淤胆通方对α-萘异硫氰酸酯诱导的胆汁淤积小鼠肠道菌群和肠道屏障功能的影响
DOI: 10.3969/j.issn.1001-5256.2023.04.018
Effect of Yudantong decoction on intestinal flora and intestinal barrier function in mice with cholestasis induced by α-naphthyl isothiocyanate
-
摘要:
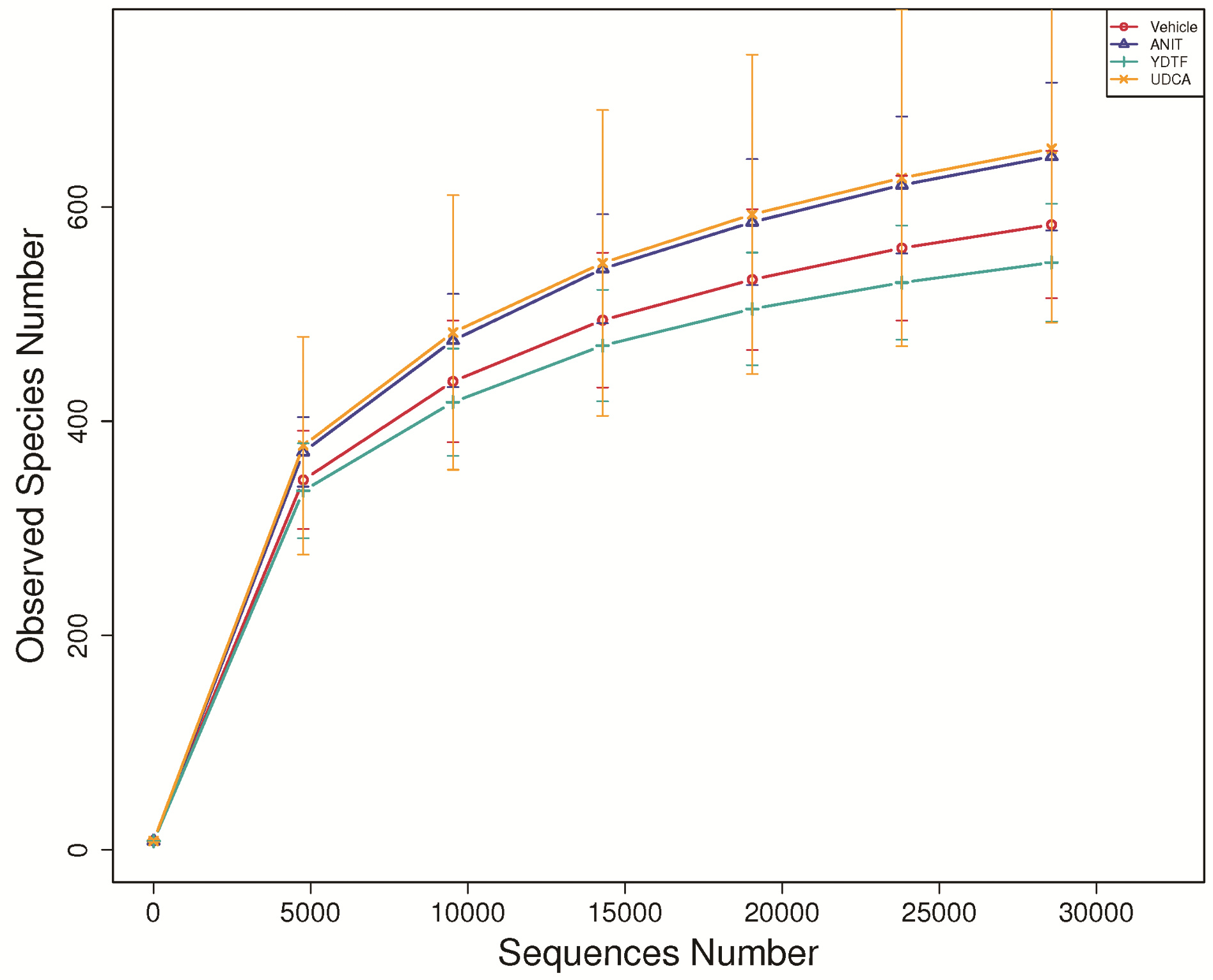
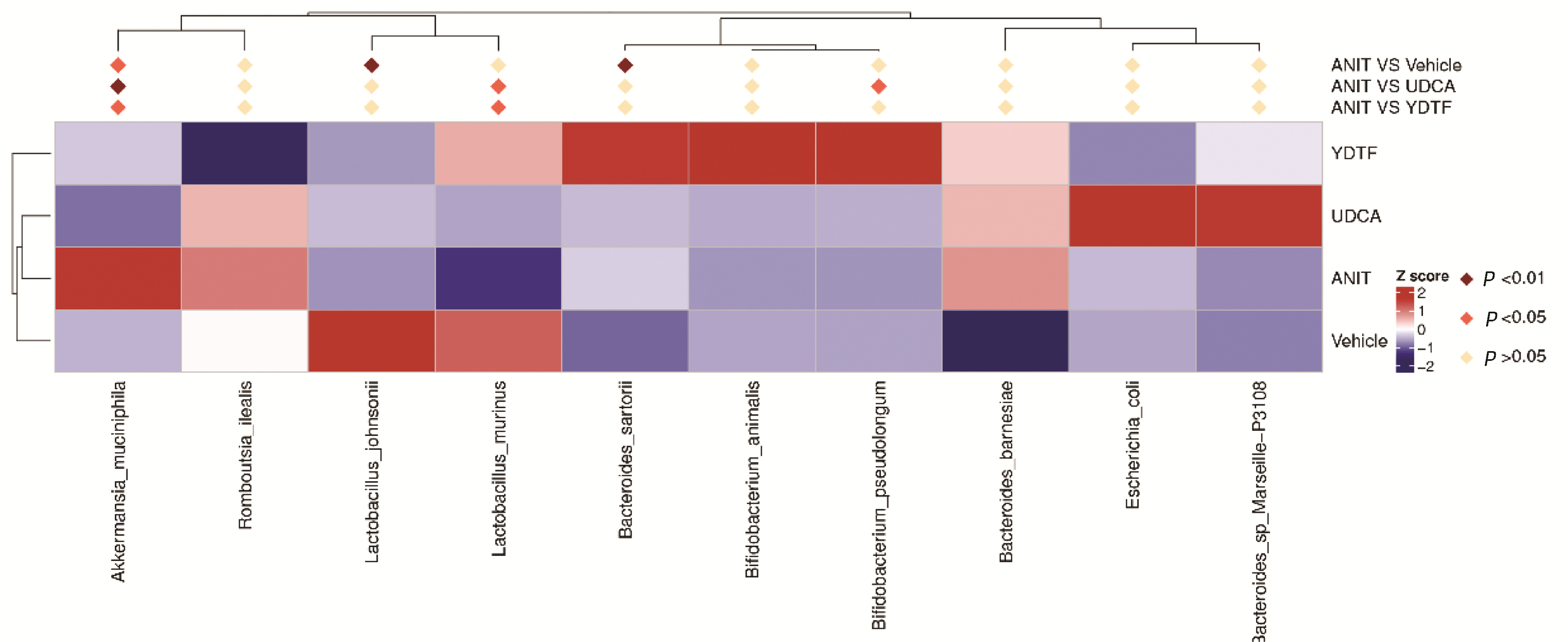
目的 观察淤胆通方对α-萘异硫氰酸酯(ANIT)诱导的胆汁淤积小鼠的治疗作用,并基于肠道菌群和肠道屏障功能探讨其作用靶点和机制。 方法 将24只C57BL/6小鼠随机分为对照组、模型组、淤胆通方组、熊去氧胆酸(UDCA)组,每组6只。模型组、淤胆通方组、UDCA组小鼠分别于第1天、第4天、第7天、第10天、第13天予ANIT 35 mg·kg-1·d-1灌胃,淤胆通方组、UDCA组小鼠每天分别予淤胆通方、UDCA灌胃,连续15 d,第16天取材。观察肝脏组织病理学,检测肝功能指标;免疫组化法检测肝caspase-1、IL-1β、FXR的蛋白表达,流式细胞术检测肝脏CD11b+、CD86+、CD45+免疫细胞的比例;对粪便微生物进行16S rDNA测序及信息分析;免疫组化法检测肠FXR/NLRP3通路的蛋白表达,免疫荧光法检测肠E-cadherin、Occludin的蛋白表达。当计量资料满足方差齐性,多组间比较采用单因素方差分析,进一步两两比较采用LSD-t检验;当资料不满足方差齐性,采用Welch检验,进一步两两比较采用Games-Howell检验。 结果 HE染色显示,模型组小鼠的部分肝细胞脂肪变性,肝小叶内肝细胞大面积坏死,肝小叶结构破坏,伴有大量炎性细胞浸润,淤胆通方组和UDCA组小鼠的肝细胞脂肪变性减轻,肝小叶内肝细胞坏死不明显,炎性细胞减少;模型组小鼠的血清ALT、AST、GGT、ALP、TBil、DBil、TBA水平较对照组明显升高(P值均<0.05);与模型组相比,淤胆通方组的血清ALT、AST、GGT、ALP、TBil、DBil、TBA水平显著降低(P值均<0.05),UDCA组的血清GGT、TBil、DBil、TBA水平显著下降(P值均<0.05)。与对照组比较,模型组肝脏caspase-1、IL-1β水平明显升高、肝FXR的表达明显下降(P值均<0.05),与模型组比较,淤胆通方组肝脏caspase-1、IL-1β水平及UDCA组肝脏IL-1β水平显著下降,淤胆通方组和UDCA组的肝FXR表达水平显著升高(P值均<0.05)。模型组的肠道菌群组成较对照组发生显著变化(P<0.05);淤胆通方组的肠道菌群结构与模型组存在统计学差异(P<0.05);UDCA组肠道菌群构成与对照组、模型组均有统计学差异(P值均<0.05);相对于对照组,模型组的肠道嗜黏蛋白阿克曼菌丰度明显升高,约氏乳杆菌丰度明显下降(P值均<0.05);与模型组比较,淤胆通方组、UDCA组嗜黏蛋白阿克曼菌的丰度均显著下降,淤胆通方组的鼠乳杆菌、UDCA组的鼠乳杆菌和假长双歧杆菌的丰度均明显升高(P值均<0.05)。与对照组比较,模型组的肠FXR蛋白表达明显降低,肠NLRP3蛋白表达明显升高,肠E-cadherin和Occludin表达均明显下降(P值均<0.05);与模型组相比,淤胆通方组和UDCA组的肠FXR表达显著上调,肠NLRP3表达显著下降,肠E-cadherin和Occludin的蛋白表达均显著升高(P值均<0.05)。 结论 淤胆通方可减轻ANIT诱导的胆汁淤积小鼠的肝损伤,改善肠道菌群和增强肠壁屏障功能可能是其作用靶点和机制之一。 Abstract:Objective To investigate the therapeutic effect of Yudantong decoction in mice with α-naphthyl isothiocyanate (ANIT)-induced cholestasis, as well as its targets and mechanism based on intestinal flora and intestinal barrier function. Methods A total of 24 C57BL/6 mice were randomly divided into control group, model group, Yudantong decoction group (YDTF group), and ursodeoxycholic acid (UDCA) group, with 6 mice in each group. The mice in the model group, the YDTF group, and the UDCA group were given ANIT 35 mg/kg/day by gavage on days 1, 4, 7, 10, and 13, and those in the YDTF group and the UDCA group were given Yudantong decoction or UDCA by gavage for 15 consecutive days; related samples were collected on day 16. Liver histopathology was observed, and liver function parameters were measured; immunohistochemistry was used to measure the protein expression levels of caspase-1, interleukin-1β (IL-1β), and FXR in the liver, and flow cytometry was used to measure the percentages of CD11b+, CD86+, and CD45+ immune cells in the liver; 16S rDNA sequencing and information analysis were performed for fecal microorganisms; immunohistochemistry was used to measure the protein expression of the intestinal FXR/NLRP3 pathway, and immunofluorescence assay was used to measure the protein expression of intestinal E-cadherin and occludin. A one-way analysis of variance was used for comparison of continuous data with homogeneity of variance between multiple groups, and the least significant difference t-test was used for further comparison between two groups; the Welch test was used for comparison of data with heterogeneity of variance between multiple groups, and the Games-Howell test was used for further comparison between two groups. Results HE staining showed that the model group had partial hepatocyte fatty degeneration, massive necrosis of hepatocytes in hepatic lobules, damage of lobular structure, and massive inflammatory cell infiltration, and the YDTF group and the UDCA group had alleviation of hepatocyte fatty degeneration and hepatocyte necrosis in hepatic lobules, with a reduction in inflammatory cells. Compared with the control group, the model group had significantly higher serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transpeptidase (GGT), alkaline phosphatase (ALP), total bilirubin (TBil), direct bilirubin (DBil), and total bile acid (TBA) (all P < 0.05); compared with the model group, the YDTF group had significant reductions in the serum levels of ALT, AST, GGT, ALP, TBil, DBil, and TBA (all P < 0.05), and the UDCA group had significant reductions in the serum levels of GGT, TBil, DBil, and TBA (all P < 0.05). Compared with the control group, the model group had significant increases in the levels of caspase-1 and IL-1β and a significant reduction in the expression of FXR in the liver (all P < 0.05); compared with the model group, the YDTF group had significant reductions in the levels of caspase-1 and IL-1β in the liver and the UDCA group had a significant reduction in the level of IL-1β in the liver, and both the YDTF group and the UDCA group had a significant increase in the expression level of FXR in the liver (all P < 0.05). The model group had a significant change in the composition of intestinal flora compared with the control group (P < 0.05); there was a significant difference in the structure of intestinal flora between the YDTF group and the model group (P < 0.05), and there was also a significant difference in the composition of intestinal flora between the UDCA group and the control/model groups (P < 0.05). Compared with the control group, the model group had a significant increase in the abundance of intestinal Akkermansia muciniphila and a significant reduction in the abundance of Lactobacillus johnsonii (both P < 0.05); compared with the model group, both the YDTF group and the UDCA group had a significant reduction in the abundance of intestinal Akkermansia muciniphila, and the YDTF group had a significant increase in the abundance of Lactobacillus murinus, while the UDCA group had significant increases in the abundance of Lactobacillus murinus and Bifidobacterium pseudolongum (all P < 0.05). Compared with the control group, the model group had a significant reduction in the protein expression of intestinal FXR, a significant increase in the protein expression of intestinal NLRP3, and significant reductions in the expression of intestinal E-cadherin and occludin (all P < 0.05); compared with the model group, both the YDTF group and the UDCA group had a significant increase in the protein expression of intestinal FXR, a significant reduction in the protein expression of intestinal NLRP3, and significant increases in the expression of intestinal E-cadherin and occludin (all P < 0.05). Conclusion Yudantong decoction can alleviate liver injury in mice with ANIT-induced cholestasis, possibly by improving intestinal flora and enhancing intestinal barrier function. -
Key words:
- Cholestasis /
- Gastrointestinal Microbiome /
- Yudantong Decoction /
- Mice
-
表 1 各组小鼠肝功能指标的比较
Table 1. Comparison of liver function indexes of mice in each group
指标 对照组(n=6) 模型组(n=6) 淤胆通方组(n=6) UDCA组(n=6) F值 P值 ALT(U/L) 49.02±7.62 115.37±11.001) 84.68±19.082) 107.68±26.14 47.613) <0.001 AST(U/L) 89.35±11.31 263.88±50.821) 202.83±61.992) 208.85±54.07 13.28 <0.001 GGT(U/L) 18.14±4.49 33.78±9.971) 25.08±4.772) 23.47±7.602) 5.05 0.009 ALP(U/L) 28.55±4.51 96.68±12.871) 80.52±13.682) 84.23±18.28 30.75 <0.001 TBil(μmol/L) 4.12±1.09 8.93±0.941) 6.07±1.062) 5.86±0.762) 25.05 <0.001 DBil(μmol/L) 2.56±0.26 4.37±1.391) 3.20±0.422) 2.87±0.502) 6.15 0.004 TBA(μmol/L) 54.80±7.17 93.52±9.171) 78.35±15.702) 63.03±7.302) 16.16 <0.001 注:与对照组比较,1)P<0.01;与模型组比较,2)P<0.01;3)Welch检验统计值。 表 2 各组小鼠肝脏组织中caspase-1、IL-1β及FXR的免疫组化累积光密度值(IOD)分析
Table 2. Immunohistochemical cumulative optical density (IOD) analysis of caspase-1, IL-1β, FXR in liver tissues of mice in each group
组别 动物数(只) caspase-1 IL-1β FXR 对照组 3 61.02±37.23 18.55±27.09 52 041.52±17 110.94 模型组 3 3 912.78±1 859.561) 5 412.49±2 405.652) 699.68±1 025.592) 淤胆通方组 3 1 885.43±630.713) 2 527.48±605.683) 17 158.18±6 910.154) UDCA组 3 3 203.67±894.45 2 602.44±649.893) 19 618.77±15 895.493) F值5) 67.86 103.26 42.98 P值 <0.001 <0.001 <0.001 注:与对照组比较,1)P<0.01,2)P<0.001;与模型组比较,3)P<0.05,4)P<0.001;5)Welch检验统计值。 表 3 各组小鼠肝脏组织中CD11b+、CD86+、CD45+免疫细胞的比例分析
Table 3. Analysis of the proportion of CD11b+, CD86+, CD45+ immune cells in liver tissues of mice in each group
组别 动物数(只) CD11b+细胞百分比(%) CD86+细胞百分比(%) CD45+细胞百分比(%) 对照组 3 7.47±1.05 7.76±0.51 6.96±0.52 模型组 3 76.33±1.361) 97.97±0.151) 99.17±0.211) 淤胆通方组 3 25.60±2.012) 27.70±0.702) 26.47±0.602) UDCA组 3 22.40±1.802) 19.07±0.872) 20.97±0.832) F值 1 055.68 12 942.67 14 931.48 P值 <0.001 <0.001 <0.001 注:与对照组比较,1)P<0.001;与模型组比较,2)P<0.001。 表 4 ANOSIM分析
Table 4. Analysis of similarities
组别 R值 P值 对照组-模型组 0.583 3 0.004 模型组-淤胆通方组 0.275 9 0.013 模型组-UDCA组 0.372 2 0.011 对照组-淤胆通方组 0.235 2 0.069 对照组-UDCA组 0.283 3 0.013 注:R>0,组间差异大于组内差异;R<0,组内差异大于组间差异。 表 5 各组小鼠的肠E-cadherin、Occludin、FXR、NLRP3的免疫荧光累积IOD分析
Table 5. Immunofluorescence cumulative optical density (IOD) analysis of intestinal E-cadherin and Occludin of mice in each group
组别 动物数(只) E-cadherin Occludin FXR NLRP3 对照组 3 34 686.33±6 277.77 30 046.64±24 583.08 1 161.31±572.99 540.83±121.52 模型组 3 6 394.06±1 088.971) 4 117.80±3 506.981) 236.88±123.13 1 824.55±450.561) 淤胆通方组 3 12 274.98±2 302.672) 9 231.42±4 026.382) 12 322.69±13 072.543) 84.63±57.313) UDCA组 3 23 102.74±7 824.212) 21 320.54±16 946.752) 7 767.62±2 878.382) 129.36±106.663) F值 75.224) 7.144) 6.56 69.634) P值 <0.001 0.003 0.001 <0.001 注:与对照组比较,1)P<0.001;与模型组比较,2)P<0.05,3)P<0.001;4)Welch检验统计值。 -
[1] YU RH, WANG YZ, ZHANG T. Clinical characteristics of infantile liver disease[J]. J Clin Pediatr, 2021, 39(1): 1-5. DOI: 10.3969/j.issn.1000-3606.2021.01.001.余荣华, 王怡仲, 张婷. 婴儿期肝病临床特点分析[J]. 临床儿科杂志, 2021, 39(1): 1-5. DOI: 10.3969/j.issn.1000-3606.2021.01.001. [2] JIN M. Progress of cholestatic liver disease and intestinal flora in children[J]. Int J Pediatr, 2020, 47(8): 548-551. DOI: 10.3760/cma.j.issn.1673-4408.2020.08.008.金萌. 胆汁淤积性肝病与儿童肠道菌群研究进展[J]. 国际儿科学杂志, 2020, 47(8): 548-551. DOI: 10.3760/cma.j.issn.1673-4408.2020.08.008. [3] FANG KL, ZHENG XT, XU LP, et al. Experimental research progress of traditional chinese medicine in prevention and treatment of cholestatic liver disease[J]. Chin J Integr Tradit West Med Liver Dis, 2020, 30(4): 375-377. DOI: 10.3969/j.issn.1005-0264.2020.04.027.方凯璐, 郑秀婷, 徐丽萍, 等. 传统中药防治胆汁淤积性肝病的实验研究进展[J]. 中西医结合肝病杂志, 2020, 30(4): 375-377. DOI: 10.3969/j.issn.1005-0264.2020.04.027. [4] LARUSSO NF, TABIBIAN JH, O'HARA SP. Role of the intestinal microbiome in cholestatic liver disease[J]. Dig Dis, 2017, 35(3): 166-168. DOI: 10.1159/000450906. [5] ZHOU R, FAN X, SCHNABL B. Role of the intestinal microbiome in liver fibrosis development and new treatment strategies[J]. Transl Res, 2019, 209: 22-38. DOI: 10.1016/j.trsl.2019.02.005. [6] GUO C. Clinical and basic study on intestinal microecology of cholestasis[D]. Shijiazhuang: Hebei Medical University, 2020.郭城. 胆汁淤积症肠道微生态学的临床与基础研究[D]. 石家庄: 河北医科大学, 2020. [7] HU Y, YAO Y, LIU J, et al. Pei Xueyi's experience in treating infantile hepatitis syndrome[J]. Chin J Inf Tradit Chin Med, 2012, 19(2): 87. DOI: 10.3969/j.issn.1005-5304.2012.02.041.胡艳, 幺远, 柳静, 等. 裴学义治疗婴儿肝炎综合征经验[J]. 中国中医药信息杂志, 2012, 19(2): 87. DOI: 10.3969/j.issn.1005-5304.2012.02.041. [8] CHEN L, HU Y, YANG M, et al. Interventional effect of traditional Chinese medicine on infants with biliary atresia after operation and its long-term effect[J]. JETCM, 2016, 25(2): 353-356. DOI: 10.3969/j.issn.1004-745X.2016.02.060.陈黎, 胡艳, 杨梦, 等. 中药对婴儿胆道闭锁术后的干预作用及其远期疗效的观察[J]. 中国中医急症, 2016, 25(2): 353-356. DOI: 10.3969/j.issn.1004-745X.2016.02.060. [9] HU Y, CHEN L, SHU J, et al. Clinical observation on 60 cases of infant cytomegalovirus hepatitis treated with traditional Chinese medicine[J]. Chin Pediatr Integr Tradit Wset Med, 2012, 4(1): 98-99. DOI: 10.3969/j.issn.1674-3865.2012.02.002.胡艳, 陈黎, 舒静, 等. 中药治疗婴儿巨细胞病毒性肝炎60例疗效观察[J]. 中国中西医结合儿科学, 2012, 4(1): 98-99. DOI: 10.3969/j.issn.1674-3865.2012.02.002. [10] DU LN, YANG Y. Establishment and application of animal models of cholestasis[J]. J Clin Hepatol, 2019, 35(2): 444-447. DOI: 10.3969/j.issn.1001-5256.2019.02.046.杜丽娜, 杨燕. 胆汁淤积动物模型的构建及应用前景[J]. 临床肝胆病杂志, 2019, 35(2): 444-447. DOI: 10.3969/j.issn.1001-5256.2019.02.046. [11] LUO YS, ZHENG XT, ZHANG HY, et al. The cholestatic fibrosis induced by α-naphthylisothiocyanate in mice and the inflammation pathway[J]. CJAP, 2020, 36(2): 152-157. DOI: 10.12047/j.cjap.5903.2020.034.罗怡爽, 郑秀婷, 章浩月, 等. α-荼异硫氰酸酯诱导小鼠胆汁淤积性肝纤维化及其炎症通路[J]. 中国应用生理学杂志, 2020, 36(2): 152-157. DOI: 10.12047/j.cjap.5903.2020.034. [12] ZHANG CY, LIU TH, WANG W, et al. Discussion on intestinal microenvironment as an important biological basis for the theory of treating liver disease from the spleen[J]. CJTCMP, 2019, 34(7): 2877-2880. https://www.cnki.com.cn/Article/CJFDTOTAL-BXYY201907011.htm张晨阳, 刘天浩, 王维, 等. 论肠道微环境是从脾论治肝病的重要生物学基础[J]. 中华中医药杂志, 2019, 34(7): 2877-2880. https://www.cnki.com.cn/Article/CJFDTOTAL-BXYY201907011.htm [13] LIAO L, SCHNEIDER KM, GALVEZ E, et al. Intestinal dysbiosis augments liver disease progression via NLRP3 in a murine model of primary sclerosing cholangitis[J]. Gut, 2019, 68(8): 1477-1492. DOI: 10.1136/gutjnl-2018-316670. [14] SWANSON KV, DENG M, TING JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics[J]. Nat Rev Immunol, 2019, 19(8): 477-489. DOI: 10.1038/s41577-019-0165-0. [15] JIA SQ, DOU XG. Farnesol X receptor and its agonists and liver diseases[J]. Chin Hepatol, 2021, 26(11): 1293-1297. DOI: 10.3969/j.issn.1008-1704.2021.11.027.贾锶琦, 窦晓光. 法尼醇X受体及其激动剂与肝脏疾病[J]. 肝脏, 2021, 26(11): 1293-1297. DOI: 10.3969/j.issn.1008-1704.2021.11.027. [16] ISAACS-TEN A, ECHEANDIA M, MORENO-GONZALEZ M, et al. Intestinal microbiome-macrophage crosstalk contributes to cholestatic liver disease by promoting intestinal permeability[J]. Hepatology, 2020, 72(6): 2090-2108. DOI: 10.1002/hep.31228. [17] HAO H, CAO L, JIANG C, et al. Farnesoid X receptor regulation of the NLRP3 inflammasome underlies cholestasis-associated sepsis[J]. Cell Metab, 2017, 25(4): 856-867. e5. DOI: 10.1016/j.cmet.2017.03.007. [18] HUANG F, ZHENG X, MA X, et al. Theabrownin from Pu-erh tea attenuates hypercholesterolemia via modulation of gut microbiota and bile acid metabolism[J]. Nat Commun, 2019, 10(1): 4971. DOI: 10.1038/s41467-019-12896-x. [19] WAHLSTRÖM A, KOVATCHEVA-DATCHARY P, STÅHLMAN M, et al. Crosstalk between bile acids and gut microbiota and its impact on farnesoid X receptor signalling[J]. Dig Dis, 2017, 35(3): 246-250. DOI: 10.1159/000450982. [20] LI SL. Effect of FXR on LPS-induced macrophage inflammatory response and intestinal barrier injury in mice[D]. Chinese People's Liberation Army (PLA) Medical School, 2019.李淑玲. FXR对LPS诱导的巨噬细胞炎症反应及小鼠肠道屏障损伤的作用研究[D]. 中国人民解放军医学院, 2019. [21] VERBEKE L, FARRE R, VERBINNEN B, et al. The FXR agonist obeticholic acid prevents gut barrier dysfunction and bacterial translocation in cholestatic rats[J]. Am J Pathol, 2015, 185(2): 409-419. DOI: 10.1016/j.ajpath.2014.10.009. [22] ZHOU JL, WANG ZX, ZHOU SM, et al. Composition and functional change of intestinal microbiota in infantile cholestasis[J]. J Clin Hepatol, 2021, 37(1): 126-130. DOI: 10.3969/j.issn.1001-5256.2021.01.025.周建利, 王朝霞, 周少明, 等. 婴儿胆汁淤积的肠道菌群组成及功能变化[J]. 临床肝胆病杂志, 2021, 37(1): 126-130. DOI: 10.3969/j.issn.1001-5256.2021.01.025. [23] PAN F, ZHANG L, LI M, et al. Predominant gut Lactobacillus murinus strain mediates anti-inflammaging effects in calorie-restricted mice[J]. Microbiome, 2018, 6(1): 54. DOI: 10.1186/s40168-018-0440-5. [24] WANG H, HE S, XIN J, et al. Psychoactive effects of lactobacillus johnsonii against restraint stress-induced memory dysfunction in mice through modulating intestinal inflammation and permeability-a study based on the gut-brain axis hypothesis[J]. Front Pharmacol, 2021, 12: 662148. DOI: 10.3389/fphar.2021.662148. [25] ZHANG H, LIU M, LIU X, et al. Bifidobacterium animalis ssp. lactis 420 mitigates autoimmune hepatitis through regulating intestinal barrier and liver immune cells[J]. Front Immunol, 2020, 11: 569104. DOI: 10.3389/fimmu.2020.569104. [26] MANGIN I, DOSSOU-YOVO F, LÉVÊQUE C, et al. Oral administration of viable Bifidobacterium pseudolongum strain Patronus modified colonic microbiota and increased mucus layer thickness in rat[J]. FEMS Microbiol Ecol, 2018, 94(11): fiy177. DOI: 10.1093/femsec/fiy177. [27] SEREGIN SS, GOLOVCHENKO N, SCHAF B, et al. NLRP6 protects Il10-/- mice from colitis by limiting colonization of akkermansia muciniphila[J]. Cell Rep, 2017, 19(4): 733-745. DOI: 10.1016/j.celrep.2017.03.080. -



 PDF下载 ( 9148 KB)
PDF下载 ( 9148 KB)


 下载:
下载: