肝硬化合并骨质疏松症的危险因素、发病机制及治疗进展
DOI: 10.3969/j.issn.1001-5256.2023.04.028
利益冲突声明:所有作者均声明不存在利益冲突。
作者贡献声明:金秋负责文献检索、文章构思并撰写论文;杨婧负责指导论文撰写与修改;马红琳、李苹菊、胡绍山、刘清清参与文献检索和文献分析。
Advances in the risk factors, pathogenesis, and treatment of liver cirrhosis with osteoporosis
-
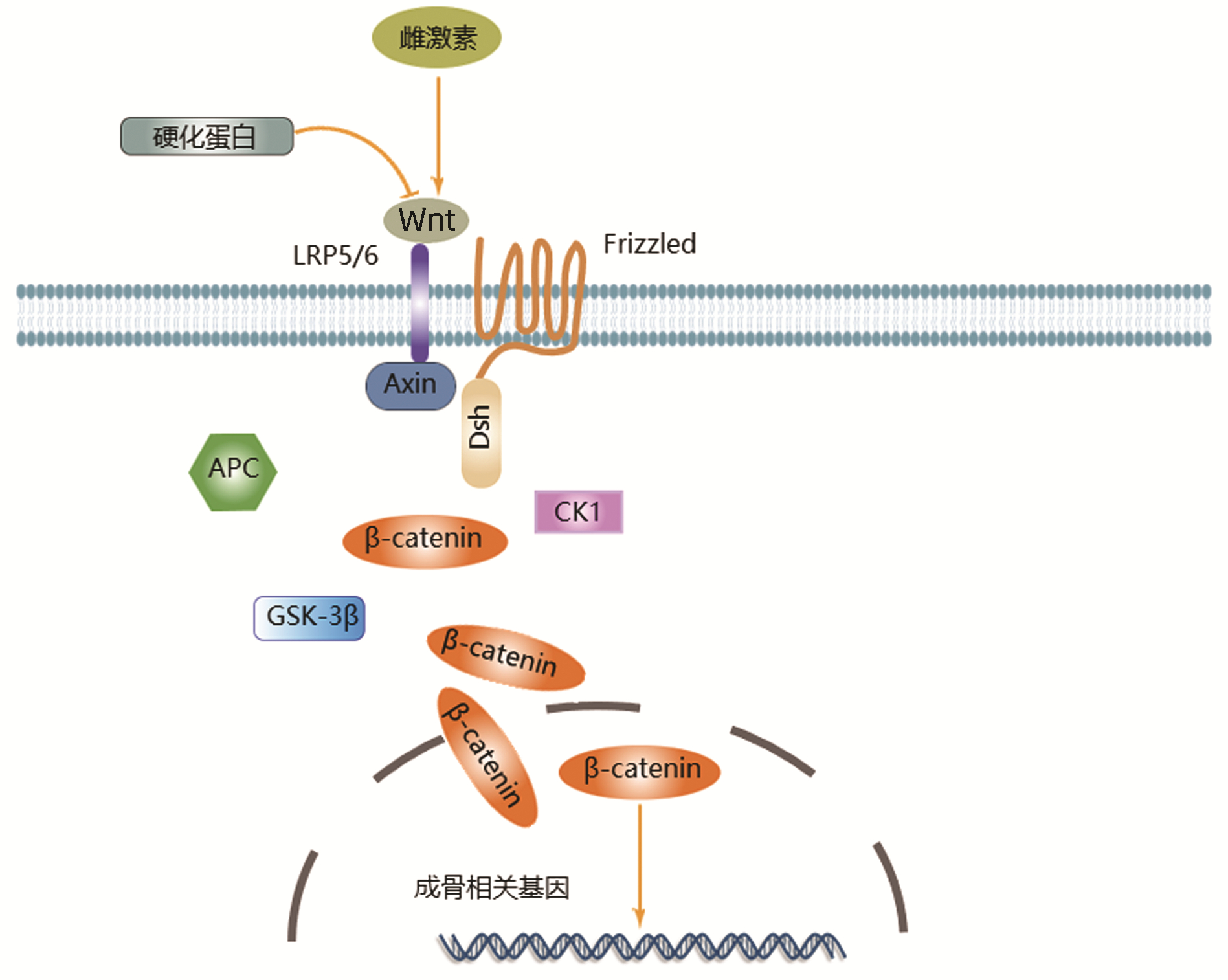
摘要: 骨质疏松症是肝硬化常见的肝外并发症,合并骨质疏松不仅增加患者经济负担而且给患者的生活质量和预后带来不良影响。近年研究发现肌肉减少症、脂联素、瘦素、鸢尾素和炎症因子等参与了肝硬化骨质疏松的发生,常用的抗骨质疏松药物有钙剂、维生素D和双膦酸盐等。本文总结了肝硬化合并骨质疏松的危险因素、发病机制和治疗的研究进展,指出部分因子对骨质疏松的影响尚存争议,仍需进一步探究相关发病机制以及探索更多安全有效的治疗方案。Abstract: Osteoporosis is a common extrahepatic complication of liver cirrhosis, and it not only increases the economic burden of patients, but also brings adverse effects on their quality of life and prognosis. Recent studies have shown that sarcopenia, adiponectin, leptin, irisin, and inflammatory factors are involved in the development of osteoporosis in patients with liver cirrhosis, and commonly used anti-osteoporosis drugs include calcium supplement, vitamin D, and bisphosphonates. This article reviews the advances in the risk factors, pathogenesis, and treatment of liver cirrhosis with osteoporosis and points out that there are still controversies over the influence of some factors on osteoporosis, and further studies are needed to explore related pathogeneses and safe and effective treatment regimens.
-
Key words:
- Liver Cirrhosis /
- Osteoporosis /
- Sarcopenia /
- Adiponectin /
- Irisin
-
-
[1] XIAO HJ, HAN T. Prevention and treatment of malnutrition, sarcopenia, and osteoporosis in patients with liver cirrhosis[J]. J Clin Hepatol, 2021, 37(1): 26-30. DOI: 10.3969/j.issn.1001-5256.2021.01.006.肖慧娟, 韩涛. 肝硬化患者营养不良、肌肉减少症及骨质疏松的防治[J]. 临床肝胆病杂志, 2021, 37(1): 26-30. DOI: 10.3969/j.issn.1001-5256.2021.01.006. [2] Chinese Society of Osteoporosis and Bone Mineral Research. Guidelines for the diagnosis and management of primary osteoporosis(2017)[J]. Chin J Osteoporos, 2019, 25(3): 281-309. DOI: 10.3969/j.issn.1006-7108.2019.03.001.中华医学会骨质疏松和骨矿盐疾病分会. 原发性骨质疏松症诊疗指南(2017)[J]. 中国骨质疏松杂志, 2019, 25(3): 281-309. DOI: 10.3969/j.issn.1006-7108.2019.03.001. [3] SANTOS LA, LIMA TB, AUGUSTI L, et al. Handgrip strength as a predictor of bone mineral density in outpatients with cirrhosis[J]. J Gastroenterol Hepatol, 2016, 31(1): 229-234. DOI: 10.1111/jgh.13062. [4] ZHU X, YAN H, CHANG X, et al. Association between non-alcoholic fatty liver disease-associated hepatic fibrosis and bone mineral density in postmenopausal women with type 2 diabetes or impaired glucose regulation[J]. BMJ Open Diabetes Res Care, 2020, 8(1): e000999. DOI: 10.1136/bmjdrc-2019-000999. [5] ZHANG W, GONG H, SU Z, et al. Risk factors associated with hepatic osteopathy in HBV related cirrhosis measured by liver stiffness: An Observational study[J]. Medicine (Baltimore), 2019, 98(31): e16628. DOI: 10.1097/MD.0000000000016628. [6] ZHANG Y, GAO X, LIU T, et al. Association between osteoporosis and hepatitis B cirrhosis: a case-control study[J]. Afr Health Sci, 2020, 20(4): 1610-1616. DOI: 10.4314/ahs.v20i4.13. [7] EBADI M, TANDON P, MOCTEZUMA-VELAZQUEZ C, et al. Low subcutaneous adiposity associates with higher mortality in female patients with cirrhosis[J]. J Hepatol, 2018, 69(3): 608-616. DOI: 10.1016/j.jhep.2018.04.015. [8] HULDÉN E, CASTEDAL M, KARLSSON MK, et al. Osteoporosis in cirrhotics before and after liver transplantation: relation with malnutrition and inflammatory status[J]. Scand J Gastroenterol, 2020, 55(3): 354-361. DOI: 10.1080/00365521.2020.1735507. [9] SAEKI C, OIKAWA T, KANAI T, et al. Relationship between osteoporosis, sarcopenia, vertebral fracture, and osteosarcopenia in patients with primary biliary cholangitis[J]. Eur J Gastroenterol Hepatol, 2021, 33(5): 731-737. DOI: 10.1097/MEG.0000000000001791. [10] SAEKI C, TAKANO K, OIKAWA T, et al. Comparative assessment of sarcopenia using the JSH, AWGS, and EWGSOP2 criteria and the relationship between sarcopenia, osteoporosis, and osteosarcopenia in patients with liver cirrhosis[J]. BMC Musculoskelet Disord, 2019, 20(1): 615. DOI: 10.1186/s12891-019-2983-4. [11] FUSARO M, CIANCIOLO G, BRANDI ML, et al. Vitamin K and osteoporosis[J]. Nutrients, 2020, 12(12): 3625. DOI: 10.3390/nu12123625. [12] RUIZ-GASPÀ S, GUAÑABENS N, JURADO S, et al. Bile acids and bilirubin effects on osteoblastic gene profile. Implications in the pathogenesis of osteoporosis in liver diseases[J]. Gene, 2020, 725: 144167. DOI: 10.1016/j.gene.2019.144167. [13] JADZIC J, CVETKOVIC D, MILOVANOVIC P, et al. The micro-structural analysis of lumbar vertebrae in alcoholic liver cirrhosis[J]. Osteoporos Int, 2020, 31(11): 2209-2217. DOI: 10.1007/s00198-020-05509-7. [14] WAKOLBINGER R, MUSCHITZ C, SCHERIAU G, et al. Bone microarchitecture and bone turnover in hepatic cirrhosis[J]. Osteoporos Int, 2019, 30(6): 1195-1204. DOI: 10.1007/s00198-019-04870-6. [15] YANG YJ, KIM DJ. An overview of the molecular mechanisms contributing to musculoskeletal disorders in chronic liver disease: Osteoporosis, sarcopenia, and osteoporotic sarcopenia[J]. Int J Mol Sci, 2021, 22(5): 2604. DOI: 10.3390/ijms22052604. [16] MORADI M, DOUSTIMOTLAGH AH, DEHPOUR AR, et al. The influence of TRAIL, adiponectin and sclerostin alterations on bone loss in BDL-induced cirrhotic rats and the effect of opioid system blockade[J]. Life Sci, 2019, 233: 116706. DOI: 10.1016/j.lfs.2019.116706. [17] WAKOLBINGER R, MUSCHITZ C, WALLWITZ J, et al. Serum levels of sclerostin reflect altered bone microarchitecture in patients with hepatic cirrhosis[J]. Wien Klin Wochenschr, 2020, 132(1-2): 19-26. DOI: 10.1007/s00508-019-01595-8. [18] JEONG HM, KIM DJ. Bone diseases in patients with chronic liver disease[J]. Int J Mol Sci, 2019, 20(17): 4270. DOI: 10.3390/ijms20174270. [19] PAL CHINA S, SANYAL S, CHATTOPADHYAY N. Adiponectin signaling and its role in bone metabolism[J]. Cytokine, 2018, 112: 116-131. DOI: 10.1016/j.cyto.2018.06.012. [20] ROOMI AB, NORI W, Al-BADRY SH. The value of serum adiponectin in osteoporotic women: does weight have an effect?[J]. J Obes, 2021, 2021: 5325813. DOI: 10.1155/2021/5325813. [21] DA SILVA TE, COSTA-SILVA M, CORREA CG, et al. Clinical significance of serum adiponectin and resistin levels in liver cirrhosis[J]. Ann Hepatol, 2018, 17(2): 286-299. DOI: 10.5604/01.3001.0010.8659. [22] ZHANG HQ, WANG LJ, LIU SH, et al. Adiponectin regulates bone mass in AIS osteopenia via RANKL/OPG and IL6 pathway[J]. J Transl Med, 2019, 17(1): 64. DOI: 10.1186/s12967-019-1805-7. [23] PETRESCU AD, GRANT S, WILLIAMS E, et al. Leptin enhances hepatic fibrosis and inflammation in a mouse model of cholestasis[J]. Am J Pathol, 2022, 192(3): 484-502. DOI: 10.1016/j.ajpath.2021.11.008. [24] MENG XH, TAN LJ, XIAO HM, et al. Examining the causal role of leptin in bone mineral density: A Mendelian randomization study[J]. Bone, 2019, 125: 25-29. DOI: 10.1016/j.bone.2019.05.006. [25] SZALAY F, FOLHOFFER A, HORVÁTH A, et al. Serum leptin, soluble leptin receptor, free leptin index and bone mineral density in patients with primary biliary cirrhosis[J]. Eur J Gastroenterol Hepatol, 2005, 17(9): 923-928. DOI: 10.1097/00042737-200509000-00007. [26] ZHAO J, QIAO L, DONG J, et al. Antioxidant effects of irisin in liver diseases: mechanistic insights[J]. Oxid Med Cell Longev, 2022, 2022: 3563518. DOI: 10.1155/2022/3563518. [27] CHEN X, SUN K, ZHAO S, et al. Irisin promotes osteogenic differentiation of bone marrow mesenchymal stem cells by activating autophagy via the Wnt//β-catenin signal pathway[J]. Cytokine, 2020, 136: 155292. DOI: 10.1016/j.cyto.2020.155292. [28] GOMARASCA M, BANFI G, LOMBARDI G. Myokines: The endocrine coupling of skeletal muscle and bone[J]. Adv Clin Chem, 2020, 94: 155-218. DOI: 10.1016/bs.acc.2019.07.010. [29] PAZGAN-SIMON M, ZUWALA-JAGIELLO J, MENZYK T, et al. Serum betatrophin and irisin levels in hepatocellular carcinoma[J]. J Physiol Pharmacol, 2020, 71(1): 113-123. DOI: 10.26402/jpp.2020.1.11. [30] WALUGA M, KUKLA M, KOTULSKI R, et al. Omentin, vaspin and irisin in chronic liver diseases[J]. J Physiol Pharmacol, 2019, 70(2): 277-285. DOI: 10.26402/jpp.2019.2.11. [31] SEELY KD, KOTELKO CA, DOUGLAS H, et al. The human gut microbiota: A key mediator of osteoporosis and osteogenesis[J]. Int J Mol Sci, 2021, 22(17): 9452. DOI: 10.3390/ijms22179452. [32] CASTANEDA M, SMITH KM, NIXON JC, et al. Alterations to the gut microbiome impair bone tissue strength in aged mice[J]. Bone Rep, 2021, 14: 101065. DOI: 10.1016/j.bonr.2021.101065. [33] TANG R, WEI Y, LI Z, et al. A common variant in CLDN14 is associated with primary biliary cirrhosis and bone mineral density[J]. Sci Rep, 2016, 6: 19877. DOI: 10.1038/srep19877. [34] YANAGAWA S, TAHARA H, TANAKA Y, et al. Analysis of risk factors affecting incidence of osteoporosis and fragility fractures in liver transplant recipients[J]. Ann Transplant, 2021, 26: e925475. DOI: 10.12659/AOT.925475. [35] PUGLIESE N, ARCARI I, AGHEMO A, et al. Osteosarcopenia in autoimmune cholestatic liver diseases: Causes, management, and challenges[J]. World J Gastroenterol, 2022, 28(14): 1430-1443. DOI: 10.3748/wjg.v28.i14.1430. [36] GROVER I, GUNJAN D, SINGH N, et al. Effect of vitamin D supplementation on vitamin D level and bone mineral density in patients with cirrhosis: A randomized clinical trial[J]. Am J Gastroenterol, 2021, 116(10): 2098-2104. DOI: 10.14309/ajg.0000000000001272. [37] WU HL, ZHENG SH, JING SJ, et al. Research progress on influencing factors and prevention of adverse reac-tions of Zoledronic Acid in the treatment of osteoporosis[J]. China Med Herald, 2021, 18(23): 38-42. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202123009.htm吴鸿亮, 郑思杭, 景胜杰, 等. 唑来膦酸治疗骨质疏松不良反应影响因素及防治的研究进展[J]. 中国医药导报, 2021, 18(23): 38-42. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202123009.htm [38] LIMA TB, SANTOS LAA, NUNES HRC, et al. Safety and efficacy of risedronate for patients with esophageal varices and liver cirrhosis: a non-randomized clinical trial[J]. Sci Rep, 2019, 9(1): 18958. DOI: 10.1038/s41598-019-55603-y. [39] LI XN, WENG W, SHEN ZY, et al. Therapeutic effect of estradiol combined with 1, 25- dihydroxyvitamin D3 on postmenopausal osteoporosis in rats[J]. J Jilin Univ(Med Edit), 2021, 47(4): 857-864. DOI: 10.13481/j.1671-587X.20210406.李希宁, 翁伟, 沈哲源, 等. 雌二醇联合1, 25-二羟维生素D3对绝经后骨质疏松症大鼠的治疗作用[J]. 吉林大学学报(医学版), 2021, 47(4): 857-864. DOI: 10.13481/j.1671-587X.20210406. [40] RUDIC JS, POROPAT G, KRSTIC MN, et al. Hormone replacement for osteoporosis in women with primary biliary cirrhosis[J]. Cochrane Database Syst Rev, 2011(12): CD009146. DOI: 10.1002/14651858.CD009146.pub2. [41] SAEKI C, SAITO M, OIKAWA T, et al. Effects of denosumab treatment in chronic liver disease patients with osteoporosis[J]. World J Gastroenterol, 2020, 26(33): 4960-4971. DOI: 10.3748/wjg.v26.i33.4960. [42] GKOUFA A, ANGELOUSI A, NEONAKI A, et al. Severe symptomatic hypocalcemia associated with denosumab administration in a patient with decompensated cirrhosis and renal dysfunction[J]. Ann Pharmacother, 2022, 56(7): 853-855. DOI: 10.1177/10600280211050216. [43] ZHOU BS, CUI XC, LI CB. A clinical study of the effect of salmon calcitonin in patients with viral cirrhosis complicated with osteoporosis[J]. Chin J Osteoporos, 2018, 24(2): 226-229. DOI: 10.3969/j.issn.1006-7108.2018.02.018.周百岁, 崔晓纯, 李传波. 鲑鱼降钙素对病毒性肝硬化合并骨质疏松症患者影响的临床研究[J]. 中国骨质疏松杂志, 2018, 24(2): 226-229. DOI: 10.3969/j.issn.1006-7108.2018.02.018. -



 PDF下载 ( 2227 KB)
PDF下载 ( 2227 KB)

 下载:
下载:



