原位肝移植术后胆道并发症发生的影响因素分析
DOI: 10.3969/j.issn.1001-5256.2023.07.017
Analysis of influencing factors on biliary complications after orthotopic liver transplantation
-
摘要:
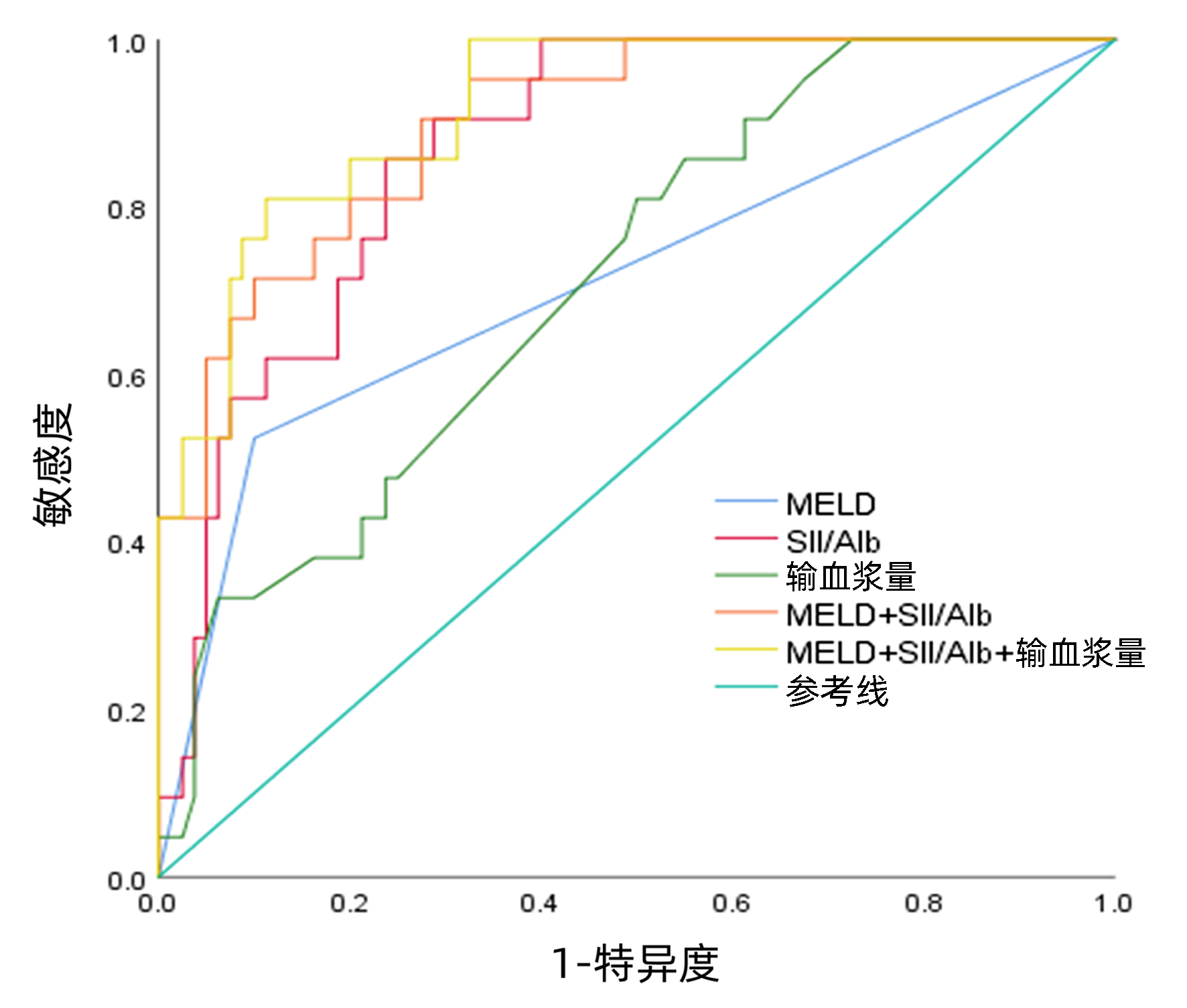
目的 分析原位肝移植术后胆道并发症相关的血清学指标、手术指标, 探究其影响因素及预测指标。 方法 回顾性收集武汉大学人民医院2016年1月-2022年6月101例行原位肝移植患者的临床资料。根据患者术后6个月是否出现胆道并发症, 分为胆道并发症组(BC组, n=21)和非胆道并发症组(非BC组, n=80)。计量资料两组间比较采用成组t检验或Mann-Whitney U检验, 计数资料两组间比较使用χ2检验。单因素与多因素分析采用Logistic回归分析, 并以受试者工作特征曲线(ROC曲线)评估联合指标的预测效能。 结果 101例患者中21例(20.8%)发生胆道并发症。Logistc多因素分析结果显示, MELD评分(OR=0.134, 95%CI: 0.031~0.590, P=0.008)、全身炎症反应指数(SⅡ)/Alb (OR=1.415, 95%CI: 1.181~1.696, P=0.001)、输入血浆量(OR=1.001, 95%CI: 1.000~1.002, P=0.032)是肝移植患者术后发生胆道并发症的独立影响因素。MELD评分、SⅡ/Alb、输入血浆量、MELD+SⅡ/Alb、MELD+SⅡ/Alb+输入血浆量预测肝移植术后胆道并发症的ROC曲线下面积(AUC)分别为0.712、0.870、0.712、0.900、0.918。 结论 SⅡ/Alb、输入血浆量及MELD评分是肝移植术后胆道并发症发生的影响因素, 三者联合具有较好的预测价值和临床指导意义。 Abstract:Objective To analyze the serological markers and surgical indicators associated with biliary complications after orthotopic liver transplantation, explore their influencing factors and predictive indicators. Methods A retrospective analysis was performed for the clinical data of 101 patients who underwent orthotopic liver transplantation in Renmin Hospital of Wuhan University from January 2016 to June 2022, according to the presence or absence of biliary complication (BC) at 6 months after surgery, they were divided into BC group with 21 patients and non-BC group with 80 patients.The t-test or the Mann-Whitney U test was used for comparison of continuous data between groups, and the chi-square test was used for comparison of categorical data between groups.Univariate and multivariate Logistic regression analyses were performed, and the receiver operating characteristic (ROC) curve was used to evaluate the predictive performance of combined indicators. Results Among the 101 patients, 21(20.8%) experienced BC.The multivariate Logistic regression analysis showed that MELD score (odds ratio[OR]=0.134, 95% confidence interval[CI]: 0.031-0.590, P=0.008), SⅡ/Alb (OR=1.415, 95%CI: 1.181-1.696, P=0.001), and plasma transfusion volume (OR=1.001, 95%CI: 1.000-1.002, P=0.032) were independent risk factors for the development of BC in patients after liver transplantation.MELD score, SⅡ/Alb, plasma transfusion volume, MELD+SⅡ/Alb, and MELD+SⅡ/Alb+plasma transfusion volume had an area under the ROC curve of 0.712, 0.870, 0.712, 0.900, and 0.918, respectively, in predicting BC after liver transplantation. Conclusion SⅡ/Alb, plasma transfusion volume and MELD score are independent risk fators for BC after liver transplantation.The combination of three indicators has good predictive value and clinical guiding significance for BC after liver transplantation. -
表 1 原位肝移植患者术后胆道并发症的单因素分析
Table 1. Univariate analysis of BC after orthotopic liver transplantation
变量 BC组(n=21) 非BC组(n=80) 统计值 P值 年龄(岁) 49.0±9.3 50.5±10.7 t=0.593 0.554 性别(男/女, 例) 19/2 67/13 χ2=0.595 0.440 原发病(例) 肝炎肝硬化(是/否) 15/6 51/29 χ2=0.433 0.510 肝恶性肿瘤(是/否) 9/12 45/35 χ2=1.199 0.273 合并症(例) 高血压(是/否) 3/18 16/64 χ2=0.356 0.551 糖尿病(是/否) 5/16 17/63 χ2=0.064 0.800 血管并发症(是/否) 6/15 12/68 χ2=2.092 0.148 胆管吻合方式[例(%)] χ2=0.276 0.599 端端吻合 19(90.5) 75(93.8) 胆肠吻合 2(9.5) 5(6.2) Child-Pugh分级[例(%)] χ2=1.381 0.240 A级 8(38.1) 42(52.5) ≥B级 13(61.9) 38(47.5) MELD评分[例(%)] χ2=16.073 0.001 >18分 10(47.6) 8(10.0) ≤18分 11(52.4) 72(90.0) ALBI评分 -2.02(-2.44~-1.40) -2.36(-2.85~-1.83) Z=-2.368 0.018 ALT(U/L) 34.0(22.5~48.0) 30.5(20.0~48.0) Z=-0.452 0.651 AST(U/L) 43.0(27.0~82.5) 39.5(28.3~69.0) Z=-0.511 0.610 TBil(μmol/L) 49.61(12.23~163.05) 26.09(14.46~55.96) Z=-1.029 0.303 Alb(g/L) 36.0±3.6 39.4±5.7 t=0.664 0.011 PT(s) 14.0(12.2~19.3) 13.8(11.6~15.7) Z=-1.080 0.280 ALP(U/L) 112.16(93.10~126.55) 104.1(83.85~125.25) Z=-1.134 0.257 GGT(U/L) 72.0(39.5~123.0) 60.5(23.3~129.0) Z=-0.439 0.660 SCr(μmol/L) 70.0(60.0~100.5) 64.0(55.0~78.8) Z=-1.532 0.125 GPR 0.43(0.28~0.92) 0.46(0.17~1.01) Z=-0.238 0.811 NLR 4.20(3.21~5.24) 2.82(2.12~3.84) Z=-3.933 0.001 SⅡ/Alb 14.77(12.39~18.09) 9.09(7.46~11.81) Z=-5.197 0.001 手术时长(min) 9.5(8.8~11.0) 9.0(8.0~10.0) Z=-2.377 0.017 术中出血量(mL) 3600(2350~5250) 2650(1525~3475) Z=-2.685 0.007 输入红细胞(U) 16(9~22) 10(8~16) Z=-2.359 0.018 输血浆量(mL) 2000(1950~3025) 1875(1000~2075) Z=-3.016 0.003 无肝期(min) 65(50~70) 57(45~65) Z=-1.387 0.165 表 2 原位肝移植患者术后胆道并发症的多因素分析
Table 2. Multivariate analysis of BC after orthotopic liver transplantation
变量 β值 SE Wald/χ2 OR 95%CI P值 MELD评分(>18分vs≤18分) -2.009 0.756 7.068 0.134 0.031~0.590 0.008 S Ⅱ /Alb(≥14.5 vs<14.5) 0.347 0.092 14.147 1.415 1.181~1.696 0.001 输入血浆量(>4 000 mL vs≤4 000 mL) 0.001 0.000 4.604 1.001 1.000~1.002 0.032 表 3 各指标对肝移植术后胆道并发症的预测性能
Table 3. Prediction of different index for BC after liver transplantation
指标 AUC SE 95%CI P值 敏感度 特异度 约登指数 MELD评分 0.712 0.071 0.572~0.852 0.003 - - - SⅡ/Alb 0.870 0.036 0.798~0.941 0.001 0.857 0.763 0.620 输入血浆量 0.712 0.059 0.598~0.827 0.003 0.810 0.500 0.310 MELD+SⅡ/Alb 0.900 0.034 0.833~0.967 0.001 0.905 0.725 0.630 MELD+S Ⅱ /Alb+输入血浆量 0.918 0.029 0.861~0.976 0.001 0.810 0.888 0.697 -
[1] SAMUEL D, COILLY A. Management of patients with liver diseases on the waiting list for transplantation: A major impact to the success of liver transplantation[J]. BMC Med, 2018, 16(1): 113. DOI: 10.1186/s12916-018-1110-y. [2] BERTACCO A, BARBIERI S, GUASTALLA G, et al. Risk factors for mortality in liver transplant patients[J]. Transplant Proc, 2019, 51 (1): 179-183. DOI: 10.1016/j.transproceed.2018.06.025 [3] AKAMATSU N, SUGAWARA Y, HASHIMOTO D. Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: A systematic review of the incidence, risk factors and outcome[J]. Transpl Int, 2011, 24(4): 379-392. DOI: 10.1111/j.1432-2277.2010.01202.x. [4] FORDE JJ, BHAMIDIMARRI KR. Management of biliary complications in liver transplant recipients[J]. Clin Liver Dis, 2022, 26(1): 81-99. DOI: 10.1016/j.cld.2021.08.008. [5] HU XW, LI T. Diagnosis and treatment of common biliary complications after orthotopic liver transplantation in adults[J]. Organ Transplant, 2022, 13(5): 569-576. DOI: 10.3969/j.issn.1674-7445.2022.05.004.胡鑫文, 李亭. 成人原位肝移植术后常见胆道并发症的诊疗[J]. 器官移植, 2022, 13(5): 569-576. DOI: 10.3969/j.issn.1674-7445.2022.05.004. [6] KOCHHAR G, PARUNGAO JM, HANOUNEH IA, et al. Biliary complications following liver transplantation[J]. World J Gastroenterol, 2013, 19(19): 2841-2846. DOI: 10.3748/wjg.v19.i19.2841. [7] TRAN LT, CARULLO PC, BANH DPT, et al. Pediatric liver transplantation: Then and now[J]. J Cardiothorac Vasc Anesth, 2020, 34(8): 2028-2035. DOI: 10.1053/j.jvca.2020.02.019. [8] GREIF F, BRONSTHER OL, VAN THIEL DH, et al. The incidence, timing, and management of biliary tract complications after orthotopic liver transplantation[J]. Ann Surg, 1994, 219(1): 40-45. DOI: 10.1097/00000658-199401000-00007. [9] TAI Q, HE XS, YANG JA, et al. The diagnosis and treatment of biliary complications in liver transplant patients[J]. Chin J Gen Surg, 2010, 25(12): 969-972. DOI: 10.3760/cma.j.issn.1007-631X.2010.12.010.邰强, 何晓顺, 杨建安, 等. 肝移植术后胆道并发症的诊断与治疗[J]. 中华普通外科杂志, 2010, 25(12): 969-972. DOI: 10.3760/cma.j.issn.1007-631X.2010.12.010. [10] FANG C, YAN S, ZHENG SS. Influencing factors, diagnosis and treatment of biliary complications after liver transplantation[J]. Chin J Gen Surg, 2014, 29(6): 486-488. DOI: 10.3760/cma.j.issn.1007-631X.2014.06.028.方程, 严盛, 郑树森. 肝移植术后胆道并发症的影响因素及诊治进展[J]. 中华普通外科杂志, 2014, 29(6): 486-488. DOI: 10.3760/cma.j.issn.1007-631X.2014.06.028. [11] KALTENBORN A, GUTCKE A, GWIASDA J, et al. Biliary complications following liver transplantation: Single-center experience over three decades and recent risk factors[J]. World J Hepatol, 2017, 9(3): 147-154. DOI: 10.4254/wjh.v9.i3.147. [12] SARHAN MD, OSMAN AMA, MOHAMED MA, et al. Biliary complications in recipients of living-donor liver transplant: A single-center review of 120 patients[J]. Exp Clin Transplant, 2017, 15(6): 648-657. DOI: 10.6002/ect.2016.0210. [13] WIEDERKEHR JC, IGREJA MR, NOGARA MS, et al. Analysis of survival after primary liver transplantation: Multivariate analysis of 155 cases in a single center[J]. Transplant Proc, 2010, 42(2): 511-512. DOI: 10.1016/j.transproceed.2010.01.014. [14] GIRARD E, RISSE O, ABBA J, et al. Internal biliary stenting in liver transplantation[J]. Langenbecks Arch Surg, 2018, 403(4): 487-494. DOI: 10.1007/s00423-018-1669-y. [15] YOON JU, BYEON GJ, PARK JY, et al. Bloodless living donor liver transplantation: Risk factors, outcomes, and diagnostic predictors[J]. Medicine, 2018, 97(50): e13581. DOI: 10.1097/MD.0000000000013581. [16] JACOB M, COPLEY LP, LEWSEY JD, et al. Pretransplant MELD score and post liver transplantation survival in the UK and Ireland[J]. Liver Transpl, 2004, 10(7): 903-907. DOI: 10.1002/lt.20169. [17] ODEN-BRUNSON H, MCDONALD MF, GODFREY E, et al. Is liver transplant justified at any MELD score?[J]. Transplantation, 2023, 107(3): 680-692. DOI: 10.1097/tp.0000000000004345. [18] LIU CC. Real-world study on SⅡ/ALB ratio to predict the efficacy of immune checkpoint inhibitors in the treatment of malignant tumors[D]. Dalian: Dalian Medical University, 2021.刘成成. SⅡ/ALB比值预测免疫检查点抑制剂治疗恶性肿瘤疗效真实世界研究[D]. 大连: 大连医科大学, 2021. [19] LI HW, WANG GC, ZHANG HH, et al. Prognostic role of the systemic immune-inflammation index in brain metastases from lung adenocarcinoma with different EGFR mutations[J]. Genes Immun, 2019, 20(6): 455-461. DOI: 10.1038/s41435-018-0050-z. [20] AN R, QIN C, WU Q, et al. Predictive value of systemic immune inflammation index (SⅡ)in the short-term prognosis of patients with dilated cardiomyopathy[J]. Clin J Med Offic, 2022, 50(11): 1129-1133. DOI: 10.16680/j.1671-3826.2022.11.07.安然, 秦璨, 武琼, 等. 全身免疫炎症指数对扩张型心肌病患者预后预测价值[J]. 临床军医杂志, 2022, 50(11): 1129-1133. DOI: 10.16680/j.1671-3826.2022.11.07. [21] REN A, LI ZQ, CHENG PR, et al. Systemic immune-inflammation index is a prognostic predictor in patients with intrahepatic cholangiocarcinoma undergoing liver transplantation[J]. Mediators Inflamm, 2021, 2021: 6656996. DOI: 10.1155/2021/6656996. [22] FU HY, ZHENG J, CAI JY, et al. Systemic immune-inflammation index (SⅡ) is useful to predict survival outcomes in patients after liver transplantation for hepatocellular carcinoma within Hangzhou criteria[J]. Cell Physiol Biochem, 2018, 47(1): 293-301. DOI: 10.1159/000489807. [23] LICHTENEGGER P, SCHIEFER J, GRAF A, et al. The association of pre-operative anaemia with survival after orthotopic liver transplantation[J]. Anaesthesia, 2020, 75(4): 472-478. DOI: 10.1111/anae.14918. [24] JÓŹWIK A, KARPETA E, NITA M, et al. Impact of blood loss and intraoperative blood transfusion during liver transplantation on the incidence of early biliary complications and mortality[J]. Transplant Proc, 2020, 52(8): 2477-2479. DOI: 10.1016/j.transproceed.2020.03.052. [25] CHU HH, KIM JH, SHIM JH, et al. Neutrophil-to-lymphocyte ratio as a biomarker predicting overall survival after chemoembolization for intermediate-stage hepatocellular carcinoma[J]. Cancers (Basel), 2021, 13(11): 2830. DOI: 10.3390/cancers13112830. [26] NYLEC M, DERBISZ K, CHRZ SZCZ P, et al. Preoperative neutrophil-to-lymphocyte ratio as an independent predictor of 1-year graft loss and mortality after orthotopic LiverTransplantation[J]. Transplant Proc, 2020, 52(8): 2472-2476. DOI: 10.1016/j.transproceed.2020.03.036. [27] KWON HM, MOON YJ, JUNG KW, et al. Neutrophil-to-lymphocyte ratio is a predictor of early graft dysfunction following living donor liver transplantation[J]. Liver Int, 2019, 39(8): 1545-1556. DOI: 10.1111/liv.14103. [28] LUÉ A, SOLANAS E, BAPTISTA P, et al. How important is donor age in liver transplantation?[J]. World J Gastroenterol, 2016, 22(21): 4966-4976. DOI: 10.3748/wjg.v22.i21.4966. [29] ZHANG QB, SHEN CH, TAO YF, et al. Risk factor analysis and classified therapeutic strategies for biliary complications after liver transplantation from organ donation by citizens after death: A report of 48 cases at a single center[J]. Chin J Organ Transplant, 2020, 41(10): 623-628. DOI: 10.3760/cma.j.cn421203-20191115-00415.张全保, 沈丛欢, 陶一峰, 等. 肝移植术后胆道并发症的危险因素分析及分类治疗策略[J]. 中华器官移植杂志, 2020, 41(10): 623-628. DOI: 10.3760/cma.j.cn421203-20191115-00415. -



 PDF下载 ( 1878 KB)
PDF下载 ( 1878 KB)

 下载:
下载:


