五种评分系统预测高甘油三酯血症性急性胰腺炎严重程度的比较
DOI: 10.3969/j.issn.1001-5256.2023.06.020
Value of five scoring systems in predicting the severity of hyperlipidemic acute pancreatitis: A comparative analysis
-
摘要:
目的 探讨PASS评分、BISAP评分、APACHE-Ⅱ评分、HAPS评分和Ranson评分五种评分系统对高甘油三酯血症性急性胰腺炎(HTGAP)病情和预后评估的价值。 方法 回顾性分析宁夏医科大学总医院2016年1月—2022年1月收治的300例HTGAP患者的临床资料,根据患者病情程度分为轻症急性胰腺炎、中度重症急性胰腺炎、重症急性胰腺炎三个组别,比较三组患者的临床资料和评分系统差异,计数资料组间比较采用χ2检验,正态方差齐的计量资料采用方差分析,非正态分布的计量资料三组间比较采用Kruskal-Wallis H检验。根据病情程度是否重症,绘制受试者工作特征曲线(ROC曲线),比较指标的ROC曲线下面积(AUC)。 结果 三组间PASS评分(χ2=219.351)、Ranson评分(χ2=83.084)、APACHE-Ⅱ评分(χ2=43.388)和BISAP评分(χ2=50.785)差异均有统计学意义(P值均<0.01)。在病情严重程度的评估和预测方面, PASS评分的敏感度(0.945)和AUC(0.963)高于其他四种评分系统,Ranson评分的敏感度(0.655)和AUC(0.819)次之。 结论 对于HTGAP患者,PASS评分可以更准确地评估HTGAP患者的病情严重程度及预后,有望在临床中更好的推广应用。 -
关键词:
- 胰腺炎, 急性坏死性 /
- 高甘油三酯血症 /
- 疾病严重程度指数
Abstract:Objective To investigate the value of pancreatitis activity scoring system (PASS) score, Bedside Index for Severity in Acute Pancreatitis (BISAP) score, Acute Physiology and Chronic Health Evaluation Ⅱ (APACHE-Ⅱ) score, harmless acute pancreatitis score (HAPS), and Ranson score in evaluating the severity and prognosis of hypertriglyceridemia acute pancreatitis (HTGAP). Methods A retrospective analysis was performed for the clinical data of 300 patients with HTGAP who were admitted to General Hospital of Ningxia Medical University from January 2016 to January 2022, and according to the disease severity, these patients were divided into mild acute pancreatitis (MAP) group, moderate-severe acute pancreatitis (MSAP) group, and severe acute pancreatitis (SAP) group. Clinical data and the above scores were compared between the three groups. The chi-square test was used for comparison of categorical data between groups; an analysis of variance was used for continuous data with homogeneity of variance, and the Kruskal-Wallis H test was used for comparison of non-normally distributed continuous data between groups. The receiver operating characteristic (ROC) curve was plotted according to disease severity, and related indicators were compared in terms of the area under the ROC curve (AUC). Results There were significant differences between the three groups in PASS score (F=219.351, P < 0.01), Ranson score (χ2=83.084, P < 0.01), APACHE-Ⅱ score (χ2=43.388, P < 0.01), and BISAP score (χ2= 50.785, P < 0.01). Compared with the other four scoring systems in evaluating and predicting disease severity, PASS score had the highest sensitivity of 0.945 and the largest AUC of 0.963, followed by Ranson score with a sensitivity of 0.655 and an AUC of 0.819. Conclusion For patients with HTGAP, PASS score can more accurately assess the severity and prognosis of HTGAP patients and thus holds promise for clinical application. -
急性胰腺炎(AP)是临床常见急症之一,病死率较高,近年来,高脂血症已成为引起AP的第二大常见病因[1-2],与胆源性胰腺炎相比,高甘油三酯血症性急性胰腺炎(hypertriglyceridemia acute pancreatitis,HTGAP)患者趋向年轻化,重症化倾向更明显,并发症多并且病死率高[3]。为了更好地判断AP的严重程度及预后,国内外提出了许多评分系统,但少有研究对HTGAP的严重程度进行相对全面的比较。本研究回顾性分析HTGAP患者的临床资料,探讨五种评分系统对HTGAP病情和预后的预测价值。
1. 资料与方法
1.1 研究对象
本研究收集了宁夏医科大学总医院2016年1月— 2022年1月收治的HTGAP患者。纳入标准:(1)AP诊断标准符合2019年发布的中国急性胰腺炎诊治指南[4];(2) HTGAP诊断标准为血甘油三酯(TG)>11.3 mmol/L,或血TG水平在5.56~11.3 mmol/L且血清呈乳糜状。排除其他如酒精性、自身免疫性、胆源性、药物性等病因所致的AP。
1.2 研究方法
收集患者的临床病历资料,记录如下信息。(1)一般资料:年龄、性别、BMI等;(2)既往史、个人史、合并症、药物服用史等;(3)入院24 h实验室检查结果;(4)根据患者入院24 h内的病历资料进行HAPS评分、BISAP评分和APACHE-Ⅱ评分,根据48 h内的病历资料进行Ranson评分,根据患者临床资料进行PASS评分,进而根据患者病历资料评估病情严重程度及预后[5],每项指标均选择最为异常的数据进行评分。
1.3 统计学方法
采用SPSS 24.0软件对数据进行统计学分析。符合正态分布的计量资料以x±s表示,组间比较采用单因素方差分析;偏态资料以M(P25~P75)表示,三组间比较采用Kruskal-Wallis H秩和检验。计数资料组间比较采用χ2检验。并绘制受试者工作特征曲线(ROC曲线),计算敏感度、特异度、约登指数、95%CI、标准误,以最大约登指数对应的值为临界值(cut-off值),比较指标的ROC曲线下面积(AUC)。P<0.05为差异有统计学意义。
2. 结果
2.1 一般情况
共收集300例患者,其中男247例,女53例,年龄19~70岁,平均(36.8±8.7)岁。根据患者病情程度分为轻症急性胰腺炎(MAP)、中度重症急性胰腺炎(MSAP)和重症急性胰腺炎(SAP),三组患者分别占比为66.3%(199例)、16.1%(48例)和17.6%(53例),经比较三组间性别、年龄、BMI等基线资料差异均无统计学意义,对入院患者的生命体征进行比较,结果提示SAP组和MSAP患者呼吸频率明显高于MAP组,差异均有统计学意义(P值均<0.01),但三组患者心率差异无统计学意义;其次,本研究针对三组患者的个人史(吸烟史、饮酒史)、既往药物服用史、合并症(脂肪肝、代谢综合征及腹腔积液)进行比较,差异均无统计学意义,但经比较,SAP组患者合并呼吸衰竭、SIRS、代谢性酸中毒、脓毒症、MODS及胸腔积液的比例明显升高,且差异均有统计学意义(P值均<0.01)(表 1)。
表 1 3组患者一般情况比较Table 1. Comparison of the general information among the three groups指标 MAP(n=199) MSAP(n=48) SAP(n=53) 统计值 P值 年龄(岁) 35.0(30.0~40.0) 37.0(29.5~45.0) 36.0(31.3~42.8) χ2=2.518 0.284 BMI(kg/m2) 26.29(23.86~29.27) 27.34(25.47~28.52) 26.74(24.13~29.42) χ2=2.180 0.336 呼吸(次/min) 20(20~21) 21(20~21) 21(20~21) χ2=15.989 <0.001 心率(次/min) 26.74±4.48 26.50±4.46 36.21±8.61 F=0.608 0.545 性别[例(%)] χ2=1.263 0.540 男 167(83.9) 36(75.0) 44(83.0) 女 32(16.1) 12(25.0) 9(17.0) 吸烟[例(%)] 93(46.7) 23(47.9) 20(37.7) χ2=2.906 0.241 饮酒[例(%)] 80(40.2) 23(47.9) 21(39.6) χ2=2.180 0.349 药物服用史[例(%)] 39(19.6) 5(10.4) 13(24.5) χ2=2.531 0.286 合并脂肪肝[例(%)] 145(72.9) 38(79.2) 38(71.7) χ2=3.701 0.160 合并糖尿病[例(%)] 57(28.6) 16(33.3) 27(50.9) χ2=7.507 0.024 合并呼吸衰竭[例(%)] 0(0.0) 1(2.1) 4(7.5) χ2=11.241 0.002 合并高血压病[例(%)] 19(9.5) 5(10.4) 6(11.3) χ2=0.300 0.880 合并代谢性酸中毒[例(%)] 0(0.0) 1(2.1) 4(7.5) χ2=11.241 0.002 合并SIRS[例(%)] 0(0.0) 0(0.0) 4(7.5) χ2=11.139 0.002 合并脓毒症[例(%)] 0(0.0) 0(0.0) 4(7.5) χ2=11.139 0.002 合并MODS[例(%)] 0(0.0) 0(0.0) 4(7.5) χ2=11.139 0.002 合并胸腔积液[例(%)] 1(0.5) 3(6.3) 8(15.1) χ2=19.961 <0.001 合并腹腔积液[例(%)] 2(1.0) 0(0.0) 2(3.8) χ2=2.331 0.265 代谢综合征[例(%)] 5(2.5) 2(4.2) 1(1.9) χ2=0.958 0.749 注:SIRS,全身炎症反应综合征;MODS,多器官功能障碍综合征。 2.2 临床资料比较
本研究回顾性分析患者入院24 h的实验室检查资料,根据统计分析结果提示三组间白细胞计数(WBC)、中性粒细胞绝对值(NEUT#)、D-二聚体(D-dimer)、国际标准化比值(INR)、凝血酶原时间(PT)、空腹血糖(GLU)、血钙(Ca)、血尿素(BUN)、白蛋白(Alb)、乳酸脱氢酶(LDH)、血淀粉酶(AMY)、血脂肪酶(LIP)、C反应蛋白(CRP)、淋巴细胞绝对值(LYM) 差异均有统计学意义(P值均<0.05),提示上述指标为重症HTGAP发生的危险因素(表 2)。
表 2 三组患者实验室检验结果比较Table 2. Comparison of laboratory results among the three groups指标 MAP(n=199) MSAP(n=48) SAP(n=53) 统计值 P值 WBC(×109/L) 110.41±18.41 20.78±1.09 22.05±3.69 F=9.424 <0.001 NEUT#(%) 100.44±74.12 20.90±2.36 20.61±1.97 F=10.758 <0.001 LYM(×109/L) 1.520(1.180~2.210) 1.410(1.115~1.920) 1.250(0.800~1.620) χ2=11.328 0.003 MXD(×109/L) 0.705(0.520~0.900) 0.700(0.570~1.000) 0.690(0.553~0.983) χ2=1.486 0.476 PTL(×109/L) 7.35±0.09 105.09±15.74 110.41±18.42 F=1.544 0.215 HCT(%) 45.70(42.80~48.40) 46.70(43.30~49.20) 46.95(41.55~50.60) χ2=1.959 0.376 D-dimer(μg/mL) 0.30(0.20~0.64) 0.32(0.20~0.76) 0.82(0.34~1.96) χ2=25.235 <0.001 PT(s) 11.00(10.00~11.00) 11.20(10.15~11.75) 11.80(10.80~13.00) χ2=19.045 <0.001 INR 0.95(0.89~1.00) 0.960(0.865~1.025) 1.02(0.94~1.12) χ2=25.617 <0.001 GLU(mmol/L) 8.235(6.190~12.163) 9.440(6.895~14.325) 12.770(9.325~17.588) χ2=27.509 <0.001 Ca(mmol/L) 2.310(2.210~2.390) 2.250(2.090~2.360) 2.060(1.785~2.218) χ2=45.766 <0.001 K(mmol/L) 4.165(3.948~4.445) 4.210(3.910~4.350) 4.150(3.905~4.810) χ2=0.613 0.736 BUN(mmol/L) 4.275(3.450~5.393) 4.320(3.645~5.285) 5.390(3.915~6.635) χ2=11.603 0.003 CREA(μmol/L) 61.900(54.100~71.300) 58.600(51.350~68.950) 62.000(50.025~83.750) χ2=2.224 0.329 UA(μmol/L) 405.50(346.75~484.25) 375.00(329.50~480.50) 414.00(307.00~493.00) χ2=0.516 0.773 Alb(g/L) 43.850(40.780~46.930) 42.800(39.500~46.900) 38.700(34.350~43.025) χ2=24.657 <0.001 LDH(U/L) 531.00(432.25~633.25) 659.00(513.50~819.00) 780.00(480.75~1 268.75) χ2=39.743 <0.001 TC(mmol/L) 6.880(5.770~8.520) 7.460(6.200~10.425) 7.000(6.268~9.540) χ2=2.885 0.236 TG(mmol/L) 12.635(10.770~21.683) 11.860(11.850~24.975) 13.910(8.503~27.740) χ2=0.669 0.716 AMY(U/L) 196.00(90.75~358.00) 292.00(140.50~440.00) 411.00(190.00~607.50) χ2=17.024 <0.001 LIP(U/L) 1 161.5(434.0~3 641.0) 922.0(554.0~3 109.5) 2 283.0(1 016.0~5 589.0) χ2=9.880 0.007 CRP(mg/L) 89.00(45.00~136.00) 136.00(79.75~273.75) 154.50(90.00~255.50) χ2=28.317 <0.001 2.3 五种评分系统及临床结局比较
本研究结果显示,三组间PASS评分、Ranson评分、APACHE-Ⅱ评分和BISAP评分系统差异均有统计学意义(P值均<0.01);对三组患者的疾病转归进行比较,根据统计分析结果提示三组间住院天数、住院费用、入住ICU率和复发率差异均有统计学意义(P值均<0.05),但三组间死亡率差异均无统计学意义(P值均>0.05)(表 3)。
表 3 三组患者评分系统和疾病转归及预后比较Table 3. Comparison of scoring systems, disease outcome, and prognosis among the three groups of patients指标 MAP(n=199) MSAP(n=48) SAP(n=53) χ2值 P值 PASS评分 90.0(90.0~90.0) 140.0(115.0~140.0) 200.0(152.5~220.0) 219.351 <0.001 Ranson评分 1(1~2) 2(2~2) 2(2~2) 83.084 <0.001 HAPS评分 1(1~1) 1(1~1) 1(0~1) 0.480 0.799 APACHE-Ⅱ评分 1(1~1) 1(1~2) 2(1~2) 43.388 <0.001 BISAP评分 0(0~0) 0(0~0) 0(0~1) 50.785 <0.001 住院天数(d) 7.00(4.00~9.00) 11.00(8.00~14.50) 10.00(6.25~15.75) 48.281 <0.001 住院费用(元) 10 713(7 200~17 224) 17 027(11 800~24 020) 31 189(21 395~47 700) 93.894 <0.001 ICU[例(%)] 0(0.0) 0(0.0) 6(11.3) 17.317 <0.001 死亡[例(%)] 0(0.0) 0(0.0) 1(1.9) 3.662 0.338 复发[例(%)] 91(45.7) 14(29.2) 36(67.9) 11.357 0.003 2.4 五种评分对HTGAP病情严重程度、并发症和死亡的评估
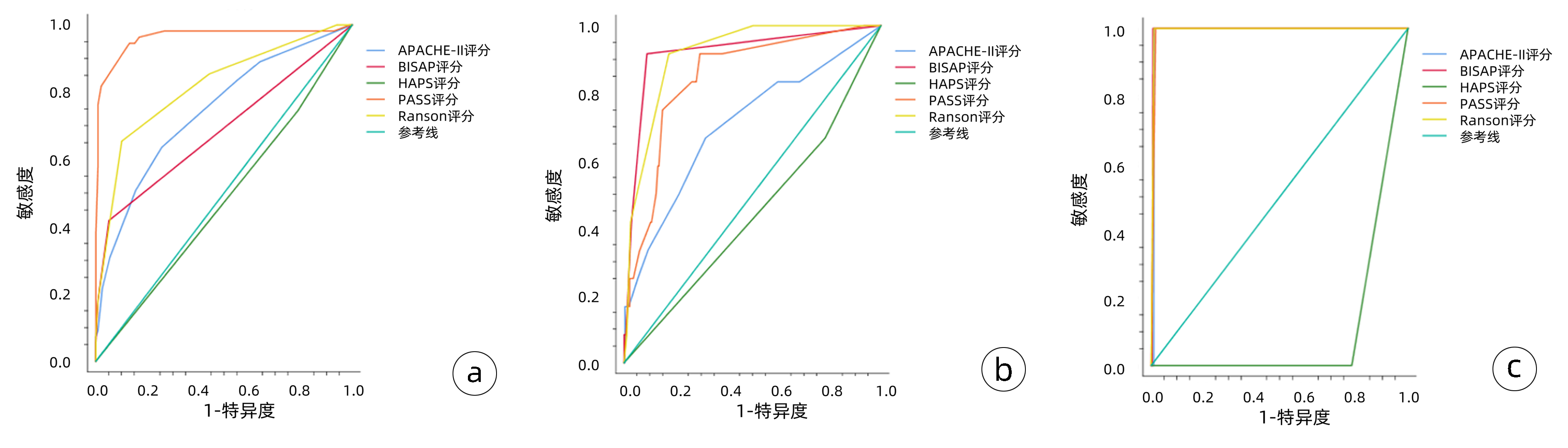
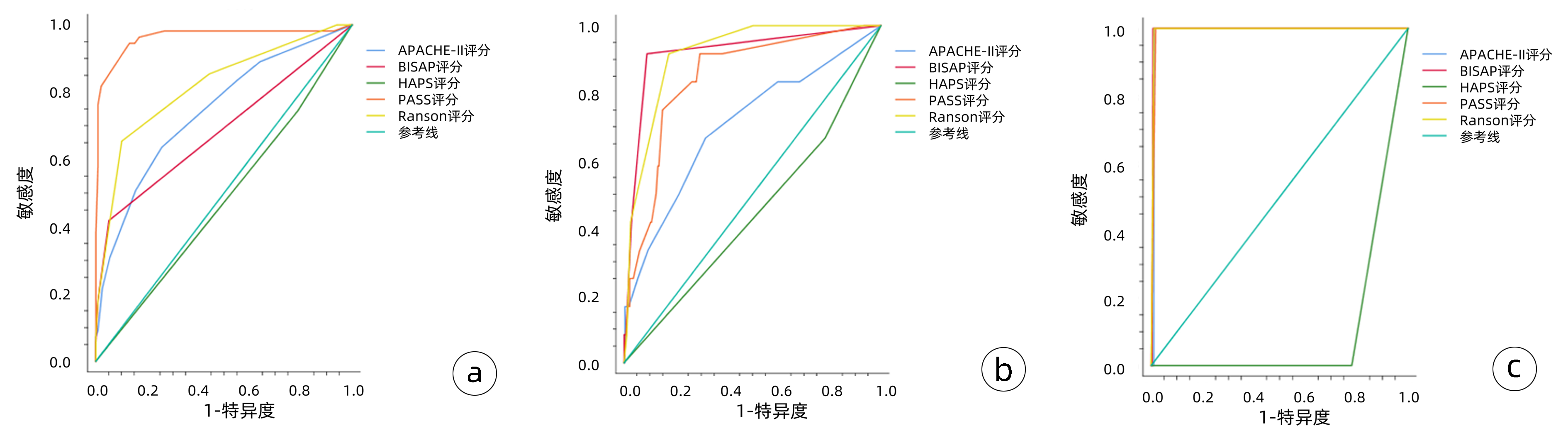
(1) 对病情严重程度(MSAP、SAP) 的预测: PASS评分的敏感度(0.945)和AUC(0.963)高于其他四种评分系统,Ranson评分的敏感度(0.655)和AUC(0.819)次之,HAPS评分AUC仅为0.478;(2)对并发症的预测:对于胸腔积液评估的AUC比较,BISAP评分>Ranson评分>PASS评分>APACHE-Ⅱ评分;(3)对于死亡的预测:BISAP评分和Ranson评分的AUC最高,均为0.995(表 4)。
表 4 五种评分系统对HTGAP患者病情严重程度、并发症和死亡的评估准确性比较Table 4. Comparison of the accuracy of the five scoring systems in evaluating patients' severity of disease, complications, and mortality评分系统及预后指标 AUC P值 敏感度 特异度 阳性预测值 阳性似然比 约登指数 APACHE-Ⅱ MSAP、SAP 0.744 <0.001 0.636 0.743 0.712 2.472 0.379 胸腔积液 0.704 0.016 0.683 0.350 0.678 2.105 0.350 死亡 0.990 <0.001 1.000 0.990 0.990 97.333 0.990 BISAP MSAP、SAP 0.687 <0.001 0.418 0.949 0.892 8.259 0.368 胸腔积液 0.919 <0.001 0.917 0.911 0.912 10.303 0.828 死亡 0.995 <0.001 1.000 0.993 0.993 146.000 0.993 PASS MSAP、SAP 0.963 <0.001 0.945 0.869 0.878 7.288 0.815 胸腔积液 0.846 <0.001 0.917 0.705 0.756 3.103 0.621 死亡 0.991 <0.001 1.000 0.983 0.983 58.400 0.983 Ranson MSAP、SAP 0.819 <0.001 0.655 0.899 0.866 6.464 0.553 胸腔积液 0.916 <0.001 0.917 0.826 0.840 5.257 0.742 死亡 0.995 <0.001 1.000 0.990 0.990 97.333 0.990 HAPS MSAP、SAP 0.418 0.619 0.745 0.211 0.486 0.945 -0.044 胸腔积液 0.442 0.512 0.512 0.217 0.460 0.852 -0.016 死亡 0.110 <0.001 0.000 0.219 0.000 0.000 -0.781 五种评分系统预测AP患者病情严重程度、并发症和死亡的ROC曲线见图 1,图 1a中ROC曲线对五种评分系统预测病情严重程度的准确度进行了比较,其中PASS评分预测病情严重程度的敏感度最高,其次是Ranson评分,HAPS评分对预测病情严重程度无统计学意义。图 1b中ROC曲线对五种评分系统预测并发症的准确度进行了比较,BISAP评分预测并发症的敏感度和特异度最高,其次是Ranson评分,HAPS评分对预测并发症无统计学意义。图 1c中ROC曲线对五种评分系统预测死亡的准确度进行了比较,除外HAPS评分,另外四种评分系统对预测死亡的敏感度、特异度均较高(均>0.90)。
3. 讨论
多个研究[6-7]表明,相较于其他病因所致的AP,HTGAP患者多为年轻人,病情进展更快更重,预后差且复发率高,正因为HTGAP特殊的临床表现,要求临床医师准确并高效的确定疾病的严重程度,对于潜在的重症患者尽早给予特殊的监护措施及治疗方案。目前虽无完美的预测HTGAP病情的工具,但存在一些多因素评分系统(基于临床、实验室、影像学证据)以及单因素评价指标(多为生物标志物),其侧重点和临床价值各不相同[8]。
HTGAP病程具有高度可变的特点, 早期患者可能表现为轻症, 但会迅速发展为危急重症状态, 为了更好地研究、评估和预测疾病发展,2017年国际专家提出了新的胰腺炎活动评分系统(PASS)[9-10],本研究结果显示对于HTGAP病情严重程度的预测: PASS评分的敏感度和AUC均高于其他四种评分系统。既往多数评分系统,大部分聚焦于早期评估HTGAP患者的病情严重程度,PASS评分的提出旨在对患者病程中以12 h为增量进行一次评分,不仅客观评估患者实验室指标,还加入了患者主观感受(如疼痛耐受程度、经口进食耐受程度),从理论上来说更能综合全面评估患者病情[11-12],动态预测不同时间点患者的病情严重程度等能力更优,综上,PASS可能对HTGAP患者的病情预测和干预具有更重要的临床意义,是一项很有前景的定量测量HTGAP患者疾病活动的评分系统。
Ranson评分纳入了11项临床和实验室参数,最初主要用于评估酒精性AP患者的病情。有些研究认为,Ranson评分耗时较长,内容相对繁琐,对临床应用价值不大,但随着对HTGAP发病机制的进一步了解,以及对于HTGAP的规范化治疗,近年来多项临床研究[13-14]证实了Ranson评分系统对于AP的病情严重程度评估的准确性和有效性。本研究发现SAP组的Ranson评分值显著高于其余两组, 其次,Ranson评分对于胸腔积液和死亡的预测能力也较高,这说明采用Ranson评分系统水平能够对HTGAP严重程度及预后进行一定的评价,但不足之处在于第2次评分需在入院48 h后进行,故难以早期预测HTGAP病情的走势。
同多数研究结果一致,BISAP在预测HTGAP严重程度、局部并发症等方面具有较高的准确性,且本研究提示BISAP评分对HTGAP的病情严重程度的预测特异度达94.5%。同时,BISAP评分系统临床数据易获取,操作相对简便,有利于早期指导临床治疗决策[15-17]。因此BISAP评分系统目前仍广泛在临床应用,但该评分系统在是否需要介入或手术干预等方面预测价值有限[18]。
HAPS评分是由Lankisch等经过一项前瞻性研究于2009年提出,该评分将无反跳痛和肌紧张、正常红细胞压积水平和正常血清肌酐水平这3项对非严重病程有最强预测的参数结合起来[8],多数研究提示入院时HAPS评分预测MAP的效能较高[19],但国内外鲜有关于HAPS评分对于HTGAP的大样本评价,本研究结果显示HAPS评分对于HTGAP严重程度的预测AUC仅为0.478,提示HAPS评分对于识别非重症急性胰腺炎有较高的临床价值,但其预测SAP的可靠性较低,对于重症HTGAP的预测价值有待于进一步研究。
本研究存在一定的局限性,单中心研究且样本量有限,回顾性的研究分析数据可能存在偏差,所以目前还需要大样本的、前瞻性、多中心的研究来验证以上评分系统对HTGPA患者病情严重程度及预后的预测作用。
综上所述,对于HTGAP患者,相较于其他四种评分系统,PASS评分可以更准确地评估HTGAP患者的病情严重程度,有望在临床中更好的推广应用。临床医师需要多结合各评分系统的优点,灵活使用每种评分系统的优势,以便及时、有效地评估病情,指导临床医师采取积极的治疗措施,从而降低HTGAP的病死率、改善预后。
-
表 1 3组患者一般情况比较
Table 1. Comparison of the general information among the three groups
指标 MAP(n=199) MSAP(n=48) SAP(n=53) 统计值 P值 年龄(岁) 35.0(30.0~40.0) 37.0(29.5~45.0) 36.0(31.3~42.8) χ2=2.518 0.284 BMI(kg/m2) 26.29(23.86~29.27) 27.34(25.47~28.52) 26.74(24.13~29.42) χ2=2.180 0.336 呼吸(次/min) 20(20~21) 21(20~21) 21(20~21) χ2=15.989 <0.001 心率(次/min) 26.74±4.48 26.50±4.46 36.21±8.61 F=0.608 0.545 性别[例(%)] χ2=1.263 0.540 男 167(83.9) 36(75.0) 44(83.0) 女 32(16.1) 12(25.0) 9(17.0) 吸烟[例(%)] 93(46.7) 23(47.9) 20(37.7) χ2=2.906 0.241 饮酒[例(%)] 80(40.2) 23(47.9) 21(39.6) χ2=2.180 0.349 药物服用史[例(%)] 39(19.6) 5(10.4) 13(24.5) χ2=2.531 0.286 合并脂肪肝[例(%)] 145(72.9) 38(79.2) 38(71.7) χ2=3.701 0.160 合并糖尿病[例(%)] 57(28.6) 16(33.3) 27(50.9) χ2=7.507 0.024 合并呼吸衰竭[例(%)] 0(0.0) 1(2.1) 4(7.5) χ2=11.241 0.002 合并高血压病[例(%)] 19(9.5) 5(10.4) 6(11.3) χ2=0.300 0.880 合并代谢性酸中毒[例(%)] 0(0.0) 1(2.1) 4(7.5) χ2=11.241 0.002 合并SIRS[例(%)] 0(0.0) 0(0.0) 4(7.5) χ2=11.139 0.002 合并脓毒症[例(%)] 0(0.0) 0(0.0) 4(7.5) χ2=11.139 0.002 合并MODS[例(%)] 0(0.0) 0(0.0) 4(7.5) χ2=11.139 0.002 合并胸腔积液[例(%)] 1(0.5) 3(6.3) 8(15.1) χ2=19.961 <0.001 合并腹腔积液[例(%)] 2(1.0) 0(0.0) 2(3.8) χ2=2.331 0.265 代谢综合征[例(%)] 5(2.5) 2(4.2) 1(1.9) χ2=0.958 0.749 注:SIRS,全身炎症反应综合征;MODS,多器官功能障碍综合征。 表 2 三组患者实验室检验结果比较
Table 2. Comparison of laboratory results among the three groups
指标 MAP(n=199) MSAP(n=48) SAP(n=53) 统计值 P值 WBC(×109/L) 110.41±18.41 20.78±1.09 22.05±3.69 F=9.424 <0.001 NEUT#(%) 100.44±74.12 20.90±2.36 20.61±1.97 F=10.758 <0.001 LYM(×109/L) 1.520(1.180~2.210) 1.410(1.115~1.920) 1.250(0.800~1.620) χ2=11.328 0.003 MXD(×109/L) 0.705(0.520~0.900) 0.700(0.570~1.000) 0.690(0.553~0.983) χ2=1.486 0.476 PTL(×109/L) 7.35±0.09 105.09±15.74 110.41±18.42 F=1.544 0.215 HCT(%) 45.70(42.80~48.40) 46.70(43.30~49.20) 46.95(41.55~50.60) χ2=1.959 0.376 D-dimer(μg/mL) 0.30(0.20~0.64) 0.32(0.20~0.76) 0.82(0.34~1.96) χ2=25.235 <0.001 PT(s) 11.00(10.00~11.00) 11.20(10.15~11.75) 11.80(10.80~13.00) χ2=19.045 <0.001 INR 0.95(0.89~1.00) 0.960(0.865~1.025) 1.02(0.94~1.12) χ2=25.617 <0.001 GLU(mmol/L) 8.235(6.190~12.163) 9.440(6.895~14.325) 12.770(9.325~17.588) χ2=27.509 <0.001 Ca(mmol/L) 2.310(2.210~2.390) 2.250(2.090~2.360) 2.060(1.785~2.218) χ2=45.766 <0.001 K(mmol/L) 4.165(3.948~4.445) 4.210(3.910~4.350) 4.150(3.905~4.810) χ2=0.613 0.736 BUN(mmol/L) 4.275(3.450~5.393) 4.320(3.645~5.285) 5.390(3.915~6.635) χ2=11.603 0.003 CREA(μmol/L) 61.900(54.100~71.300) 58.600(51.350~68.950) 62.000(50.025~83.750) χ2=2.224 0.329 UA(μmol/L) 405.50(346.75~484.25) 375.00(329.50~480.50) 414.00(307.00~493.00) χ2=0.516 0.773 Alb(g/L) 43.850(40.780~46.930) 42.800(39.500~46.900) 38.700(34.350~43.025) χ2=24.657 <0.001 LDH(U/L) 531.00(432.25~633.25) 659.00(513.50~819.00) 780.00(480.75~1 268.75) χ2=39.743 <0.001 TC(mmol/L) 6.880(5.770~8.520) 7.460(6.200~10.425) 7.000(6.268~9.540) χ2=2.885 0.236 TG(mmol/L) 12.635(10.770~21.683) 11.860(11.850~24.975) 13.910(8.503~27.740) χ2=0.669 0.716 AMY(U/L) 196.00(90.75~358.00) 292.00(140.50~440.00) 411.00(190.00~607.50) χ2=17.024 <0.001 LIP(U/L) 1 161.5(434.0~3 641.0) 922.0(554.0~3 109.5) 2 283.0(1 016.0~5 589.0) χ2=9.880 0.007 CRP(mg/L) 89.00(45.00~136.00) 136.00(79.75~273.75) 154.50(90.00~255.50) χ2=28.317 <0.001 表 3 三组患者评分系统和疾病转归及预后比较
Table 3. Comparison of scoring systems, disease outcome, and prognosis among the three groups of patients
指标 MAP(n=199) MSAP(n=48) SAP(n=53) χ2值 P值 PASS评分 90.0(90.0~90.0) 140.0(115.0~140.0) 200.0(152.5~220.0) 219.351 <0.001 Ranson评分 1(1~2) 2(2~2) 2(2~2) 83.084 <0.001 HAPS评分 1(1~1) 1(1~1) 1(0~1) 0.480 0.799 APACHE-Ⅱ评分 1(1~1) 1(1~2) 2(1~2) 43.388 <0.001 BISAP评分 0(0~0) 0(0~0) 0(0~1) 50.785 <0.001 住院天数(d) 7.00(4.00~9.00) 11.00(8.00~14.50) 10.00(6.25~15.75) 48.281 <0.001 住院费用(元) 10 713(7 200~17 224) 17 027(11 800~24 020) 31 189(21 395~47 700) 93.894 <0.001 ICU[例(%)] 0(0.0) 0(0.0) 6(11.3) 17.317 <0.001 死亡[例(%)] 0(0.0) 0(0.0) 1(1.9) 3.662 0.338 复发[例(%)] 91(45.7) 14(29.2) 36(67.9) 11.357 0.003 表 4 五种评分系统对HTGAP患者病情严重程度、并发症和死亡的评估准确性比较
Table 4. Comparison of the accuracy of the five scoring systems in evaluating patients' severity of disease, complications, and mortality
评分系统及预后指标 AUC P值 敏感度 特异度 阳性预测值 阳性似然比 约登指数 APACHE-Ⅱ MSAP、SAP 0.744 <0.001 0.636 0.743 0.712 2.472 0.379 胸腔积液 0.704 0.016 0.683 0.350 0.678 2.105 0.350 死亡 0.990 <0.001 1.000 0.990 0.990 97.333 0.990 BISAP MSAP、SAP 0.687 <0.001 0.418 0.949 0.892 8.259 0.368 胸腔积液 0.919 <0.001 0.917 0.911 0.912 10.303 0.828 死亡 0.995 <0.001 1.000 0.993 0.993 146.000 0.993 PASS MSAP、SAP 0.963 <0.001 0.945 0.869 0.878 7.288 0.815 胸腔积液 0.846 <0.001 0.917 0.705 0.756 3.103 0.621 死亡 0.991 <0.001 1.000 0.983 0.983 58.400 0.983 Ranson MSAP、SAP 0.819 <0.001 0.655 0.899 0.866 6.464 0.553 胸腔积液 0.916 <0.001 0.917 0.826 0.840 5.257 0.742 死亡 0.995 <0.001 1.000 0.990 0.990 97.333 0.990 HAPS MSAP、SAP 0.418 0.619 0.745 0.211 0.486 0.945 -0.044 胸腔积液 0.442 0.512 0.512 0.217 0.460 0.852 -0.016 死亡 0.110 <0.001 0.000 0.219 0.000 0.000 -0.781 -
[1] HE WH, ZHU Y. Diagnosis and lipid-lowering treatment strategy for hypertriglyceridemic pancreatitis[J]. Chin J Pancreatol, 2022, 22(4): 241-246. DOI: 10.3760/cma.j.cn115667-20220711-00098.何文华, 祝荫. 高三酰甘油血症性胰腺炎的诊断和降脂治疗策略[J]. 中华胰腺病杂志, 2022, 22(4): 241-246. DOI: 10.3760/cma.j.cn115667-20220711-00098. [2] SU W, GUO F. Triglyceride-controlling during acute phase of hypertriglyceridemia induced pancreatitis[J]. Chin J Dig Surg, 2023, 22(1): 89-93. DOI: 10.3760/cma.j.cn115610-20221220-00755.苏伟, 郭丰. 高甘油三酯血症性胰腺炎急性期的血脂控制[J]. 中华消化外科杂志, 2023, 22(1): 89-93. DOI: 10.3760/cma.j.cn115610-20221220-00755. [3] DU YQ, SONG YX. Characteristics and treatment of hypertriglyceridemia acute pancreatitis[J]. Chin J Pract Int Med, 2021, 41(1): 10-13. DOI: 10.19538/j.nk2021010103.杜奕奇, 宋英晓. 高三酰甘油血症急性胰腺炎的特点与处理[J]. 中国实用内科杂志, 2021, 41(1): 10-13. DOI: 10.19538/j.nk2021010103. [4] Pancreas Study Group, Chinese Society of Gastroenterology, Chinese Medical Association, Editorial Board of Chinese Journal of Pancreatology, Editorial Board of Chinese Journal of Digestion. Chinese guidelines for the management of acute pancreatitis (Shenyang, 2019)[J]. J Clin Hepatol, 2019, 35(12): 2706-2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013.中华医学会消化病学分会胰腺疾病学组, 《中华胰腺病杂志》编委会, 《中华消化杂志》编委会. 中国急性胰腺炎诊治指南(2019年, 沈阳)[J]. 临床肝胆病杂志, 2019, 35(12): 2706-2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013. [5] WU BU, JOHANNES RS, SUN X, et al. The early prediction of mortality in acute pancreatitis: a large population-based study[J]. Gut, 2008, 57(12): 1698-1703. DOI: 10.1136/gut.2008.152702. [6] TANG YF, TANG GD, LIANG ZH, et al. Clinical features of severe acute hypertriglyceridemic pancreatitis[J]. J Clin Hepatol, 2019, 35(4): 830-834. DOI: 10.3969/j.issn.1001-5256.2019.04.024.唐永凤, 唐国都, 梁志海, 等. 重症高甘油三酯性急性胰腺炎的临床特征分析[J]. 临床肝胆病杂志, 2019, 35(4): 830-834. DOI: 10.3969/j.issn.1001-5256.2019.04.024. [7] ZHAO HJ, WU D, WU WM, et al. Research advances of hyperlipidemic pancreatitis[J]. Med J Pumch, 2022, 13(4): 637-643. DOI: 10.12290/xhyxzz.2021-0760.赵慧佳, 吴东, 吴文铭, 等. 高脂血症性胰腺炎研究进展[J]. 协和医学杂志, 2022, 13(4): 637-643. DOI: 10.12290/xhyxzz.2021-0760. [8] CHEN HZ, JI L, LI L, et al. Early prediction of infected pancreatic necrosis secondary to necrotizing pancreatitis[J]. Medicine (Baltimore), 2017, 96(30): e7487. DOI: 10.1097/MD.0000000000007487. [9] WU BU, BATECH M, QUEZADA M, et al. Dynamic measurement of disease activity in acute pancreatitis: the pancreatitis activity scoringsystem[J]. Am J Gastroenterol, 2017, 112(7): 1144-1152. DOI: 10.1038/ajg.2017.114. [10] BUXBAUM J, QUEZADA M, CHONG B, et al. The Pancreatitis Activity Scoring System predicts clinical outcomes in acute pancreatitis: findings from a prospective cohort study[J]. Am J Gastroenterol, 2018, 113(5): 755-764. DOI: 10.1038/s41395-018-0048-1. [11] YU Z, NI Q, ZHANG P, et al. Clinical utility of the pancreatitis activity scoring system in severe acute pancreatitis[J]. Front Physiol, 2022, 13: 935329. DOI: 10.3389/fphys.2022.935329. [12] ONG Y, SHELAT VG. Ranson score to stratify severity in acute pancreatitis remains valid-old is gold[J]. Expert Rev Gastroenterol Hepatol, 2021, 15(8): 865-877. DOI: 10.1080/17474124.2021.1924058. [13] MIKÓ A, VIGH É, MÁTRAI P, et al. Computed tomography severity index vs. other indices in the prediction of severity and mortality in acute pancreatitis: A predictive accuracy meta-analysis[J]. Front Physiol, 2019, 10: 1002. DOI: 10.3389/fphys.2019.01002. [14] HE WH, ZHENG X, ZHU Y, et al. To study the early prediction method of acute pancreatitis severity and infectious pancreatic necrosis based on acute pancreatitis database[J]. Chin J Pancreatol, 2019, 19(3): 172- 176. DOI: 10.3760/cma.j.issn.1674-1935.2019.03.004.何文华, 郑西, 祝荫, 等. 基于大样本数据库比较APACHEⅡ、Ranson、BISAP和CTSI评分在早期预测急性胰腺炎病情严重程度的价值[J]. 中华胰腺病杂志, 2019, 19(3): 172-176. DOI: 10.3760/cma.j.issn.1674-1935.2019.03.004. [15] HAN T, CHENG T, LIAO Y, et al. Thrombo-inflammatory prognostic scores improve bisap-based risk stratification in acute pancreatitis patients: A retrospective cohort study[J]. J Inflamm Res, 2022, 15: 3323-3335. DOI: 10.2147/JIR.S366246. [16] VALVERDE-LÓPEZ F, MATAS-COBOS AM, ALEGRÍA-MOTTE C, et al. BISAP, RANSON, lactate and others biomarkers in prediction of severe acute pancreatitis in a European cohort[J]. J Gastroenterol Hepatol, 2017, 32(9): 1649-1656. DOI: 10.1111/jgh.13763. [17] GAO W, YANG HX, MA CE. The value of BISAP score for predicting mortality and severity in acute pancreatitis: A systematic review and meta-analysis[J]. PLoS One, 2015, 10(6): e0130412. DOI: 10.1371/journal.pone.0130412. [18] LUO XP, WANG J, WU Q, et al. Research advances in acute pancreatitis scoring system[J]. J Clin Hepatol, 2022, 38(9): 2188-2192. DOI: 10.3969/j.issn.1001-5256.2022.09.046.罗秀平, 王洁, 吴青, 等. 急性胰腺炎评分系统的研究进展[J]. 临床肝胆病杂志, 2022, 38(9): 2188-2192. DOI: 10.3969/j.issn.1001-5256.2022.09.046. [19] MA XH, LI L, JIN T, et al. Harmless acute pancreatitis score on admission can accurately predict mild acute pancreatitis[J]. J South Med Univ, 2020, 40(2): 190-195. DOI: 10.12122/j.issn.1673-4254.2020.02.09.马小华, 李兰, 金涛, 等. 入院时无害性急性胰腺炎评分可预测轻症急性胰腺炎[J]. 南方医科大学学报, 2020, 40(2): 190-195. DOI: 10.12122/j.issn.1673-4254.2020.02.09. -




 PDF下载 ( 2228 KB)
PDF下载 ( 2228 KB)

 下载:
下载:

 下载:
下载: