巨噬细胞极化及其与邻近细胞串扰在肝细胞癌中的作用
DOI: 10.3969/j.issn.1001-5256.2023.05.032
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:苏会吉负责课题设计,资料分析,撰写论文;颜耿杰、陈含笑、班少群参与收集数据,修改论文;毛德文、韦艾凌、龙富立负责拟定写作思路,指导撰写文章并最后定稿。
Role of macrophage polarization and its crosstalk with neighboring cells in hepatocellular carcinoma
-
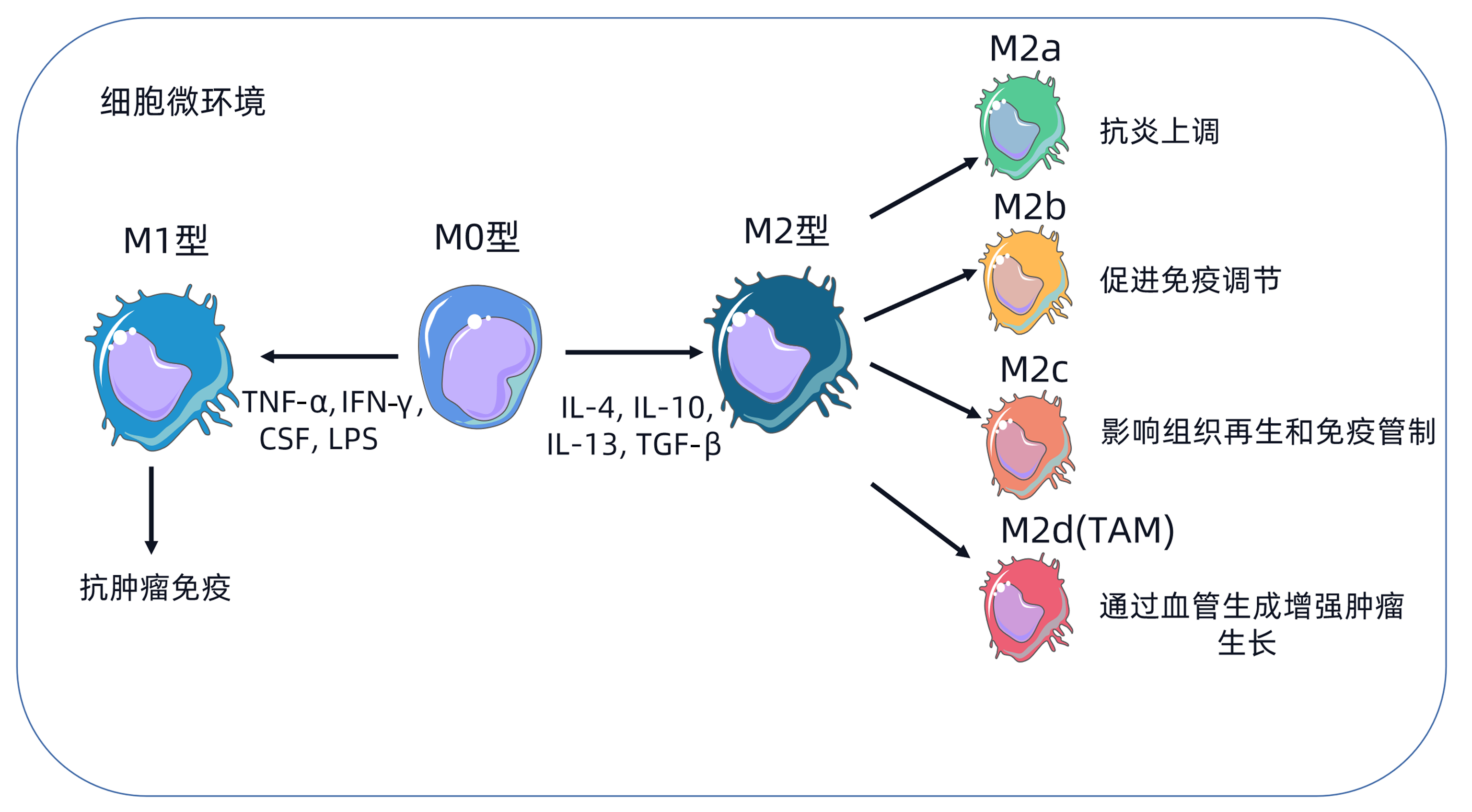
摘要: 炎症与癌症的发生密切相关。肿瘤相关巨噬细胞参与肿瘤相关炎症,促进肿瘤的生长和转移,在一定条件下又表现出细胞毒性和肿瘤杀伤活性,从而抑制癌症的发展。肿瘤相关巨噬细胞与邻近细胞之间的串扰与肝细胞癌的进展和治疗耐药性密切相关。本文综述了巨噬细胞在肝细胞癌中的作用及其细胞间的串扰联系,以期为肝细胞癌的临床诊疗提供新的治疗策略。Abstract: Inflammation is closely associated with the development of cancer. Tumor-associated macrophages (TAM) actively participate in tumor-related inflammation and promote tumor growth and metastasis, while under certain conditions, TAM also show cytotoxicity and tumor killing activity and thus inhibit the progression of cancer. Crosstalk between TAM and neighboring cells is closely associated with the progression of hepatocellular carcinoma (HCC) and drug resistance during treatment. This article summarizes the role of macrophages in HCC and the crosstalk between macrophages and other cells, so as to provide new strategies for the clinical diagnosis and treatment of HCC.
-
Key words:
- Carcinoma, Hepatocellular /
- Macrophages /
- Immunotherapy
-
[1] PINTER M, SCHEINER B, PECK-RADOSAVLJEVIC M. Immunotherapy for advanced hepatocellular carcinoma: a focus on special subgroups[J]. Gut, 2021, 70(1): 204-214. DOI: 10.1136/gutjnl-2020-321702. [2] FANG CH, CAI W. Application of artificial intelligence in the diagnosis and treatment of primary liver cancer[J]. J Clin Hepatol, 2022, 38(1): 26-29. DOI: 10.3969/j.issn.1001-5256.2022.01.004.方驰华, 蔡伟. 人工智能在原发性肝癌诊疗中的应用[J]. 临床肝胆病杂志, 2022, 38(1): 26-29. DOI: 10.3969/j.issn.1001-5256.2022.01.004. [3] FINN RS, QIN S, IKEDA M, et al. Atezolizumab plus Bevacizumab in unresectable hepatocellular carcinoma[J]. N Engl J Med, 2020, 382(20): 1894-1905. DOI: 10.1056/NEJMoa1915745. [4] RIZVI S, WANG J, EL-KHOUEIRY AB. Liver cancer immunity[J]. Hepatology, 2021, 73(Suppl 1): 86-103. DOI: 10.1002/hep.31416. [5] RITZ T, KRENKEL O, TACKE F. Dynamic plasticity of macrophage functions in diseased liver[J]. Cell Immunol, 2018, 330: 175-182. DOI: 10.1016/j.cellimm.2017.12.007. [6] ESHGHJOO S, KIM DM, JAYARAMAN A, et al. Macrophage polarization in atherosclerosis[J]. Genes (Basel), 2022, 13(5): 756. DOI: 10.3390/genes13050756. [7] ANDERSON NR, MINUTOLO NG, GILL S, et al. Macrophage-based approaches for cancer immunotherapy[J]. Cancer Res, 2021, 81(5): 1201-1208. DOI: 10.1158/0008-5472.CAN-20-2990. [8] SHAPOURI-MOGHADDAM A, MOHAMMADIAN S, VAZINI H, et al. Macrophage plasticity, polarization, and function in health and disease[J]. J Cell Physiol, 2018, 233(9): 6425-6440. DOI: 10.1002/jcp.26429. [9] OSIPOV A, MURPHY A, ZHENG L. From immune checkpoints to vaccines: The past, present and future of cancer immunotherapy[J]. Adv Cancer Res, 2019, 143: 63-144. DOI: 10.1016/bs.acr.2019.03.002. [10] REICHEL D, TRIPATHI M, PEREZ JM. Biological effects of nanoparticles on macrophage polarization in the tumor microenvironment[J]. Nanotheranostics, 2019, 3(1): 66-88. DOI: 10.7150/ntno.30052. [11] XIANG W, SHI R, KANG X, et al. Monoacylglycerol lipase regulates cannabinoid receptor 2-dependent macrophage activation and cancer progression[J]. Nat Commun, 2018, 9(1): 2574. DOI: 10.1038/s41467-018-04999-8. [12] HAM S, LIMA LG, LEK E, et al. The impact of the cancer microenvironment on macrophage phenotypes[J]. Front Immunol, 2020, 11: 1308. DOI: 10.3389/fimmu.2020.01308. [13] MEI J, XIAO Z, GUO C, et al. Prognostic impact of tumor-associated macrophage infiltration in non-small cell lung cancer: A systemic review and meta-analysis[J]. Oncotarget, 2016, 7(23): 34217-34228. DOI: 10.18632/oncotarget.9079. [14] CHEN Y, SONG Y, DU W, et al. Tumor-associated macrophages: an accomplice in solid tumor progression[J]. J Biomed Sci, 2019, 26(1): 78. DOI: 10.1186/s12929-019-0568-z. [15] BOHN T, RAPP S, LUTHER N, et al. Tumor immunoevasion via acidosis-dependent induction of regulatory tumor-associated macrophages[J]. Nat Immunol, 2018, 19(12): 1319-1329. DOI: 10.1038/s41590-018-0226-8. [16] YANG Y, YE YC, CHEN Y, et al. Crosstalk between hepatic tumor cells and macrophages via Wnt/β-catenin signaling promotes M2-like macrophage polarization and reinforces tumor malignant behaviors[J]. Cell Death Dis, 2018, 9(8): 793. DOI: 10.1038/s41419-018-0818-0. [17] CHEN MM, XIAO X, LAO XM, et al. Polarization of tissue-resident TFH-like cells in human hepatoma bridges innate monocyte inflammation and M2b macrophage polarization[J]. Cancer Discov, 2016, 6(10): 1182-1195. DOI: 10.1158/2159-8290.CD-16-0329. [18] ZHANG YL, LI Q, YANG XM, et al. SPON2 promotes M1-like macrophage recruitment and inhibits hepatocellular carcinoma metastasis by distinct integrin-Rho GTPase-Hippo pathways[J]. Cancer Res, 2018, 78(9): 2305-2317. DOI: 10.1158/0008-5472.CAN-17-2867. [19] LIU N, WANG X, STEER CJ, et al. MicroRNA-206 promotes the recruitment of CD8+ T cells by driving M1 polarisation of Kupffer cells[J]. Gut, 2022, 71(8): 1642-1655. DOI: 10.1136/gutjnl-2021-324170. [20] XU J, LIN H, WU G, et al. IL-6/STAT3 is a promising therapeutic target for hepatocellular carcinoma[J]. Front Oncol, 2021, 11: 760971. DOI: 10.3389/fonc.2021.760971. [21] WANG TT, YUAN JH, MA JZ, et al. CTGF secreted by mesenchymal-like hepatocellular carcinoma cells plays a role in the polarization of macrophages in hepatocellular carcinoma progression[J]. Biomed Pharmacother, 2017, 95: 111-119. DOI: 10.1016/j.biopha.2017.08.004. [22] SUN Y, WU L, ZHONG Y, et al. Single-cell landscape of the ecosystem in early-relapse hepatocellular carcinoma[J]. Cell, 2021, 184(2): 404-421. DOI: 10.1016/j.cell.2020.11.041. [23] LI X, YAO W, YUAN Y, et al. Targeting of tumour-infiltrating macrophages via CCL2/CCR2 signalling as a therapeutic strategy against hepatocellular carcinoma[J]. Gut, 2017, 66(1): 157-167. DOI: 10.1136/gutjnl-2015-310514. [24] LI X, CHEN L, PENG X, et al. Progress of tumor-associated macrophages in the epithelial-mesenchymal transition of tumor[J]. Front Oncol, 2022, 12: 911410. DOI: 10.3389/fonc.2022.911410. [25] GUO B, LI L, GUO J, et al. M2 tumor-associated macrophages produce interleukin-17 to suppress oxaliplatin-induced apoptosis in hepatocellular carcinoma[J]. Oncotarget, 2017, 8(27): 44465-44476. DOI: 10.18632/oncotarget.17973. [26] WEI Y, SHI D, LIANG Z, et al. IL-17A secreted from lymphatic endothelial cells promotes tumorigenesis by upregulation of PD-L1 in hepatoma stem cells[J]. J Hepatol, 2019, 71(6): 1206-1215. DOI: 10.1016/j.jhep.2019.08.034. [27] SIA D, JIAO Y, MARTINEZ-QUETGLAS I, et al. Identification of an immune-specific class of hepatocellular carcinoma, based on molecular features[J]. Gastroenterology, 2017, 153(3): 812-826. DOI: 10.1053/j.gastro.2017.06.007. [28] KE M, ZHANG Z, CONG L, et al. MicroRNA-148b-colony-stimulating factor-1 signaling-induced tumor-associated macrophage infiltration promotes hepatocellular carcinoma metastasis[J]. Biomed Pharmacother, 2019, 120: 109523. DOI: 10.1016/j.biopha.2019.109523. [29] LI Z, LI H, ZHAO ZB, et al. SIRT4 silencing in tumor-associated macrophages promotes HCC development via PPARδ signalling-mediated alternative activation of macrophages[J]. J Exp Clin Cancer Res, 2019, 38(1): 469. DOI: 10.1186/s13046-019-1456-9. [30] PU Z, DUDA DG, ZHU Y, et al. VCP interaction with HMGB1 promotes hepatocellular carcinoma progression by activating the PI3K/AKT/mTOR pathway[J]. J Transl Med, 2022, 20(1): 212. DOI: 10.1186/s12967-022-03416-5. [31] DEBACKER JM, GONDRY O, LAHOUTTE T, et al. The prognostic value of CD206 in solid malignancies: A systematic review and meta-analysis[J]. Cancers (Basel), 2021, 13(14): 3422. DOI: 10.3390/cancers13143422. [32] WU X, LUO H, SHI B, et al. Combined antitumor effects of sorafenib and GPC3-CAR T cells in mouse models of hepatocellular carcinoma[J]. Mol Ther, 2019, 27(8): 1483-1494. DOI: 10.1016/j.ymthe.2019.04.020. [33] CHEN R, LI Q, XU S, et al. Modulation of the tumour microenvironment in hepatocellular carcinoma by tyrosine kinase inhibitors: from modulation to combination therapy targeting the microenvironment[J]. Cancer Cell Int, 2022, 22(1): 73. DOI: 10.1186/s12935-021-02435-4. [34] LEE TK, GUAN XY, MA S. Cancer stem cells in hepatocellular carcinoma - from origin to clinical implications[J]. Nat Rev Gastroenterol Hepatol, 2022, 19(1): 26-44. DOI: 10.1038/s41575-021-00508-3. [35] YIN Z, MA T, LIN Y, et al. IL-6/STAT3 pathway intermediates M1/M2 macrophage polarization during the development of hepatocellular carcinoma[J]. J Cell Biochem, 2018, 119(11): 9419-9432. DOI: 10.1002/jcb.27259. [36] ZHONG CQ, ZHANG XP, MA N, et al. FABP4 suppresses proliferation and invasion of hepatocellular carcinoma cells and predicts a poor prognosis for hepatocellular carcinoma[J]. Cancer Med, 2018, 7(6): 2629-2640. DOI: 10.1002/cam4.1511. [37] XUE ST, LI K, GAO Y, et al. The role of the key autophagy kinase ULK1 in hepatocellular carcinoma and its validation as a treatment target[J]. Autophagy, 2020, 16(10): 1823-1837. DOI: 10.1080/15548627.2019.1709762. [38] LIU LZ, ZHANG Z, ZHENG BH, et al. CCL15 recruits suppressive monocytes to facilitate immune escape and disease progression in hepatocellular carcinoma[J]. Hepatology, 2019, 69(1): 143-159. DOI: 10.1002/hep.30134. [39] LIU C, CHIKINA M, DESHPANDE R, et al. Treg cells promote the SREBP1-dependent metabolic fitness of tumor-promoting macrophages via repression of CD8+ T cell-derived interferon-γ[J]. Immunity, 2019, 51(2): 381-397. DOI: 10.1016/j.immuni.2019.06.017. [40] SUNG PS, YOON SK, JANG JW, et al. Inflammation-induced IgA plus tumor-associated macrophages express PD-L1 and causes impaired T cell functionality in hepatocellular carcinoma[J]. Hepatology, 2020, 72(Suppl 1): 780A-781A. [41] HSU BE, ROY J, MOUHANNA J, et al. C3a elicits unique migratory responses in immature low-density neutrophils[J]. Oncogene, 2020, 39(12): 2612-2623. DOI: 10.1038/s41388-020-1169-8. [42] ZHOU Z, WANG P, SUN R, et al. Tumor-associated neutrophils and macrophages interaction contributes to intrahepatic cholangiocarcinoma progression by activating STAT3[J]. J Immunother Cancer, 2021, 9(3): e001946. DOI: 10.1136/jitc-2020-001946. [43] PENG ZP, JIANG ZZ, GUO HF, et al. Glycolytic activation of monocytes regulates the accumulation and function of neutrophils in human hepatocellular carcinoma[J]. J Hepatol, 2020, 73(4): 906-917. DOI: 10.1016/j.jhep.2020.05.004. [44] ZHOU SL, DAI Z, ZHOU ZJ, et al. Overexpression of CXCL5 mediates neutrophil infiltration and indicates poor prognosis for hepatocellular carcinoma[J]. Hepatology, 2012, 56(6): 2242-2254. DOI: 10.1002/hep.25907. [45] WU G, MA Z, CHENG Y, et al. Targeting Gas6/TAM in cancer cells and tumor microenvironment[J]. Mol Cancer, 2018, 17(1): 20. DOI: 10.1186/s12943-018-0769-1. [46] YANG F, WEI Y, HAN D, et al. Interaction with CD68 and regulation of GAS6 expression by endosialin in fibroblasts drives recruitment and polarization of macrophages in hepatocellular carcinoma[J]. Cancer Res, 2020, 80(18): 3892-3905. DOI: 10.1158/0008-5472. -



 PDF下载 ( 2693 KB)
PDF下载 ( 2693 KB)

 下载:
下载:



