A model to predict survival in patients with end-stage liver disease[J]. Hepatology, 2001, 33(2): 464-470. DOI: 10.1053/jhep.2001.22172. [18] HEUMAN DM, ABOU-ASSI SG, HABIB A, et al. Persistent ascites and low serum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death[J]. Hepatology, 2004, 40(4): 802-810. DOI: 10.1002/hep.20405. [19] ANGELI P, WONG F, WATSON H, et al. Hyponatremia in cirrhosis: Results of a patient population survey[J]. Hepatology, 2006, 44(6): 1535-1542. DOI: 10.1002/hep.21412. -



 PDF下载 ( 2385 KB)
PDF下载 ( 2385 KB)


 下载:
下载: