我国一般人群原发性胆汁性胆管炎患病率及其影响因素的系统综述
DOI: 10.3969/j.issn.1001-5256.2023.02.011
Prevalence of primary biliary cholangitis in the Chinese general population and its influencing factors: A systematic review
-
摘要:
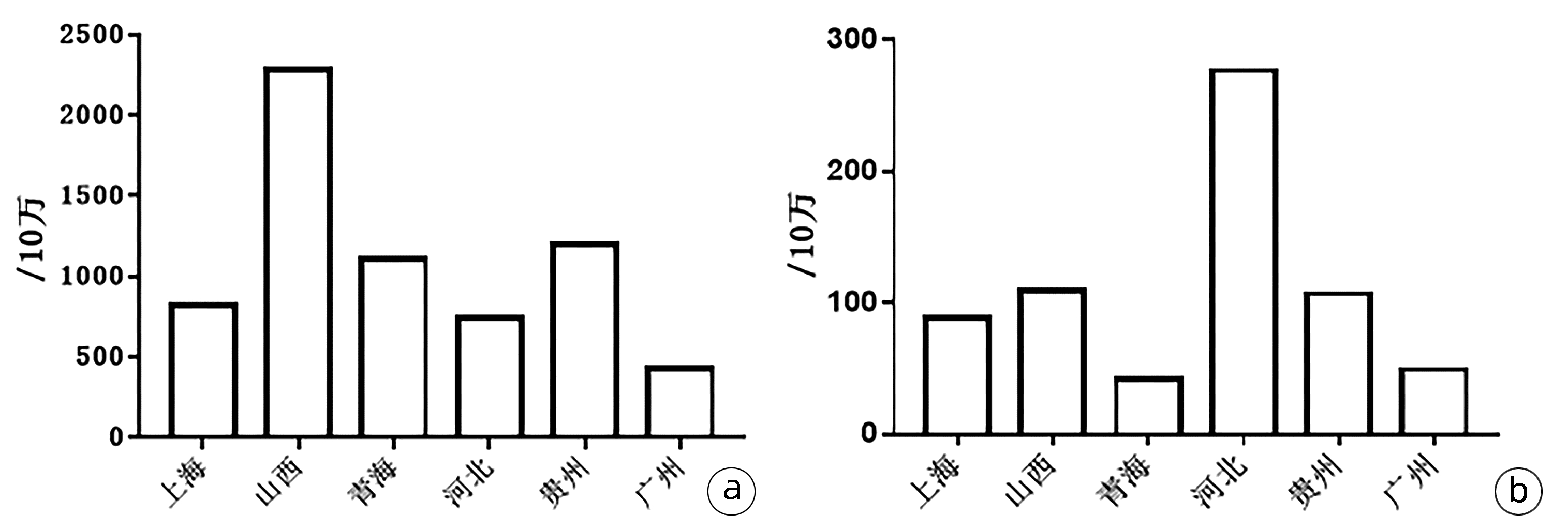
目的 系统回顾原发性胆汁性胆管炎(PBC)流行病学研究,了解中国一般人群PBC的患病率及其影响因素。 方法 检索PubMed、Embase、The Cochrane Library、CNKI和万方自建库至2022年3月31日发表的有关我国PBC流行病学研究文献。2位研究者独立筛选文献、提取资料,然后进行分析。 结果 共纳入9篇研究文献。AMA阳性率及PBC患病率分别为1 049.05/10万(范围159.65/10万~2 287.40/10万)和123.68/10万(范围42.70/10万~276.59/10万)。AMA阳性率在男女中分别为636.51/10万(范围52.55/10万~1 164.33/10万)和1 265.47/10万(范围225.23/10万~1 704.93/10万),AMA患病率男女比为1∶1.99。PBC患病率在男女中分别为40.81/10万(范围23.54/10万~75.10/10万)和148.71/10万(范围77.36/10万~214.91/10万),PBC患病率男女比为1∶3.64。 结论 不同研究我国一般人群AMA阳性率及PBC患病率差别较大,其主要受年龄、性别及地区影响。从整体看,AMA阳性率及PBC患病率随年龄增大而增大,年龄≥50岁AMA阳性率明显高于年龄<50岁。AMA阳性率远高于PBC患病率。AMA阳性人群和PBC患者女性明显多于男性,性别对AMA的影响小于其对PBC的影响。 Abstract:Objective To systematically review the epidemiological studies on primary biliary cholangitis (PBC), and to investigate the prevalence rate of PBC in the Chinese general population and its influencing factors. Methods PubMed, Embase, The Cochrane Library, CNKI, and Wanfang Data were searched for articles on the epidemiology of PBC in China published up to 31th March 2022. Two researchers independently performed screening and data extraction, and then related analyses were performed. Results A total of 9 articles were included. The positive rate of AMA was 1 049.05/100 000 (ranging fr om 159.65/100 000 to 2287.40/100 000), and the prevalence rate of PBC was 123.68/100 000 (ranging from 42.70/100 000 to 276.59/100 000). The positive rate of AMA was 636.51/100 000 (ranging from 52.55/100 000 to 1 164.33/100 000) in men and 1 265.47/100 000 (ranging from 225.23/100 000 to 1 704.93/100 000) in women, with a male/female ratio of 1∶1.99 for the prevalence rate of AMA. The prevalence rate of PBC was 40.81/100 000 (ranging from 23.54/100 000 to 75.10/100 000) in men and 148.71/100 000 (ranging from 77.36/100 000 to 214.91/100 000) in women, with a male/female ratio of 1∶3.64 for the prevalence rate of PBC. Conclusion Different studies show great differences in the positive rate of AMA and the prevalence rate of PBC in the Chinese general population, which is mainly affected by sex, age, and region. The positive rate of AMA and the prevalence rate of PBC increase with age, and the patients aged ≥50 years have a significantly higher positive rate of AMA than those aged < 50 years. The positive rate of AMA is significantly higher than the prevalence rate of PBC. There are significantly more women than men in the AMA-positive population and the PBC patients, and the influence of sex on AMA is lower than that on PBC. -
Key words:
- Primary Biliary Cholangitis /
- Epidemiology /
- Prevalence
-
表 1 纳入文献的基本特征
Table 1. Characteristics of included studies
第一作者 发表年份 收集病例年份 地区 AMA-M2阳性例数(男/女) AMA-M2阳性率(男/女,10万) 不同年龄段AMA-M2阳性率 Jiang等[12] 2003 2000 上海 8(1/7) 159.65(52.55/225.23) - Liu等[13] 2010 2006 广州 35(15/20) 430.72(353.11/515.73) - 郭亚平等[15] 2014 2011 河北 156(32/124) 743.92(303.32/1 190.02) - Chen等[11] 2016 2013 上海 133(33/100) 699.56(397.11/934.40) 18~49岁: 16.9 (0/41.5);
50~59岁: 1 740.5 (714.3/2 251.2);
60~69岁: 578.9 (161.2/856.2);
70~79岁: 1 147.4 (942.8/1 219.5);
80~89岁: 1 187.9 (1 077.6/1 243.2);
≥90岁: 1574.8 (3 225.8/621.1)叶震璇等[18] 2018 2015 贵州 438(135/303) 1 201.35(722.43/1 704.93) ≤ 40岁: 739.3;
41~60岁: 1 363.5;
≥ 61岁: 2 601.0;刘晓萍等[16] 2018 2015 山西 209(-) 2 287.40 - 瞿国英等[17] 2018 2017 上海 175(69/106) 1 075.93(843.73/1 310.75) ≤ 30岁: 18.45(0/36.97);
31~45岁: 1 083.27(901.19/1 267.06);
46~60岁: 1 831.79(1 567.23/2 107.48);
≥ 61岁: 4 597.70(2 652.52/6 403.94)郑佳等[19] 2019 2013和2017 青海 26(10/16) 1 110.16(725.16/1 661.47)) <30岁: 760.46
<50岁: 781.76
≥50岁: 2 205.88曲颖等[14] 2022 2012—2014 上海 245(97/148) 1 323.25(1 164.33/1 453.26) - 总计 1425(392/824) 1 049.05(636.51/1 265.47) - 第一作者 PBC患者例数(男/女) PBC患病率(男/女,10万) 不同年龄段PBC患病率 Jiang等[12] 3(0/3) 59.87(0/96.53) - Liu等[13] 4(1/3) 49.22(23.54/77.36) >40岁: 女性155.8 郭亚平等[15] 58(-) 276.59(-) - Chen等[11] 25(2/23) 131.50(24.07/214.91) 50~59岁: 316.5 (0/473.9)
60~69岁: 85.8 (0/142.7)
70~79岁: 174.6 (67.3/228.7)
80~89岁: 360.0 (107.8/486.5)叶震璇等[18] 39(10/29) 106.97(53.51/163.18) ≤ 40岁: 24.04
41~60岁: 123.40
≥ 61岁: 415.05刘晓萍等[16] 10(4/6) 109.45(75.10/157.44) - 瞿国英等[17] 16(4/12) 98.37(48.91/148.39) 31~45岁: 48.50(32.19/64.98)
46~60岁: 154.80(50.56/263.43)
≥61岁: 894.00(530.50/1231.53)郑佳等[19] 1(0/1) 42.70(0/103.84) - 曲颖等[14] 12(2/10) 64.81(24.01/98.19) - 总计 168(23/87) 123.68(40.81/148.71) - -
[1] LINDOR KD, BOWLUS CL, BOYER J, et al. Primary biliary cholangitis: 2018 practice guidance from the american association for the study of liver diseases[J]. Hepatology, 2019, 69(1): 394-419. DOI: 10.1002/hep.30145. [2] YANG YF, DENG ZH. Immune mechanism of biliary epithelial cell injury in the small intrahepatic bile ducts in primary biliary cholangitis[J]. J Clin Hepatol, 2021, 37(6): 1466-1468. DOI: 10.3969/j.issn.1001-5256.2021.06.051.杨雅斐, 邓志华. 原发性胆汁性胆管炎肝内小胆管上皮细胞损伤的免疫学机制[J]. 临床肝胆病杂志, 2021, 37(6): 1466-1468. DOI: 10.3969/j.issn.1001-5256.2021.06.051. [3] European Association for the Study of the Liver. EASL Clinical Practice Guidelines: The diagnosis and management of patients with primary biliary cholangitis[J]. J Hepatol, 2017, 67(1): 145-172. DOI: 10.1016/j.jhep.2017.03.022. [4] ZHANG HP, YAN HP, CHEN DX, et al. The role of pathogen infections in the development and progression of autoimmune liver diseases[J]. Clin Hepatol, 2022, 38(4): 754-758. DOI: 10.3969/j.issn.1001-5256.2022.04.004.张海萍, 闫惠平, 陈德喜, 等. 病原感染在自身免疫性肝病发生发展中的作用[J]. 临床肝胆病杂志, 2022, 38(4): 754-758. DOI: 10.3969/j.issn.1001-5256.2022.04.004. [5] EFE C, TŞÇILAR K, HENRIKSSON I, et al. Validation of risk scoring systems in ursodeoxycholic acid-treated patients with primary biliary cholangitis[J]. Am J Gastroenterol, 2019, 114(7): 1101-1108. DOI: 10.14309/ajg.0000000000000290. [6] HARMS MH, van BUUREN HR, CORPECHOT C, et al. Ursodeoxycholic acid therapy and liver transplant-free survival in patients with primary biliary cholangitis[J]. J Hepatol, 2019, 71(2): 357-365. DOI: 10.1016/j.jhep.2019.04.001. [7] AHRENS EH Jr, PAYNE MA, KUNKEL HG, et al. Primary biliary cirrhosis[J]. Medicine (Baltimore), 1950, 29(4): 299-364. DOI: 10.1097/00005792-195012000-00002. [8] BOONSTRA K, BEUERS U, PONSIOEN CY. Epidemiology of primary sclerosing cholangitis and primary biliary cirrhosis: a systematic review[J]. J Hepatol, 2012, 56(5): 1181-1188. DOI: 10.1016/j.jhep.2011.10.025. [9] LV T, CHEN S, LI M, et al. Regional variation and temporal trend of primary biliary cholangitis epidemiology: A systematic review and meta-analysis[J]. J Gastroenterol Hepatol, 2021, 36(6): 1423-1434. DOI: 10.1111/jgh.15329. [10] ZENG N, DUAN W, CHEN S, et al. Epidemiology and clinical course of primary biliary cholangitis in the Asia-Pacific region: a systematic review and meta-analysis[J]. Hepatol Int, 2019, 13(6): 788-799. DOI: 10.1007/s12072-019-09984-x. [11] CHEN BH, WANG QQ, ZHANG W, et al. Screening of anti- mitochondrial antibody subtype M2 in residents at least 18 years of age in an urban district of Shanghai, China[J]. Eur Rev Med Pharmacol Sci, 2016, 20(10): 2052-2060. [12] JIANG XH, ZHONG RQ, FAN XY, et al. Characterization of M2 antibodies in asymptomatic Chinese population[J]. World J Gastroenterol, 2003, 9(9): 2128-2131. DOI: 10.3748/wjg.v9.i9.2128. [13] LIU H, LIU Y, WANG L, et al. Prevalence of primary biliary cirrhosis in adults referring hospital for annual health check-up in Southern China[J]. BMC Gastroenterol, 2010, 10: 100. DOI: 10.1186/1471-230X-10-100. [14] QU Y, CAI XB, ZHANG QD, et al. Prevalence of serum anti-mitochondrial antibody-M2 antibody in health check-up individuals[J]. J Prac Hepatol, 2022, 25(2): 203-206. DOI: 10.3969/j.issn.1672-5069.2022.02.013.曲颖, 蔡晓波, 张启迪, 等. 体检人群血清M2型抗线粒体抗体流行率调查[J]. 实用肝脏病杂志, 2022, 25(2): 203-206. DOI: 10.3969/j.issn.1672-5069.2022.02.013. [15] GUO YP, WANG CG, LIU X, et al. Evaluation of markers associated with primary biliary cirrhosis in a population of anti-mitochondrial antibody-M2 positive individuals[J]. Chin J Hepatol, 2014, 22(10): 735-738. DOI: 10.3760/cma.j.issn.1007-3418.2014.10.004.郭亚平, 王春光, 刘欣, 等. 抗线粒体抗体-M2阳性体检人群原发性胆汁性肝硬化相关指标的调查分析[J]. 中华肝脏病杂志, 2014, 22(10): 735-738. DOI: 10.3760/cma.j.issn.1007-3418.2014.10.004. [16] LIU XP, CUI LP, FANG LH. Investigation on primary biliary cirrhosis related indicators in anti-mitochondrial antibody-M2 positive physical examination group[J]. Systems Med, 2018, 3(11): 1-3, 17. DOI: 10.19368/j.cnki.2096-1782.2018.11.001.刘晓萍, 崔潞萍, 房丽华. 抗线粒体抗体-M2阳性体检人群患原发性胆汁性肝硬化相关指标调查分析[J]. 系统医学, 2018, 3(11): 1-3, 17. DOI: 10.19368/j.cnki.2096-1782.2018.11.001. [17] QU GY, QIAN H. Screening of healthy subjects' anti-mitochondrial antibody-M2 in a Shanghai community hospital in 2017[J]. Shanxi Med J, 2018, 47(21): 2536-2537. DOI: 10.3969/j.issn.0253-9926.2018.21.010.瞿国英, 钱慧. 2017年上海某社区医院健康体检者抗M2型线粒体抗体筛查分析[J]. 山西医药杂志, 2018, 47(21): 2536-2537. DOI: 10.3969/j.issn.0253-9926.2018.21.010. [18] YE ZX, YANG BW, ZHOU WJ, et al. Screening of specific anti- mitochondrial antibody-M2 in 36459 healthy subjects in Guiyang[J]. Laboratory Med, 2018, 33(3): 205-208. DOI: 10.3969/j.issn.1673-8640.2018.03.004.叶震璇, 杨必伟, 周雯婧, 等. 贵阳地区36459名健康体检者抗M2型线粒体抗体筛查分析[J]. 检验医学, 2018, 33(3): 205-208. DOI: 10.3969/j.issn.1673-8640.2018.03.004. [19] ZHENG J, LI ZA, A XR. Analysis and Significances of autoantibody in health check-up individuals[J]. Int J Lab Med, 2019, 40(19): 2412-2415. DOI: 10.3969/j.issn.1673-4130.2019.19.027.郑佳, 李子安, 阿祥仁. 体检人群自身抗体检测结果分析及意义[J]. 国际检验医学杂志, 2019, 40(19): 2412-2415. DOI: 10.3969/j.issn.1673-4130.2019.19.027. [20] HEATHCOTE EJ. Management of primary biliary cirrhosis. The American Association for the Study of Liver Diseases practice guidelines[J]. Hepatology, 2000, 31(4): 1005-1013. DOI: 10.1053/he.2000.5984. [21] LINDOR KD, GERSHWIN ME, POUPON R, et al. Primary biliary cirrhosis[J]. Hepatology, 2009, 50(1): 291-308. DOI: 10.1002/hep.22906. [22] European Association for the Study of the Liver. EASL clinical practice guidelines: management of cholestatic liver diseases[J]. J Hepatol, 2009, 51(2): 237-267. DOI: 10.1016/j.jhep.2009.04.009. [23] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Consensus on the diagnosis and management of primary biliary cirrhosis (cholangitis)(2015)[J]. J Clin Hepatol, 2015, 31(12): 1980-1988. DOI: 10.3969/j.issn.1001-5256.2015.12.004.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会感染病学分会. 原发性胆汁性肝硬化(又名原发性胆汁性胆管炎)诊断和治疗共识(2015)[J]. 临床肝胆病杂志, 2015, 31(12): 1980-1988. DOI: 10.3969/j.issn.1001-5256.2015.12.004. [24] CORDELL HJ, FRYETT JJ, UENO K, et al. An international genome-wide meta-analysis of primary biliary cholangitis: Novel risk loci and candidate drugs[J]. J Hepatol, 2021, 75(3): 572-581. DOI: 10.1016/j.jhep.2021.04.055. [25] LLEO A, COLAPIETRO F. Changes in the epidemiology of primary biliary cholangitis[J]. Clin Liver Dis, 2018, 22(3): 429-441. DOI: 10.1016/j.cld.2018.03.001. [26] LLEO A, WANG GQ, GERSHWIN ME, et al. Primary biliary cholangitis[J]. Lancet, 2020, 396(10266): 1915-1926. DOI: 10.1016/S0140-6736(20)31607-X. [27] COLAPIETRO F, LLEO A, GENERALI E. Antimitochondrial antibodies: from bench to bedside[J]. Clin Rev Allergy Immunol, 2022, 63(2): 166-177. DOI: 10.1007/s12016-021-08904-y. [28] SHUAI Z, WANG J, BADAMAGUNTA M, et al. The fingerprint of antimitochondrial antibodies and the etiology of primary biliary cholangitis[J]. Hepatology, 2017, 65(5): 1670-1682. DOI: 10.1002/hep.29059. [29] DUAN WJ, LYU TT, CHEN S, et al. Clinical features and prognosis of autoimmune hepatitis with antimitochondrial antibody positive[J]. J Clin Exp Med, 2022, 21(18): 1931-1934. DOI: 10.3969/j.issn.1671-4695.2022.18.008.段维佳, 吕婷婷, 陈莎, 等. 抗线粒体抗体阳性的自身免疫性肝炎患者的临床特点及预后[J]. 临床和实验医学杂志, 2022, 21(18): 1931-1934. DOI: 10.3969/j.issn.1671-4695.2022.18.008. -



 PDF下载 ( 2441 KB)
PDF下载 ( 2441 KB)


 下载:
下载: