标准胰颈横断下胰腺断面结构参数对胰十二指肠切除术后胰瘘的预测价值
DOI: 10.3969/j.issn.1001-5256.2022.12.022
Value of pancreatic anatomic structure under standard pancreatic neck transection in predicting pancreatic fistula after pancreaticoduodenectomy
-
摘要:
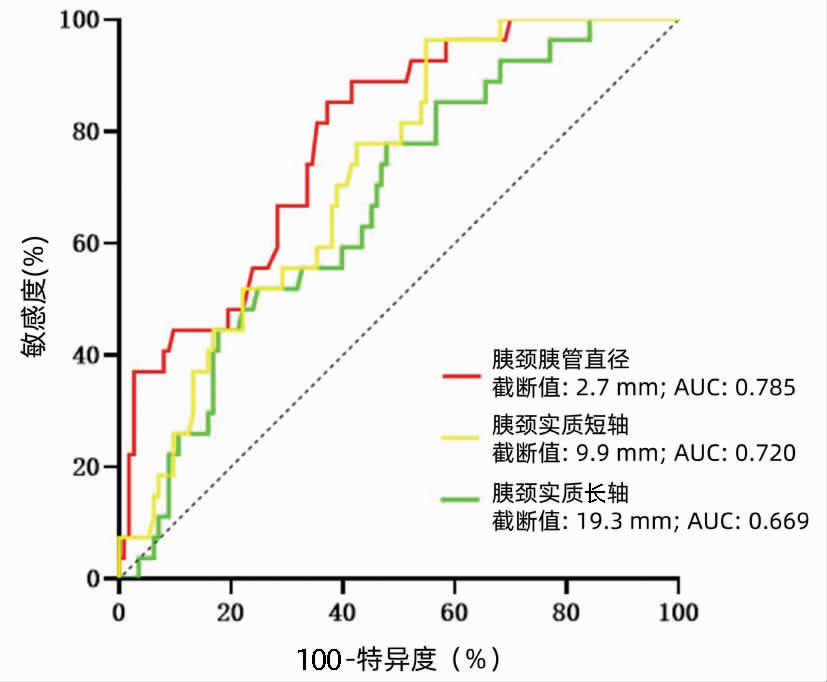
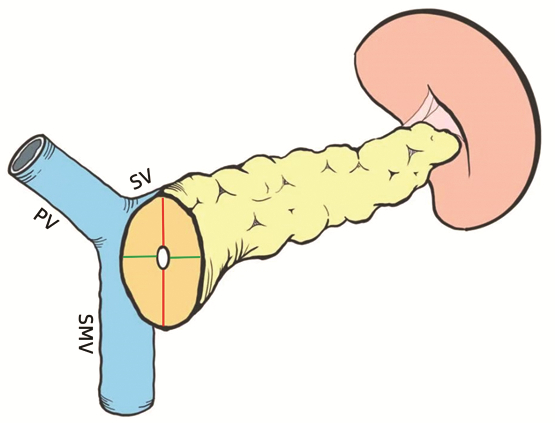
目的 探究标准胰颈横断下胰腺断面结构相关参数对胰瘘预测作用,并验证。 方法 回顾性收集2016年6月—2019年12月在中国人民解放军西部战区总医院行胰十二指肠切除术(PD)的患者140例作为预测组;2020年1月—2021年3月在中国人民解放军西部战区总医院行PD手术的患者82例为验证组。比较两组基线水平,通过预测组单因素分析筛选胰瘘危险因素,在验证组采用组内相关系数比较术前影像学与术中实际测量值的一致性,并分组验证胰瘘危险因素。符合正态分布的计量资料组间比较采用t检验;偏态分布的计量资料组间比较采用Mann-Whitney U检验。计数资料组间比较采用χ2检验。采用单因素Logistic分析筛选胰瘘危险因素。计算约登指数,GraphPad Prism绘制受试者工作特征曲线,计算受试者工作特征曲线下面积(AUC)。对术前影像测量值与术中实际测量值采用组内相关系数进行可靠性分析。 结果 胰颈胰管直径(OR=0.347,95%CI:0.192~0.626,P<0.001)、胰颈实质长轴(OR=1.127,95%CI:1.031~1.231,P=0.008)及胰颈实质短轴(OR=1.350,95%CI:1.137~1.602,P=0.001)具有显著差异。胰颈胰管直径AUC=0.785(95%CI:0.128~0.302,P<0.001)、截断值为2.7 mm;胰颈实质长轴AUC=0.669(95%CI:0.564~0.774,P=0.006)、截断值为19.3 mm;胰颈实质短轴AUC=0.720(95%CI:0.627~0.813,P<0.001)、截断值为9.9 mm。验证组30例患者中,术前影像测量值与术中实际测量值具有高度一致性,组内相关系数均>0.75,P<0.001。截断值分组验证,以胰颈胰管直径划分的高危组与低危组之间胰瘘发生率存在显著差异(χ2=0.645,P=0.011);胰颈实质短轴划分的两组之间胰瘘发生率差异显著(χ2=5.901,P=0.015)。 结论 标准胰颈横断下胰颈断面结构特征是胰瘘发生的危险因素,通过术前CT影像可进行判别,方法在临床上简单易行。 Abstract:Objective To investigate and validate the effect of relevant parameters of pancreatic anatomic structure under standard pancreatic neck transection in predicting postoperative pancreatic fistula (POPF). Methods A total of 140 patients who underwent pancreaticoduodenectomy (PD) in The General Hospital of Western Theater Command from June 2016 to December 2019 were enrolled as prediction group, and 82 patients who underwent PD in the same hospital from January 2020 to March 2021 were enrolled as validation group. Baseline levels were compared between the two groups. A univariate analysis was performed for the prediction group to screen out the risk factors for POPF, and in the validation group, the interclass correlation coefficient (ICC) was used to compare the consistency between preoperative imaging measurements and actual intraoperative measurements. The risk factors for POPF were validated in each group. The t-test was used for comparison of normally distributed continuous data between groups, and the Mann-Whitney U test was used for comparison of continuous data with skewed distribution between groups; the chi-square test was used for comparison of categorical data between groups. The multivariate logistic regression analysis was used to investigate the risk factors for POPF. Youden index was calculated, GraphPad Prism was used to plot the receiver operating characteristic (ROC) curve, and the area under the ROC curve (AUC) was calculated. ICC was used for the reliability analysis of preoperative imaging measurements and actual intraoperative measurements. Results Pancreatic duct diameter at the pancreatic neck (odds ratio [OR]=0.347, 95% confidence interval [CI]: 0.192-0.626, P < 0.001), the major axis of the pancreatic neck parenchyma (OR=1.127, 95%CI: 1.031-1.231, P=0.008), and the minor axis of the pancreatic neck parenchyma (OR=1.350, 95% CI: 1.137-1.602, P=0.001) were risk factors for POPF. Pancreatic duct diameter at the pancreatic neck had an AUC of 0.785 (95%CI: 0.128-0.302, P < 0.001) and a cut-off value of 2.7 mm; the major axis of the pancreatic neck parenchyma had an AUC of 0.669 (95%CI: 0.564-0.774, P=0.006) and a cut-off value of 19.3 mm, and the minor axis of the pancreatic neck parenchyma had an AUC of 0.720 (95%CI: 0.627-0.813, P < 0.001) and a cut-off value of 9.9 mm. Preoperative imaging measurements were highly consistent with actual intraoperative measurements for 30 patients in the validation group, with an ICC of > 0.75 (P < 0.001). Grouping validation of cut-off values showed that there was a significant different in the incidence rate of POPF between the high-risk group and the low-risk group based on pancreatic duct diameter at the pancreatic neck (χ2=0.645, P=0.011), as well as between the high-risk group and the low-risk group based on the minor axis of the pancreatic neck parenchyma (χ2=5.901, P=0.015). Conclusion Structural features of the pancreatic neck under standard pancreatic neck transection are risk factors for POPF, which can be differentiated by preoperative CT, and the method is easy and convenient in clinical practice. -
Key words:
- Pancreaticoduodenectomy /
- Pancreatic Fistula /
- Forecasting
-
表 1 两组基线水平和围手术期资料对比
Table 1. Comparison of baseline and perioperative data between two groups
变量 总计(n=222) 预测组(n=140) 验证组(n=82) 统计值 P值 年龄(岁) 60.0(51.0~66.0) 59.5(51.0~65.0) 60.0(51.0~67.0) Z=-1.161 0.246 性别[例(%)] χ2=0.753 0.385 男 138(62.2) 84(60.0) 54(65.9) 女 84(37.8) 56(40.0) 28(34.1) BMI(kg/m2) 22.3±3.1 22.5±3.1 22.0±3.1 t=1.305 0.193 体质量下降(kg) 0(0~5.0) 0(0~5.0) 0(0~5.0) Z=-0.086 0.932 吸烟史[例(%)] 85(38.3) 54(38.6) 31(37.8) χ2=0.013 0.910 饮酒史[例(%)] 71(32.0) 43(30.7) 28(34.1) χ2=0.280 0.597 高血压[例(%)] 40(18.0) 27(19.3) 13(15.9) χ2=0.412 0.521 糖尿病[例(%)] 33(14.9) 18(12.9) 15(18.3) χ2=1.207 0.272 ASA分级[例(%)] χ2=0.971 0.325 Ⅰ~Ⅱ 203(91.4) 130(92.9) 73(89.0) Ⅲ 19(8.6) 10(7.1) 9(11.0) 术前[例(%)] 总胆红素(μmol/L) 149.0(41.6~240.5) 172.9(56.1~245.4) 131.6(19.8~228.3) Z=-1.443 0.149 CA19-9(U/mL) 69.0(21.9~244.0) 87.4(28.1~262.4) 48.2(13.5~226.1) Z=-1.759 0.079 C反应蛋白(mg/L) 32.4(5.8~89.0) 41.9(8.0~90.2) 23.4(3.4~90.1) Z=-1.837 0.066 白蛋白(g/L) 40.4±4.0 40.6±3.9 40.0±4.1 t=1.163 0.246 血红蛋白 125.8±17.7 127.0±18.7 123.8±15.5 t=1.300 0.195 手术方式[例(%)] χ2=0.243 0.622 腹腔镜 66(29.7) 40(28.6) 26(31.7) 开腹 156(70.3) 100(71.4) 56(68.3) 手术时间(min) 437.6±118.9 445.8±117.8 422.8±116.0 t=1.350 0.178 失血量(mL) 400.0(300.0~500.0) 400.0(300.0~500.0) 300.0(200.0~500.0) Z=-1.187 0.235 输血量(mL) 0(0~700.0) 0(0~700.0) 0(0~500.0) Z=-0.989 0.323 术后住院时间(d) 15.0(12.0~21.0) 15.0(12.0~21.0) 15(13.0~21.0) Z=-0.090 0.928 术后病理[例(%)] χ2=0.166 0.920 胰腺癌 51(23.0) 32(22.8) 19(23.2) 胆总管下段癌 97(43.7) 60(42.9) 37(45.1) 十二指肠癌 74(33.3) 48(34.3) 26(31.7) 注:ASA分级,美国麻醉医师协会分级。 表 2 预测组临床相关性胰瘘的单因素分析
Table 2. univariate analysis of CR-POPF in prediction group
变量 OR值 95%CI P值 年龄(岁) 0.967 0.922~1.013 0.157 性别 0.702 0.290~1.698 0.433 BMI(kg/m2) 1.017 0.888~1.165 0.810 体质量下降(kg) 1.019 0.902~1.151 0.762 吸烟史 1.084 0.455~2.582 0.855 饮酒史 0.473 0.199~1.122 0.089 高血压 0.799 0.287~2.224 0.667 糖尿病 2.405 0.811~7.130 0.114 ASA分级 2.250 0.273~18.562 0.451 Ⅰ~Ⅱ Ⅲ 总胆红素(μmol/L) 1.001 0.996~1.006 0.653 CA199(U/mL) 1.000 1.000~1.000 0.306 C反应蛋白(mg/L) 1.004 0.998~1.010 0.235 白蛋白(g/L) 0.935 0.842~1.037 0.204 手术方式 1.179 0.455~3.052 0.735 手术时间(min) 0.999 0.995~1.003 0.530 失血量(mL) 1.000 0.998~1.002 0.969 输血量(mL) 1.001 1.000~1.001 0.138 胰颈胰管直径(mm) 0.347 0.192~0.626 <0.001 胰颈长轴(mm) 1.069 0.973~1.174 0.165 胰颈短轴(mm) 1.118 0.943~1.324 0.200 胰颈实质长轴(mm) 1.127 1.031~1.231 0.008 胰颈实质短轴(mm) 1.350 1.137~1.602 0.001 表 3 术前影像测量值与术中实际测量值的一致性分析
Table 3. Consistency analysis between preoperative imaging measurements and intraoperative actual measurements
变量 术前影像测量值 术中实际测量值 ICC值 P值 胰颈胰管直径(mm) 4.7±2.4 4.5±2.1 0.945 <0.001 胰颈长轴(mm) 22.7±4.2 23.1±4.7 0.970 <0.001 胰颈短轴(mm) 14.2±2.9 14.0±2.7 0.947 <0.001 胰颈实质长轴(mm) 18.0±5.3 18.5±5.3 0.967 <0.001 胰颈实质短轴(mm) 9.5±3.4 9.5±3.0 0.926 <0.001 表 4 胰颈胰管直径及胰颈实质验证
Table 4. Verification of diameter of pancreatic neck duct and pancreatic neck parenchyma
变量 总计(n=82) 无CR-POPF组
(n=67)CR-POPF组
(n=15)χ2值 P值 胰颈胰管直径[例(%)] 6.457 0.011 >2.7 mm 46(56.1) 42(62.7) 4(26.7) ≤2.7 mm 36(43.9) 25(37.3) 11(73.3) 胰颈实质长轴[例(%)] 3.394 0.065 ≥19.3 mm 32(39.0) 23(34.3) 9(60.0) <19.3 mm 50(61.0) 44(65.7) 6(40.0) 胰颈实质短轴[例(%)] 5.901 0.015 ≥9.9 mm 37(45.1) 26(38.8) 11(73.3) <9.9 mm 45(54.9) 41(61.2) 4(26.7) -
[1] SHINDE RS, ACHARYA R, CHAUDHARI VA, et al. External validation and comparison of the original, alternative and updated-alternative fistula risk scores for the prediction of postoperative pancreatic fistula after pancreatoduodenectomy[J]. Pancreatology, 2020, 20(4): 751-756. DOI: 10.1016/j.pan.2020.04.006. [2] CASCIANI F, BASSI C, VOLLMER CM Jr. Decision points in pancreatoduodenectomy: Insights from the contemporary experts on prevention, mitigation, and management of postoperative pancreatic fistula[J]. Surgery, 2021, 170(3): 889-909. DOI: 10.1016/j.surg.2021.02.064. [3] DONG Q, LIU X, ZHANG RJ, et al. The influence of bundled ligation of the pancreatic stump on postoperative pancreatic fistula of distal pancreatectomy[J]. Chin J Dig Surg, 2021, 20(4): 419-424. DOI: 10.3760/cma.j.cn115610-20210203-00061.董勤, 刘旭, 张瑞坚, 等. 胰腺残端捆绑结扎对胰腺远端切除术后胰瘘的影响[J]. 中华消化外科杂志, 2021, 20(4): 419-424. DOI: 10.3760/cma.j.cn115610-20210203-00061. [4] GAO HQ, LI BY, MA YS, et al. Risk factors analysis and treatment of postpancreaticoduodenectomy hemorrhage[J]. Chin J Dig Surg, 2022, 21(4): 492-499. DOI: 10.3760/cma.j.cn115610-20220228-00111.高红桥, 李宝毅, 马永蔌, 等. 胰十二指肠切除术后出血的危险因素分析及治疗策略[J]. 中华消化外科杂志, 2022, 21(4): 492-499. DOI: 10.3760/cma.j.cn115610-20220228-00111. [5] PEDRAZZOLI S, BRAZZALE AR. Systematic review and meta-analysis of surgical drain management after the diagnosis of postoperative pancreatic fistula after pancreaticoduodenectomy: draining-tract-targeted works better than standard management[J]. Langenbecks Arch Surg, 2020, 405(8): 1219-1231. DOI: 10.1007/s00423-020-02005-8. [6] LAO M, ZHANG X, GUO C, et al. External validation of alternative fistula risk score (a-FRS) for predicting pancreatic fistula after pancreatoduodenectomy[J]. HPB (Oxford), 2020, 22(1): 58-66. DOI: 10.1016/j.hpb.2019.05.007. [7] YU J, REN CY, WANG J, et al. Establishment of risk prediction model of postoperative pancreatic fistula after pancreatoduodenectomy: 2016 edition of definition and grading system of pancreatic fistula: a single center experience with 223 cases[J]. World J Surg Oncol, 2021, 19(1): 257. DOI: 10.1186/s12957-021-02372-6. [8] ZHANG B, YUAN Q, LI S, et al. Risk factors of clinically relevant postoperative pancreatic fistula after pancreaticoduodenectomy: A systematic review and meta-analysis[J]. Medicine (Baltimore), 2022, 101(26): e29757. DOI: 10.1097/MD.0000000000029757. [9] ROBERTS KJ, KARKHANIS S, PITCHAIMUTHU M, et al. Comparison of preoperative CT-based imaging parameters to predict postoperative pancreatic fistula[J]. Clin Radiol, 2016, 71(10): 986-992. DOI: 10.1016/j.crad.2016.06.108. [10] SUGIMOTO M, KENDRICK ML, FARNELL MB, et al. Relationship between pancreatic thickness and staple height is relevant to the occurrence of pancreatic fistula after distal pancreatectomy[J]. HPB (Oxford), 2020, 22(3): 398-404. DOI: 10.1016/j.hpb.2019.07.010. [11] WATANABE N, YAMAMOTO Y, SUGIURA T, et al. The impact of stump closure techniques on pancreatic fistula stratified by the thickness of the pancreas in distal pancreatectomy[J]. Dig Surg, 2020, 37(4): 340-347. DOI: 10.1159/000505061. [12] BOX EW, DENG L, MORGAN DE, et al. Preoperative anthropomorphic radiographic measurements can predict postoperative pancreatic fistula formation following pancreatoduodenectomy[J]. Am J Surg, 2021, 222(1): 133-138. DOI: 10.1016/j.amjsurg.2020.10.023. [13] TAJIMA Y, KAWABATA Y, HIRAHARA N. Preoperative imaging evaluation of pancreatic pathologies for the objective prediction of pancreatic fistula after pancreaticoduodenectomy[J]. Surg Today, 2018, 48(2): 140-150. DOI: 10.1007/s00595-017-1529-3. [14] DATTA J, WILLOBEE BA, RYON EL, et al. Contemporary reappraisal of intraoperative neck margin assessment during pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: a review[J]. JAMA Surg, 2021, 156(5): 489-495. DOI: 10.1001/jamasurg.2020.5676. [15] BASSI C, MARCHEGIANI G, DERVENIS C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After[J]. Surgery, 2017, 161(3): 584-591. DOI: 10.1016/j.surg.2016.11.014. [16] HVTTNER FJ, FITZMAURICE C, SCHWARZER G, et al. Pylorus-preserving pancreaticoduodenectomy (pp Whipple) versus pancreaticoduodenectomy (classic Whipple) for surgical treatment of periampullary and pancreatic carcinoma[J]. Cochrane Database Syst Rev, 2016, 2: CD006053. DOI: 10.1002/14651858.CD006053.pub6. [17] SKANDALAKIS LJ, ROWE JS Jr, GRAY SW, et al. Surgical embryology and anatomy of the pancreas[J]. Surg Clin North Am, 1993, 73(4): 661-697. DOI: 10.1016/s0039-6109(16)46080-9. [18] BARDOL T, DELICQUE J, HERMIDA M, et al. Neck transection level and postoperative pancreatic fistula after pancreaticoduodenectomy: A retrospective cohort study of 195 patients[J]. Int J Surg, 2020, 82: 43-50. DOI: 10.1016/j.ijsu.2020.08.001. [19] RENBERG S, ZHANG Y, KARLSSON F, et al. The role of neoadjuvant imatinib in gastrointestinal stromal tumor patients: 20 years of experience from a tertial referral center[J]. Int J Cancer, 2022, 151(6): 906-913. DOI: 10.1002/ijc.34052. [20] YOU L, ZHAO W, HONG X, et al. The effect of body mass index on surgical outcomes in patients undergoing pancreatic resection: a systematic review and meta-analysis[J]. Pancreas, 2016, 45(6): 796-805. DOI: 10.1097/MPA.0000000000000525. [21] ZARZAVADJIAN LE BIAN A, FUKS D, MONTALI F, et al. Predicting the severity of pancreatic fistula after pancreaticoduodenectomy: overweight and blood loss as independent risk factors: retrospective analysis of 277 patients[J]. Surg Infect (Larchmt), 2019, 20(6): 486-491. DOI: 10.1089/sur.2019.027. [22] SHIMIZU A, TANI M, KAWAI M, et al. Influence of visceral obesity for postoperative pulmonary complications after pancreaticoduodenectomy[J]. J Gastrointest Surg, 2011, 15(8): 1401-1410. DOI: 10.1007/s11605-011-1436-7. [23] GRUPPO M, ANGRIMAN I, MARTELLA B, et al. Perioperative albumin ratio is associated with post-operative pancreatic fistula[J]. ANZ J Surg, 2018, 88(7-8): e602-e605. DOI: 10.1111/ans.14262. [24] SAKAMOTO T, YAGYU Y, UCHINAKA EI, et al. Predictive significance of c-reactive protein-to-albumin ratio for postoperative pancreatic fistula after pancreaticoduodenectomy[J]. Anticancer Res, 2019, 39(11): 6283-6290. DOI: 10.21873/anticanres.13838. [25] TEMPERO MA, MALAFA MP, CHIOREAN EG, et al. Pancreatic adenocarcinoma, version 1.2019[J]. J Natl Compr Canc Netw, 2019, 17(3): 202-210. DOI: 10.6004/jnccn.2019.0014. [26] NISHIDA Y, KATO Y, KUDO M, et al. Preoperative sarcopenia strongly influences the risk of postoperative pancreatic fistula formation after pancreaticoduodenectomy[J]. J Gastrointest Surg, 2016, 20(9): 1586-1594. DOI: 10.1007/s11605-016-3146-7. [27] MU W, LIU C, GAO F, et al. Prediction of clinically relevant Pancreatico-enteric Anastomotic Fistulas after Pancreatoduodenectomy using deep learning of Preoperative Computed Tomography[J]. Theranostics, 2020, 10(21): 9779-9788. DOI: 10.7150/thno.49671. [28] BARBIER L, MÈGE D, REYRE A, et al. Predict pancreatic fistula after pancreaticoduodenectomy: ratio body thickness/main duct[J]. ANZ J Surg, 2018, 88(5): E451-E455. DOI: 10.1111/ans.14048. [29] PARTELLI S, ANDREASI V, SCHIAVO LENA M, et al. The role of acinar content at pancreatic resection margin in the development of postoperative pancreatic fistula and acute pancreatitis after pancreaticoduodenectomy[J]. Surgery, 2021, 170(4): 1215-1222. DOI: 10.1016/j.surg.2021.03.047. [30] NAKAMURA H, MURAKAMI Y, UEMURA K, et al. Reduced pancreatic parenchymal thickness indicates exocrine pancreatic insufficiency after pancreatoduodenectomy[J]. J Surg Res, 2011, 171(2): 473-478. DOI: 10.1016/j.jss.2010.03.052. [31] STEGER U, RANGE P, MAYER F, et al. Pancreatic duct anatomy in the corpus area: implications for closure and anastomotic technique in pancreas surgery[J]. Langenbecks Arch Surg, 2010, 395(3): 201-206. DOI: 10.1007/s00423-009-0526-4. [32] UMEZAKI N, HASHIMOTO D, NAKAGAWA S, et al. Number of acinar cells at the pancreatic stump predicts pancreatic fistula after pancreaticoduodenectomy[J]. Surg Today, 2018, 48(8): 790-795. DOI: 10.1007/s00595-018-1656-5. -



 PDF下载 ( 2420 KB)
PDF下载 ( 2420 KB)

 下载:
下载: