超声内镜对胆总管泥沙样结石的诊断价值
DOI: 10.3969/j.issn.1001-5256.2023.02.018
Value of endoscopic ultrasonography in the diagnosis of muddy stones of the common bile duct
-
摘要:
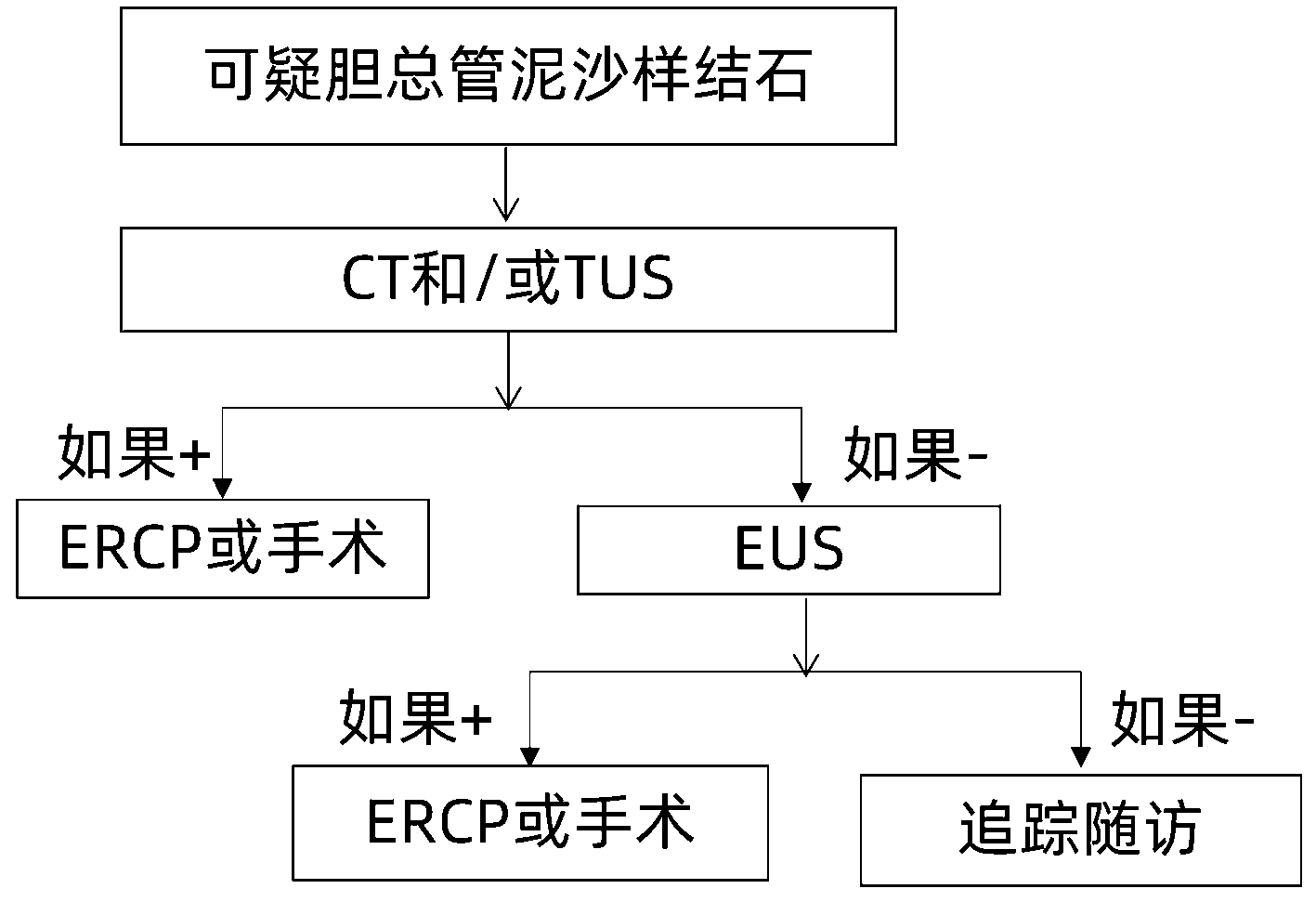
目的 通过比较超声内镜(EUS)及CT、腹部超声(TUS)对胆总管泥沙样结石的诊断能力,探讨EUS能否成为诊断性内镜逆行胰胆管造影(ERCP)的替代方法。 方法 选取2019年7月—2021年12月于广西壮族自治区南溪山医院就诊的53例疑似胆总管泥沙样结石的患者进行前瞻性研究,所有患者在行ERCP前均接受EUS、TUS和CT检查;以ERCP检查并行十二指肠乳头括约肌切开术(EST)取出胆总管泥沙样结石作为诊断胆总管泥沙样结石的金标准,将EUS、TUS和CT对胆总管泥沙样结石显示情况进行比较,计数资料组间比较采用χ2检验或Fisher精确概率法。 结果 53例患者中,EUS、TUS和CT检出胆总管泥沙样结石的阳性率分别为88.68%、50.94%和62.26%;在经ERCP下EST所证实的的阳性结果中,其中EUS检出胆总管泥沙样结石的敏感度、特异度和准确度分别为93.75%、60.00%和90.57%;TUS分别为56.25%、100.00%和60.38%;而CT为66.67%、80.00%和67.92%。EUS检出胆总管泥沙样结石的准确性与CT比较,差异有统计学意义(χ2=8.26,P=0.004),EUS与TUS的诊断准确性比较,差异有统计学意义(χ2=13.05,P<0.001)。 结论 在胆总管泥沙样结石的诊断上,EUS比TUS和CT的检出更准确,对于TUS、CT未能发现病变而临床怀疑为胆总管泥沙样结石时,推荐进行EUS检查,以便明确诊断,而不是首选ERCP检查,为此可以减少相关成本和由此带来的并发症。 -
关键词:
- 胆总管结石病 /
- 腔内超声检查 /
- 胰胆管造影术, 内窥镜逆行 /
- 诊断
Abstract:Objective To investigate whether endoscopic ultrasonography (EUS) can be an alternative method for diagnostic endoscopic retrograde cholangiopancreatography (ERCP) by comparing the ability of EUS versus CT and transabdominal ultrasonography (TUS) in the diagnosis of muddy stones of the common bile duct. Methods A prospective study was conducted for 53 patients suspected of muddy stones of the common bile duct who attended Nanxishan Hospital of Guangxi Zhuang Autonomous Region from July 2019 to December 2021, and all patients underwent EUS, TUS, and CT before ERCP. With ERCP and endoscopic sphincterotomy (EST) for removing muddy stones of the common bile duct as the gold standard for the diagnosis of muddy stones of the common bile duct, EUS, TUS, and CT were compared in terms of their ability to display the muddy stones of the common bile duct. The chi-square test or the Fisher's exact test was used for comparison of categorical data between groups. Results In the 53 patients, EUS, TUS, and CT had a positive rate of 88.68%, 50.94%, and 62.26%, respectively, in detecting muddy stones of the common bile duct. As for the positive results confirmed by EST under ERCP, EUS had a sensitivity of 93.75%, a specificity of 60.00%, and an accuracy of 90.57% in detecting muddy stones of the common bile duct, while TUS had a sensitivity of 56.25%, a specificity of 100.00%, and an accuracy of 60.38% and CT had a sensitivity of 66.67%, a specificity of 80.00%, and an accuracy of 67.92%. There was a significant difference between EUS and CT in the accuracy in detecting muddy stones of the common bile duct (χ2=8.26, P=0.004), and there was also a significant difference in diagnostic accuracy between EUS and TUS (χ2=13.05, P < 0.001). Conclusion EUS is more accurate than TUS and CT in the diagnosis of muddy stones of the common bile duct, and instead of ERCP, EUS is thus recommended for suspected muddy stones of the common bile duct when TUS and CT fail to identify the lesions in clinical practice, so as to make a confirmed diagnosis and reduce related costs and complications. -
表 1 纳入患者的一般特征
Table 1. The general characteristics of patients
项目 数值 男性[例(%)] 24(45) 年龄(岁) 57.64±14.03 ALT(U/L) 93.00(56.50~240.00) AST(U/L) 74.00(45.00~178.00) GGT(U/L) 277.00(80.50~507.00) ALP(U/L) 174.00(93.50~228.00) TBil(μmol/L) 40.70(13.90~64.00) 表 2 EUS、CT和TUS各检查结果对比
Table 2. Comparison of EUS, CT and TUS examination results
检查方法 ERCP(+)(n=48) ERCP(-)(n=5) 合计(n=53) EUS(+) 45 2 47 EUS(-) 3 3 6 CT(+) 32 1 33 CT(-) 16 4 20 TUS(+) 27 0 27 TUS(-) 21 5 26 表 3 EUS、CT和TUS对胆总管泥沙样结石的诊断准确性比较
Table 3. Comparison of diagnostic accuracy of EUS, CT and TUS in choledocholithiasis
项目 EUS CT TUS 敏感度 93.75%(45/48) 66.67%(32/48)1) 56.25%(27/48)1) 特异度 60.00%(3/5) 80.00%(4/5)1) 100.00%(5/5)1) 准确度 90.57%(48/53) 67.92%(36/53)1) 60.38%(32/53)1) 注:与EUS比较,1)P<0.025。 -
[1] CAI JS, QIANG S, BAO-BING Y. Advances of recurrent risk factors and management of choledocholithiasis[J]. Scand J Gastroenterol, 2017, 52(1): 34-43. DOI: 10.1080/00365521.2016.1224382. [2] WILKINS T, AGABIN E, VARGHESE J, et al. Gallbladder dysfunction: cholecystitis, choledocholithiasis, cholangitis, and biliary dyskinesia[J]. Prim Care, 2017, 44(4): 575-597. DOI: 10.1016/j.pop.2017.07.002. [3] MA RH, LUO XB, WANG XF, et al. A comparative study of mud-like and coralliform calcium carbonate gallbladder stones[J]. Microsc Res Tech, 2017, 80(7): 722-730. DOI: 10.1002/jemt.22857. [4] PEREIRA R, ESLICK G, COX M. Endoscopic ultrasound for routine assessment in idiopathic acute pancreatitis[J]. J Gastrointest Surg, 2019, 23(8): 1694-1700. DOI: 10.1007/s11605-019-04272-3. [5] HILL PA, HARRIS RD. Clinical importance and natural history of biliary sludge in outpatients[J]. J Ultrasound Med, 2016, 35(3): 605-610. DOI: 10.7863/ultra.15.05026. [6] KEIZMAN D, ISH-SHALOM M, KONIKOFF FM. The clinical significance of bile duct sludge: is it different from bile duct stones?[J]. Surg Endosc, 2007, 21(5): 769-773. DOI: 10.1007/s00464-006-9153-0. [7] PLEWKA M, RYSZ J, KUJAWSKI K. Complications of endoscopic retrograde cholangiopancreatography[J]. Pol Merkur Lekarski, 2017, 43(258): 272-275. [8] ŞURLIN V, SǍFTOIU A, DUMITRESCU D. Imaging tests for accurate diagnosis of acute biliary pancreatitis[J]. World J Gastroenterol, 2014, 20(44): 16544-16549. DOI: 10.3748/wjg.v20.i44.16544. [9] COSTI R, SARLI L, CARUSO G, et al. Preoperative ultrasonographic assessment of the number and size of gallbladder stones: is it a useful predictor of asymptomatic choledochal lithiasis?[J]. J Ultrasound Med, 2002, 21(9): 971-976. DOI: 10.7863/jum.2002.21.9.971. [10] CANLAS KR, BRANCH MS. Role of endoscopic retrograde cholangiopancreatography in acute pancreatitis[J]. World J Gastroenterol, 2007, 13(47): 6314-6320. DOI: 10.3748/wjg.v13.i47.6314. [11] LOU LZ, LIU HL, REN JC. Clinical value of magnetic reso- nance cholangiopancrea tography and CT in the diagnosis of 70 patients with biliary calculi[J]. Guide China Med, 2017, 15(16): 97-98. DOI: 10.15912/j.cnki.gocm.2017.16.074.娄立志, 刘红玲, 任锦程. 70例胆系结石患者行磁共振胰胆管成像和CT诊断的临床价值分析[J]. 中国医药指南, 2017, 15(16): 97-98. DOI: 10.15912/j.cnki.gocm.2017.16.074. [12] PATEL R, INGLE M, CHOKSI D, et al. Endoscopic ultrasonography can prevent unnecessary diagnostic endoscopic retrograde cholangiopancreatography even in patients with high likelihood of choledocholithiasis and inconclusive ultrasonography: results of a prospective study[J]. Clin Endosc, 2017, 50(6): 592-597. DOI: 10.5946/ce.2017.010. [13] PRAT F, AMOUYAL G, AMOUYAL P, et al. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common-bileduct lithiasis[J]. Lancet, 1996, 347(8994): 75-79. DOI: 10.1016/s0140-6736(96)90208-1. [14] KOHUT M, NOWAK A, NOWAKOWSKA-DULAWA E, et al. Endosonography with linear array instead of endoscopic retrograde cholangiography as the diagnostic tool in patients with moderate suspicion of common bile duct stones[J]. World J Gastroenterol, 2003, 9(3): 612-614. DOI: 10.3748/wjg.v9.i3.612. [15] MESIHOVI C ' R, MEHMEDOVI C ' A. Better non-invasive endoscopic procedure: endoscopic ultrasound or magnetic resonance cholangiopancreatography?[J]. Med Glas (Zenica), 2019, 16(1): 40-44. DOI: 10.17392/955-19. [16] JVNGST C, KULLAK-UBLICK GA, JVNGST D. Gallstone disease: Microlithiasis and sludge[J]. Best Pract Res Clin Gastroenterol, 2006, 20(6): 1053-1062. DOI: 10.1016/j.bpg.2006.03.007. [17] ZHANG H, HUANG P, ZHANG XF, et al. Comparison of endoscopic ultrasonography, transabdominal ultrasonography and magnetic resonance cholangiopancreatography in diagnosis of common bile duct stones[J]. China J Endosc, 2015, 21(1): 26-29. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGNJ201501006.htm张皞, 黄平, 张筱凤, 等. 超声内镜、腹部超声及磁共振胰胆管造影对胆总管结石诊断价值的对比分析研究[J]. 中国内镜杂志, 2015, 21(1): 26-29. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGNJ201501006.htm [18] JEON TJ, CHO JH, KIM YS, et al. Diagnostic value of endoscopic ultrasonography in symptomatic patients with high and intermediate probabilities of common bile duct stones and a negative computed tomography scan[J]. Gut Liver, 2017, 11(2): 290-297. DOI: 10.5009/gnl16052. [19] DITTRICK G, LAMONT JP, KUHN JA, et al. Usefulness of endoscopic ultrasound in patients at high risk of choledocholithiasis[J]. Proc (Bayl Univ Med Cent), 2005, 18(3): 211-213. DOI: 10.1080/08998280.2005.11928068. [20] HONG J, CAI Q, CUI W. Application value of 3.0 T MRCP combined with abdominal color Doppler ultrasound in the diagnosis of suspected gallstones[J]. Chin Med Herald, 2021, 18(19): 159-162. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202119040.htm洪杰, 蔡琦, 崔巍. 3.0T MRCP联合腹部彩超在可疑胆囊结石诊断中的应用价值[J]. 中国医药导报, 2021, 18(19): 159-162. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202119040.htm [21] VILA JJ, VICUÑA M, IRISARRI R, et al. Diagnostic yield and reliability of endoscopic ultrasonography in patients with idiopathic acute pancreatitis[J]. Scand J Gastroenterol, 2010, 45(3): 375-381. DOI: 10.3109/00365520903508894. [22] CHEN CC. The efficacy of endoscopic ultrasound for the diagnosis of common bile duct stones as compared to CT, MRCP, and ERCP[J]. J Chin Med Assoc, 2012, 75(7): 301-302. DOI: 10.1016/j.jcma.2012.05.002. 期刊类型引用(3)
1. 粟雨萌,张鸣杰,谈振华,谢平. 胰十二指肠切除术后发生胃排空延迟的危险因素分析. 肝胆胰外科杂志. 2024(10): 608-611+616 .  百度学术
百度学术2. 张苗苗,白纪刚,张东,雷建军,耿智敏,冯爱芳,董芳芳,史爱华,吕毅,严小鹏. 用于胰十二指肠切除术中Braun吻合磁环的设计及临床应用. 中国医疗设备. 2022(06): 8-11 .  百度学术
百度学术3. 李利平,游意莹,沈宁,曹宏,王艳玲. 改良内陷式胰肠吻合在胰十二指肠切除术中的应用. 中华肝脏外科手术学电子杂志. 2022(05): 458-462 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 2729 KB)
PDF下载 ( 2729 KB)


 下载:
下载:

 百度学术
百度学术

